Exam Code: Health Cloud Accredited Professional
Exam Name: Health Cloud Accredited Professional
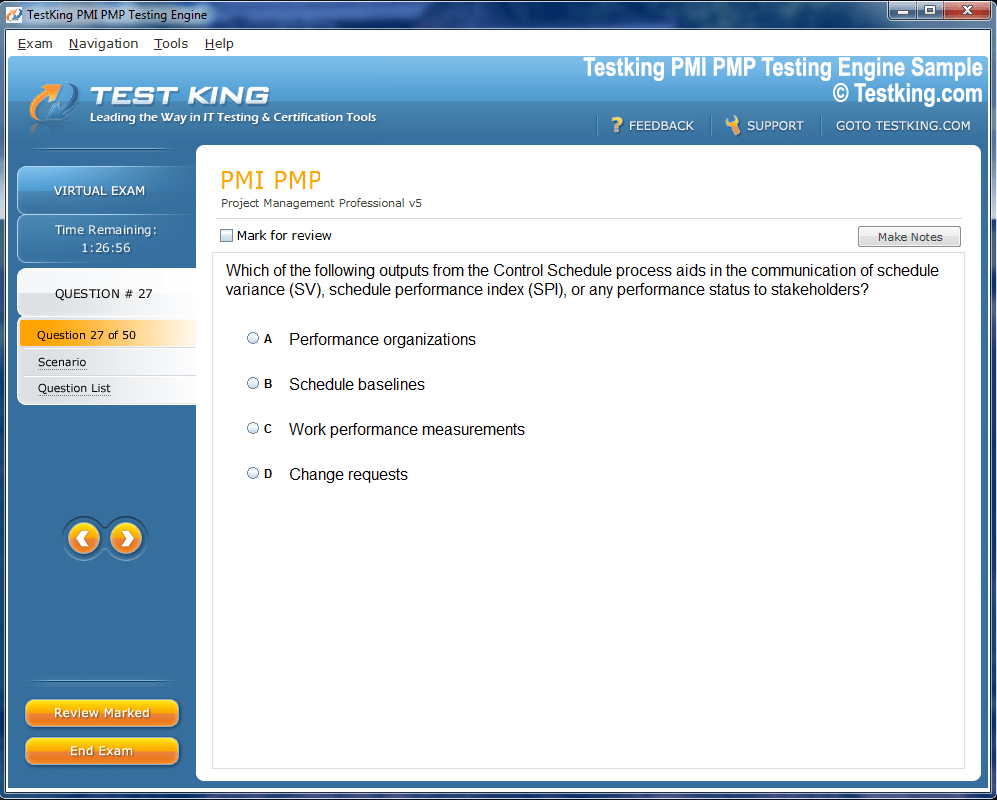
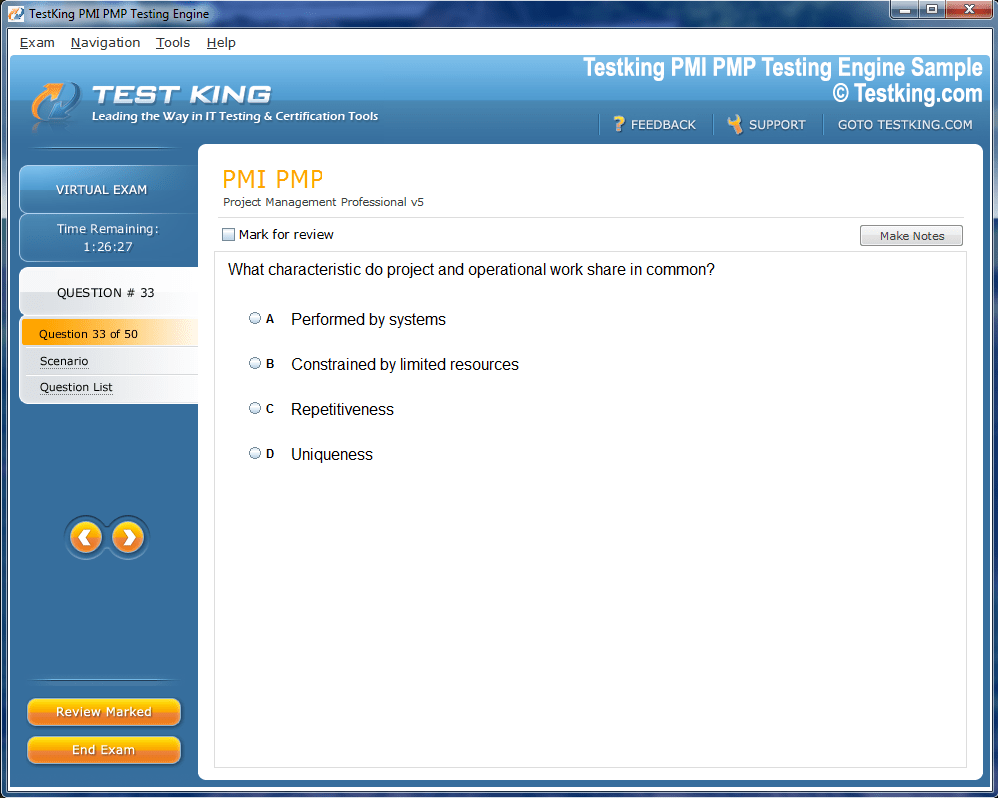
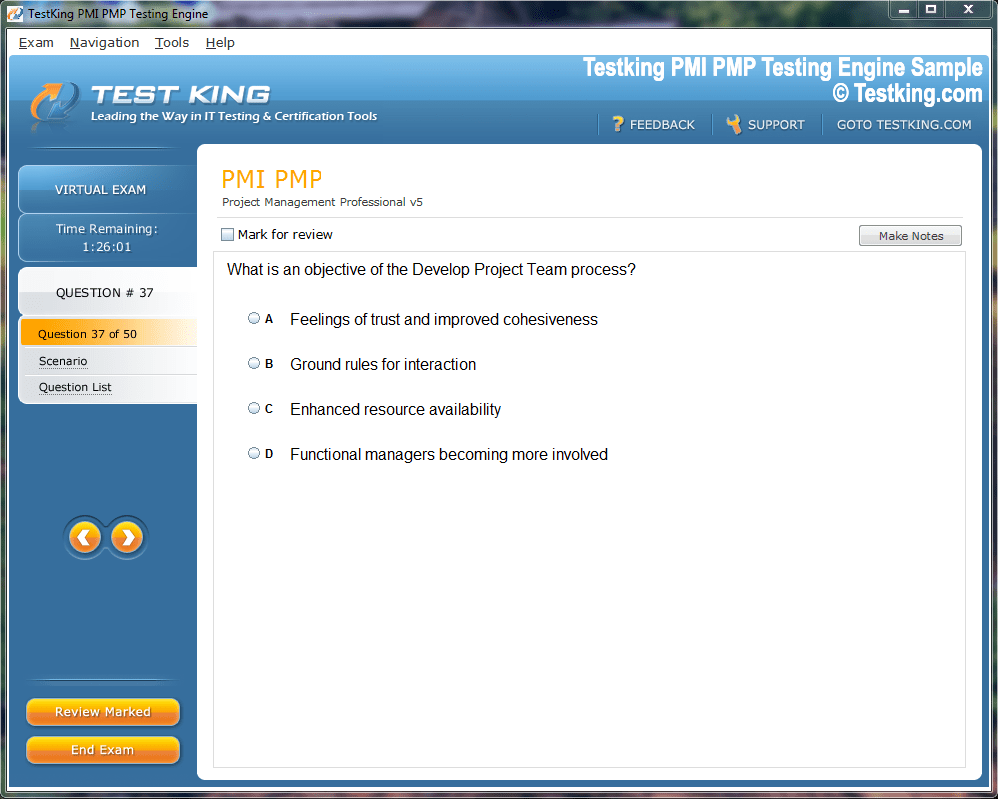
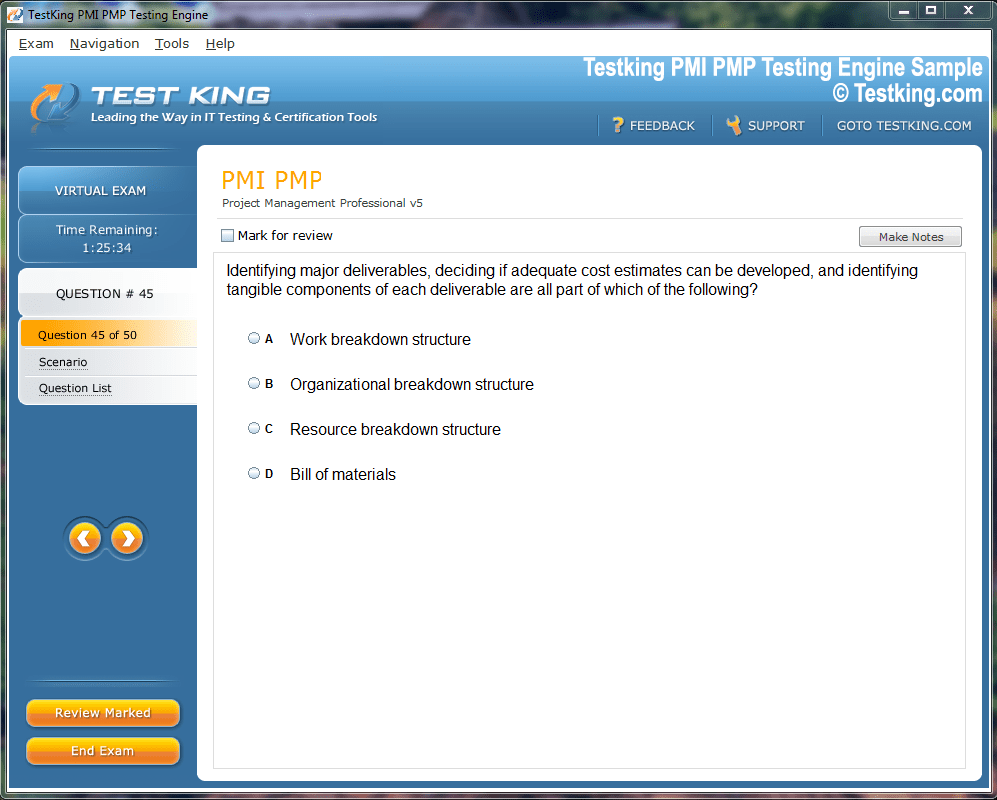
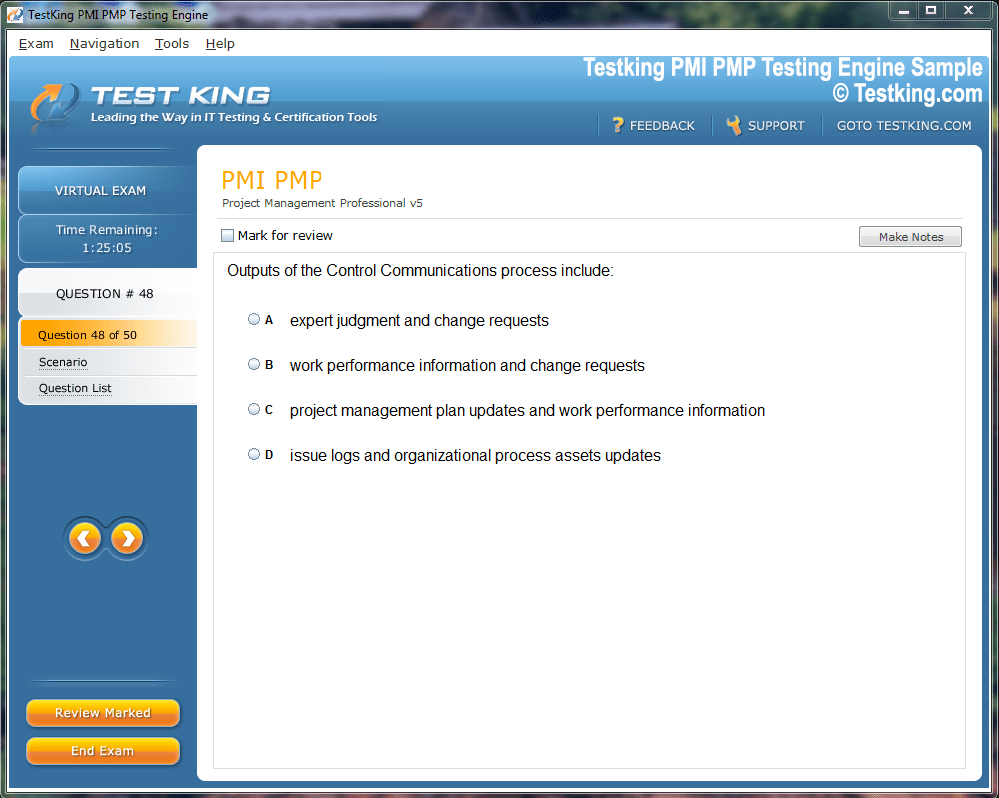
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our Health Cloud Accredited Professional testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Top Salesforce Exams
- Certified Agentforce Specialist - Certified Agentforce Specialist
- Certified Data Cloud Consultant - Certified Data Cloud Consultant
- Certified Integration Architect - Certified Integration Architect
- Certified Service Cloud Consultant - Salesforce Certified Service Cloud Consultant
- Certified Development Lifecycle and Deployment Architect - Certified Development Lifecycle and Deployment Architect
- Certified Platform App Builder - Certified Platform App Builder
- Certified Sharing and Visibility Architect - Certified Sharing and Visibility Architect
- Certified Platform Developer II - Certified Platform Developer II
- Certified Data Architect - Certified Data Architect
- ADM-201 - Administration Essentials for New Admins
- Certified Business Analyst - Certified Business Analyst
- Certified Platform Developer - Certified Platform Developer
- Certified MuleSoft Developer I - Certified MuleSoft Developer I
- Certified Marketing Cloud Administrator - Certified Marketing Cloud Administrator
- Certified Experience Cloud Consultant - Certified Experience Cloud Consultant
- CRT-450 - Salesforce Certified Platform Developer I
- Certified Marketing Cloud Email Specialist - Certified Marketing Cloud Email Specialist
- Certified Sales Cloud Consultant - Certified Sales Cloud Consultant
- Certified Advanced Administrator - Certified Advanced Administrator
- Certified Identity and Access Management Designer - Certified Identity and Access Management Designer
- Health Cloud Accredited Professional - Health Cloud Accredited Professional
- Field Service Lightning Consultant - Field Service Lightning Consultant
- Certified Tableau Data Analyst - Certified Tableau Data Analyst
- Certified Marketing Cloud Consultant - Certified Marketing Cloud Consultant
- Certified OmniStudio Consultant - Certified OmniStudio Consultant
- Certified Tableau Desktop Foundations - Certified Tableau Desktop Foundations
- Certified User Experience Designer - Certified User Experience Designer
- Certified Tableau CRM and Einstein Discovery Consultant - Certified Tableau CRM and Einstein Discovery Consultant
- Certified AI Specialist - Certified AI Specialist
- Public Sector Solutions Accredited Professional - Public Sector Solutions Accredited Professional
- Financial Services Cloud Accredited Professional - Financial Services Cloud Accredited Professional
- Certified Marketing Cloud Account Engagement Specialist - Certified Marketing Cloud Account Engagement Specialist
- Certified Sharing and Visibility Designer - Certified Sharing and Visibility Designer
- Certified MuleSoft Integration Architect I - Salesforce Certified MuleSoft Integration Architect I
- Certified Education Cloud Consultant - Certified Education Cloud Consultant
- Certified Platform Administrator II - Certified Platform Administrator II
- Field Service Consultant - Field Service Consultant
- CRM Analytics and Einstein Discovery Consultant - Certified CRM Analytics and Einstein Discovery Consultant
- Certified Associate - Certified Associate
- Certified AI Associate - Certified AI Associate
Navigating Data Models and Care Programs in Salesforce Health Cloud Accredited
The Salesforce Health Cloud Accredited Professional exam is meticulously designed to evaluate an individual’s comprehensive understanding of the Health Cloud platform, including its nuances, underlying architecture, and functional capabilities. Candidates who undertake this exam are expected to possess a profound knowledge of Health Cloud terminology, an understanding of its various modules, and the ability to troubleshoot or remediate fundamental issues that may arise within the platform. This examination serves as a benchmark for proficiency, measuring not only theoretical knowledge but also the aptitude to apply platform features in practical scenarios, thereby bridging the gap between comprehension and operational execution.
The exam consists of 60 multiple-choice and multiple-select questions, carefully constructed to assess a candidate’s holistic grasp of Health Cloud functionalities. Candidates are allotted 75 minutes to complete the assessment, requiring efficient time management, analytical thinking, and decisiveness in selecting the correct responses. Achieving a passing score necessitates correctly answering 65 percent of the questions, which equates to 39 correct responses. The exam fee is set at 150 USD, with applicable taxes, and retake fees mirror the original cost. No prerequisites are required, making the assessment accessible to professionals with varied backgrounds, although prior practical exposure to Salesforce Health Cloud can significantly enhance performance.
Exam Structure and Core Components
The structure of the Health Cloud Accredited Professional exam is designed to align closely with real-world implementation scenarios. It is categorized into four principal domains: discovery, design, implementation, and deployment. Each domain is weighted based on its relative importance in practical application, ensuring that candidates are evaluated on both conceptual understanding and applied proficiency.
Discovery
The discovery phase represents approximately 11 percent of the exam and emphasizes the foundational stage of any Health Cloud implementation. Candidates must demonstrate the ability to translate customer use cases into actionable insights by identifying personas and stakeholders, ensuring that all relevant parties are considered in the design and deployment processes. This involves not merely listing roles but comprehending how each stakeholder interacts with the platform, the data flows they generate, and the implications of their engagement on overall system functionality.
An essential aspect of discovery is the elicitation of requirements, both functional and technical. Candidates are expected to gather detailed information regarding desired customer outcomes and map these to tangible Health Cloud capabilities. This requires analytical acuity, as requirements often exist in ambiguous or loosely defined forms. Successful candidates can discern underlying needs from stated requirements, anticipate potential challenges, and recommend features or workflows that align with organizational objectives.
Discovery also involves a strategic evaluation of customer expectations, ensuring that the intended outcomes are achievable within the framework of Health Cloud’s capabilities. This includes understanding regulatory and compliance constraints, particularly those affecting patient data and privacy, and integrating these considerations into the initial planning. By mastering the discovery phase, professionals can lay the groundwork for a seamless implementation that maximizes system utility while mitigating potential risks.
Design
The design phase constitutes the most substantial portion of the examination, accounting for approximately 42 percent of the total assessment. This segment evaluates the candidate’s ability to convert requirements gathered during discovery into a coherent and optimized solution within Health Cloud. A key aspect of design is determining how to model patients, providers, healthcare facilities, and other essential entities using the appropriate Health Cloud objects. This requires an intimate understanding of the underlying data structures, relationships, and best practices for object utilization.
Candidates must also be adept at creating solutions tailored to specific verticals within healthcare. For instance, designing a care program for chronic disease management differs significantly from designing an insurance utilization workflow. Each scenario demands a unique configuration of Health Cloud modules, data models, and security settings to ensure both compliance and operational efficiency.
Design considerations extend to data migration, integration, and reporting. Professionals are expected to devise strategies that preserve data integrity while facilitating seamless migration from legacy systems to Health Cloud. This includes understanding the sequence of data loads, dependencies between objects, and the reconciliation of historical records with new structures. Furthermore, candidates should be capable of defining key performance indicators (KPIs) and configuring Salesforce to monitor these metrics, providing insights that inform decision-making and continuous improvement.
Security and compliance are critical design elements. Candidates must understand how to configure organizational security settings, sharing rules, and access controls to safeguard sensitive patient information. They should also be able to integrate external systems, such as electronic health records or appointment management platforms, in a manner that maintains data fidelity while supporting business objectives. By the conclusion of the design phase, the candidate should have a robust blueprint that balances operational requirements with compliance, performance, and scalability considerations.
Discovery and Design Synergy
While the discovery and design phases are assessed separately, they are deeply interconnected in practical implementation. Discovery informs design, providing the context, constraints, and requirements necessary to build a functional solution. Conversely, design decisions may prompt a reevaluation of discovery findings, highlighting gaps in stakeholder analysis or technical requirements. Effective professionals navigate this interplay, maintaining a feedback loop that ensures the final design is both feasible and aligned with organizational priorities.
A salient component of design is understanding how to leverage Health Cloud best practices. These practices encompass everything from the optimal use of standard and custom objects to the integration of automated workflows, security protocols, and reporting mechanisms. Mastery of these best practices enables professionals to construct solutions that are not only functional but also maintainable, scalable, and aligned with Salesforce’s evolving platform features.
Implementation Overview
Although the implementation domain accounts for 42 percent of the exam, it is intrinsically linked to discovery and design. Candidates must demonstrate the ability to translate theoretical designs into operational configurations within Health Cloud. This involves installing packages, configuring application settings, setting up permission structures, and integrating external data sources. Candidates are also assessed on their ability to use Salesforce automation capabilities, including workflows, process builders, and OmniStudio components, to streamline operations and improve efficiency.
Security configuration is another vital component of implementation. Candidates should be able to establish sharing rules, define role hierarchies, and assign permissions to ensure that users can access the necessary data without compromising security or compliance. Reporting and analytics capabilities must also be configured to monitor operational metrics, track performance, and support decision-making. By effectively executing the implementation phase, professionals demonstrate their ability to operationalize Health Cloud solutions that meet organizational needs and stakeholder expectations.
Deployment Considerations
Deployment, though representing a smaller portion of the exam at 5 percent, is crucial for ensuring that the solution is functional and sustainable. Candidates must be capable of planning pre- and post-deployment activities, including system validation, user provisioning, and verification of permission sets. This phase also requires knowledge of testing strategies to confirm that all workflows, integrations, and data migrations perform as expected in a live environment.
User access and permissions are critical deployment elements. Professionals should ensure that appropriate permission set licenses are assigned to each user, enabling access to Health Cloud features relevant to their roles. This includes administrative users, care coordinators, patients, and external stakeholders, all of whom interact with the system in different ways. Properly managed deployments reduce the risk of errors, enhance user adoption, and contribute to the overall effectiveness of the Health Cloud solution.
Study Resources and Preparation
To prepare for the Salesforce Health Cloud Accredited Professional exam, candidates can utilize a combination of theoretical study and hands-on practice. Partner Learning Camp provides a structured curriculum and study materials, while practical exercises, such as the Health Cloud Specialist Superbadge, allow professionals to apply knowledge in realistic scenarios. Emphasis on both conceptual understanding and applied proficiency is essential, as the exam evaluates a candidate’s ability to integrate knowledge into actionable solutions.
Preparation strategies should include a detailed review of data models, care program configurations, provider management, and utilization management workflows. Candidates should also become familiar with integration mechanisms, including HL7 and FHIR standards, as well as automated workflows, reporting, and analytics features. By engaging in immersive study and practical exercises, candidates can develop the confidence and expertise necessary to succeed in the examination.
Essential Knowledge Areas
Candidates should focus on several critical domains of Health Cloud functionality. These include patient and household data models, clinical data structures, insurance and claims management, care program development, and social determinants of health. Understanding provider networks, utilization management, intelligent sales workflows, and appointment management are also key. Each domain encompasses unique objects, workflows, and configuration strategies that must be mastered to ensure comprehensive competency.
Understanding the interplay between data models and real-world healthcare operations is particularly valuable. For instance, the utilization management module allows insurers to evaluate requests for medical services, while the care program module enables proactive patient engagement. Mastery of these modules requires both theoretical knowledge and practical experience, as candidates must understand not only the object structures but also the business processes they support.
Strategic Insights
The Salesforce Health Cloud Accredited Professional exam is not simply a test of memorization. It assesses the ability to apply strategic thinking to platform configuration, stakeholder engagement, and data management. Candidates who approach the exam with a holistic understanding of healthcare workflows, regulatory compliance, and system integration are more likely to succeed. Strategic insights, such as anticipating potential workflow bottlenecks, designing scalable data models, and configuring automation to enhance efficiency, differentiate proficient professionals from those with limited practical exposure.
Furthermore, the exam evaluates problem-solving skills in realistic scenarios. Candidates may be presented with incomplete information, conflicting requirements, or complex integration challenges, requiring them to reason critically and propose effective solutions. Success in these scenarios reflects not only technical knowledge but also analytical agility, decision-making acumen, and the ability to navigate complexity—essential skills for any Health Cloud professional.
Implementation of Salesforce Health Cloud Solutions
The implementation phase within Salesforce Health Cloud encompasses the intricate process of transforming meticulously designed plans into operational systems. This phase requires not only technical acumen but also the ability to interpret designs in a manner that preserves their integrity while ensuring operational efficiency. Professionals embarking on this stage are tasked with translating solution designs into fully functional configurations, encompassing the installation of Health Cloud packages, configuration of applications, integration with external systems, and establishment of security protocols that align with regulatory requirements.
Installation and Configuration
The initial step in implementation is the installation of the Health Cloud managed package, a process contingent upon pre-existing organizational settings. For instance, enabling the Contacts to Multiple Accounts feature is a prerequisite, as it facilitates shared contact management, which is central to patient and provider data structures. Post-installation, the organization must undergo configuration to establish system readiness. This involves setting up My Domain to ensure a unique Salesforce domain, deploying it to users, and assigning default record types, page layouts, and permission sets to system administrators. These preparatory steps are crucial to prevent misconfigurations that could impede functionality or user adoption.
Following installation, administrators configure Health Cloud profiles, permission sets, and roles to manage diverse user types effectively. These roles span system administrators, internal Salesforce users, care coordinators, patients, and community members. Configuring the Health Cloud console is another essential task, enabling customization of key components to reflect organizational workflows. This customization ensures that dashboards, lists, and patient records are displayed according to operational priorities, enhancing user experience and minimizing navigation friction.
Data Migration and Management
An integral component of implementation is the migration of patient data from legacy systems into Health Cloud. The patient creation process employs two mechanisms: a job flow that establishes patient records and a mapping group that transfers data from candidate objects to active patient objects. Configuring these processes allows administrators to control how records are created, mapped, and validated, ensuring accuracy, referential integrity, and compliance with data governance policies. Furthermore, migrating historical data requires careful sequencing of operations to maintain relationships among patients, providers, and care programs, preventing data fragmentation or duplication.
Data management also encompasses the establishment of healthcare-specific objects and their relationships. The design of care plans, provider networks, utilization management records, and insurance claims must be operationalized in a manner that supports ongoing workflows. Each object requires configuration of fields, relationships, validation rules, and automation to ensure seamless operation within the Health Cloud ecosystem. This level of granularity ensures that healthcare professionals and administrators can access reliable, actionable information, facilitating improved patient outcomes and streamlined operational processes.
Security and Access Control
Security within Health Cloud is paramount, given the sensitivity of healthcare data. Implementation mandates meticulous configuration of sharing rules, role hierarchies, and permission sets to align with regulatory standards such as HIPAA and GDPR. Professionals must ensure that each user receives access commensurate with their responsibilities, preventing unauthorized exposure of protected health information. Permission Set Licenses, including Health Cloud PSL and Health Cloud Platform PSL, must be allocated to users to enable appropriate platform functionalities. Optional assignments, such as the Analytics Platform PSL, support advanced reporting and predictive analytics.
Establishing role hierarchies ensures that supervisory roles, such as care coordinators or administrative staff, can access subordinate records while maintaining compliance with confidentiality protocols. Sharing rules and visibility settings enable nuanced control over patient data, allowing selective access for providers, insurance representatives, and other stakeholders. These security configurations require both technical understanding and an appreciation of healthcare workflows, as misalignment can compromise both compliance and operational efficiency.
Integration with External Systems
A critical facet of Health Cloud implementation is integrating with external healthcare systems, particularly electronic health records, appointment management platforms, and insurance databases. Integration strategies leverage standard APIs, HL7 v2 interfaces, and FHIR R4 protocols, enabling real-time data exchange and operational synchronization. For instance, patient demographics, clinical records, and insurance claims can be imported into Health Cloud, ensuring a consolidated view of patient interactions and care history.
Integration requires thoughtful planning, as disparate systems often use varied data models and formats. Professionals must map source fields to Health Cloud objects, implement error-handling protocols, and schedule data updates to maintain system consistency. Middleware solutions can bridge compatibility gaps, translating FHIR or HL7 messages into formats consumable by Health Cloud, enabling seamless interoperability without disrupting ongoing clinical operations. The ability to integrate effectively enhances data fidelity, accelerates decision-making, and supports coordinated care across multiple stakeholders.
Automation and Process Optimization
Health Cloud implementation emphasizes automation to streamline routine processes, reduce manual intervention, and enhance accuracy. Automation spans workflows, process builders, and OmniStudio components, allowing care coordinators, administrators, and providers to execute repetitive tasks efficiently. For example, preauthorization requests, service evaluations, and concurrent reviews can be automated based on predefined rules, ensuring compliance with clinical policies and regulatory standards.
The utilization of OmniStudio components facilitates advanced process automation, enabling complex questionnaire paths, care assessments, and dynamic interactions with patients. Automated notifications, follow-up reminders, and adherence alerts can be configured to improve patient engagement and ensure continuity of care. By leveraging these automation capabilities, Health Cloud reduces administrative overhead, enhances operational agility, and provides a robust foundation for intelligent decision-making.
Care Plans and Program Implementation
Care plans and care programs represent operational manifestations of strategic healthcare objectives within Health Cloud. Implementing care plans involves defining problems, goals, tasks, and care teams. Problems denote specific clinical or nonclinical health issues that require attention, while goals establish measurable outcomes for addressing these issues. Tasks represent actionable steps toward goal attainment, providing clear directives for patients and care teams. Care teams consist of professionals and stakeholders collaborating to deliver integrated care, ensuring that patient support networks are both comprehensive and coordinated.
Care program implementation extends this concept by providing structured interventions and educational resources to support patient health proactively. Programs can deliver medication adherence guidance, resource allocation, financial assistance, and predictive analytics through Einstein Analytics to anticipate risks. Configuring these programs requires attention to workflow sequencing, data capture, and automated notifications, ensuring that interventions are timely, accurate, and personalized to patient needs.
Provider Management and Relationship Configuration
Effective provider management is fundamental to Health Cloud’s operational efficiency. Implementation involves establishing provider networks, configuring relationship cards, and mapping practitioner affiliations to facilities. Provider cards on account pages display associated practitioners, while relationship cards on contact pages reveal hospital or clinic affiliations. This dual-view configuration allows administrators and care coordinators to access comprehensive provider information, facilitating referrals, appointments, and coordination of care.
Provider data must be synchronized across multiple records, and automation mechanisms must maintain up-to-date information in searchable fields. The CareProviderSearchableField object serves as a central repository, ensuring rapid and accurate provider searches. This functionality supports operational efficiency, enabling care teams to identify suitable providers quickly, schedule appointments effectively, and manage patient interactions with minimal friction.
Utilization Management Implementation
Implementing utilization management within Health Cloud enables insurers and care organizations to streamline authorization processes and ensure appropriate care delivery. Health Cloud provides objects for reviewing and evaluating medical requests, enabling clinicians, administrators, and medical directors to monitor adherence to policy, escalate critical cases, and approve or deny requests efficiently. The system automates decision-making where feasible, reducing manual intervention, improving SLA compliance, and enhancing cost-effectiveness.
Implementation involves assigning the Health Cloud Utilization Management permission set to users, configuring guided workflows, and establishing escalation paths. Processes may include drug requests, service authorizations, admissions, concurrent reviews, appeals, and grievance handling. Properly configured utilization management enhances transparency, facilitates interdepartmental collaboration, and ensures that patients receive timely, medically appropriate services.
Intelligent Sales and Appointment Configuration
Health Cloud extends beyond clinical operations to support intelligent sales and operational workflows. Med tech and healthcare product sales teams benefit from features that provide visibility into surgical case management, inventory tracking, and contract execution. Implementation requires assigning appropriate permission sets to enable access to ActionPlans, Health Cloud Foundation, and Industry Visits, facilitating operational readiness.
Appointment management integration allows Health Cloud to synchronize with external scheduling systems, delivering a unified booking experience for call center agents and care coordinators. Implementing this functionality involves configuring appointment objects, mapping source systems, and ensuring that data flows between Health Cloud and electronic health records are consistent. This integration enhances operational efficiency, reduces scheduling errors, and improves patient satisfaction through timely and accurate appointment management.
Reporting and Analytics Setup
An essential aspect of Health Cloud implementation is configuring reporting and analytics capabilities to monitor operational performance and inform strategic decisions. Salesforce provides mechanisms to define KPIs, generate reports, and visualize trends across patient populations, care programs, and utilization management workflows. Implementation involves configuring dashboards, defining metrics, and ensuring that reporting aligns with business objectives.
Advanced analytics may incorporate predictive models to identify at-risk patients, anticipate resource requirements, or forecast revenue streams. These insights enable care teams and administrators to allocate resources effectively, optimize workflows, and enhance patient outcomes. Implementation of these capabilities requires both technical configuration and a strategic understanding of healthcare operations to ensure that the data captured is actionable and meaningful.
Deployment and Operational Management in Salesforce Health Cloud
Deployment within Salesforce Health Cloud marks the transition from a configured system to a fully operational platform. Though deployment represents a smaller portion of professional accreditation exams, it is critical for ensuring that the designed and implemented solutions function seamlessly in real-world environments. Successful deployment integrates technical configuration with workflow validation, user readiness, and compliance assurance, ensuring the system delivers value immediately upon go-live.
Pre-Deployment Planning
Effective deployment begins with meticulous pre-deployment planning. Administrators must evaluate system readiness, verifying that all configuration elements, data migrations, and security settings are aligned with organizational objectives. This process includes validating workflows, automation processes, and integration endpoints to prevent operational disruptions. Planning also encompasses defining the deployment sequence, prioritizing tasks, and establishing rollback procedures in case unforeseen errors arise. Proactive planning mitigates risks, ensuring that end-users experience minimal disruption and that data integrity is maintained throughout the deployment.
Pre-deployment considerations also involve ensuring that all permission set licenses are appropriately assigned. Each user type—ranging from system administrators and care coordinators to patients and external stakeholders—requires access aligned with their roles. Proper license allocation ensures that users can execute necessary operations without encountering access errors or functionality gaps, while maintaining adherence to security protocols.
Post-Deployment Validation
Following deployment, post-deployment validation ensures that configured processes, integrations, and data flows operate as intended. This phase includes thorough testing of automated workflows, confirmation of role-based access permissions, and verification of reporting capabilities. Any discrepancies identified during this validation must be remediated promptly to maintain system integrity. Post-deployment monitoring also involves evaluating system performance under operational loads, ensuring that automation processes and integrations scale effectively without degradation in speed or accuracy.
User onboarding and training are integral components of post-deployment activities. While Health Cloud provides a user-friendly interface, different roles interact with the system in unique ways. Training ensures that care coordinators can manage patient interactions efficiently, administrators can oversee configurations and reports, and clinicians or providers can access and update patient records accurately. A structured onboarding process fosters rapid adoption and reduces the likelihood of operational errors.
Permission Structures and Access Control
A robust deployment strategy relies on well-defined permission structures. Health Cloud requires a nuanced approach to access control, balancing operational needs with regulatory compliance. Permission set licenses, including Health Cloud PSL and Health Cloud Platform PSL, form the foundation of user access. These licenses enable platform functionalities while allowing administrators to assign additional granular permissions tailored to specific user roles.
Roles and profiles are configured to reflect organizational hierarchies, ensuring that supervisors can access subordinate records, care coordinators can manage patient workflows, and external stakeholders receive restricted, relevant access. Sharing rules and visibility settings refine access further, enabling conditional data exposure based on defined criteria. Properly configured permission structures protect sensitive information while facilitating efficient workflow execution, supporting both compliance and operational efficiency.
Remote Patient Monitoring
Remote monitoring capabilities within Health Cloud enable care coordinators to track patient health metrics outside traditional clinical environments. Implementation of these capabilities involves configuring code sets, units of measure, and care metric targets that reflect individual patient requirements. Care observations, such as vital signs or adherence metrics, are displayed within patient accounts, providing a centralized view for care teams. Dashboards and visualizations allow rapid identification of anomalies or at-risk patients, enabling proactive interventions.
Remote monitoring integrations also leverage connected devices, capturing real-time data that informs care decisions. Alerts and automated notifications can be configured to trigger when patient metrics fall outside defined thresholds, supporting timely interventions and mitigating potential health risks. Effective deployment of remote monitoring enhances patient engagement, reduces emergency visits, and supports continuity of care, aligning with broader healthcare objectives.
Risk Score Management
Health Cloud enables the calculation and recalibration of patient risk scores, providing insight into individual and population-level health risks. Using batch Apex jobs, risk scores are recalculated based on patient data updates, with configurations ensuring that only relevant records are processed. Risk scores can inform care prioritization, resource allocation, and intervention strategies, offering predictive analytics that support clinical decision-making.
Deployment requires careful configuration of scheduled jobs, data access permissions, and notification mechanisms to ensure that risk scores remain accurate and actionable. By integrating risk management into daily workflows, care teams can anticipate potential health complications, tailor interventions, and improve patient outcomes, while administrative teams gain actionable insights for strategic planning.
Provider Search and Network Optimization
A central component of operational management in Health Cloud is provider search, which allows care teams to locate suitable healthcare providers based on criteria such as location, specialty, or availability. Deployment involves configuring the CareProviderSearchableField object, which consolidates data from contacts, accounts, healthcare provider records, and practitioner facilities into a searchable repository. Automation ensures that updates to source records are synchronized, maintaining data fidelity and search efficiency.
Provider network management extends beyond search, encompassing relationship mapping, affiliation tracking, and network optimization. Relationship cards on account and contact pages provide contextual information about practitioner associations with facilities, enabling care coordinators to identify referral opportunities, coordinate treatments, and ensure patients receive care in appropriate settings. This comprehensive provider management framework supports operational efficiency, enhances patient satisfaction, and facilitates coordinated care delivery.
Utilization Management Operations
Utilization management in Health Cloud enables healthcare organizations and payers to ensure appropriate, cost-effective care delivery. Deployment involves configuring guided workflows, escalation paths, and automated decision rules for preauthorization requests, service approvals, and concurrent reviews. Health Cloud provides a centralized platform for agents, clinicians, and medical directors to review, evaluate, and approve care requests, reducing manual intervention and improving SLA compliance.
Permission sets must be assigned to users involved in utilization management to enable access to relevant workflows and reporting tools. Deploying these processes ensures transparency, enhances operational efficiency, and reduces the risk of inappropriate or delayed care. By standardizing utilization workflows, organizations can maintain regulatory compliance, optimize resource allocation, and improve overall patient outcomes.
Intelligent Sales Deployment
Health Cloud also supports operational deployment for med tech and healthcare sales teams through intelligent sales configurations. Deployment involves assigning permission sets that enable access to ActionPlans, Health Cloud Foundation, and Industry Visits functionalities. These configurations allow sales teams to manage surgical case visits, monitor inventory, and execute orders effectively.
Sales operations benefit from features such as serial inventory tracking, mobile access to case details, and automated documentation of sales activities. By deploying these tools within Health Cloud, organizations enhance operational efficiency, ensure accurate product availability, and support field sales representatives in executing strategic objectives. The integration of operational and clinical data provides a unified view of patient care and associated supply chain considerations.
Appointment Management Deployment
Appointment management integration in Health Cloud facilitates coordinated scheduling across multiple systems. Deployment involves configuring appointment objects, mapping data from external scheduling systems, and establishing automated workflows for reminders, confirmations, and rescheduling. This functionality ensures that patients and care coordinators have access to accurate, real-time scheduling information, improving service delivery and reducing administrative burden.
By integrating appointment management into Health Cloud, organizations create a seamless experience for both patients and providers. Automated workflows reduce missed appointments, enhance operational efficiency, and enable proactive communication with patients, fostering engagement and satisfaction.
Reporting and Analytics Deployment
Reporting and analytics deployment in Health Cloud transforms operational data into actionable insights. Dashboards, KPI tracking, and customized reports provide visibility into patient populations, care program efficacy, utilization metrics, and operational performance. During deployment, administrators configure these tools to reflect organizational priorities, ensuring that stakeholders receive relevant and timely information.
Advanced deployment configurations may include predictive analytics, enabling organizations to anticipate patient risks, optimize resource allocation, and forecast operational needs. By deploying these capabilities effectively, care teams, administrators, and executives gain a comprehensive understanding of performance trends, enabling data-driven decision-making and strategic planning.
Continuous Operational Governance
Deployment is not the endpoint of Health Cloud operations; continuous governance ensures system efficacy, compliance, and adaptability. Post-deployment monitoring includes auditing data integrity, verifying automation processes, and evaluating user adherence to workflows. Feedback loops enable administrators to identify inefficiencies, implement corrective actions, and refine system configurations in response to evolving operational requirements.
Governance also extends to security and compliance monitoring. Regular reviews of access permissions, sharing rules, and role hierarchies ensure that data exposure remains appropriate and that regulatory obligations are met. Continuous operational oversight safeguards patient data, maintains trust among stakeholders, and enhances the long-term sustainability of Health Cloud implementations.
Integration of Advanced Functionalities
Deployment may also incorporate advanced functionalities such as care assessments, predictive risk modeling, and personalized care plan tracking. Configuring these features requires attention to detail, ensuring that assessments are properly linked to patient records, workflows are optimized for operational efficiency, and results are actionable. Health Cloud’s modular architecture allows organizations to integrate these functionalities gradually, aligning deployment with strategic priorities and operational readiness.
Advanced deployment also involves ensuring interoperability with external systems, including electronic health records, insurance platforms, and connected devices. Effective integration enhances data completeness, supports coordinated care, and enables real-time decision-making, aligning operational capabilities with patient-centric objectives.
Data Models and Care Program Configuration in Salesforce Health Cloud
Data models within Salesforce Health Cloud form the foundation upon which all patient-centric workflows, provider interactions, and healthcare operations are built. A deep understanding of these models is essential for professionals seeking to leverage the platform’s capabilities effectively. The architecture of Health Cloud allows for the representation of households, clinical data, insurance claims, care programs, and social determinants of health, ensuring that patient information is structured, interconnected, and actionable.
Household and Individual Data Models
The household data model enables the representation of patients and their family or household relationships. This model allows care teams to understand familial contexts that may impact patient health, such as shared genetic conditions, living arrangements, or support systems. Accurate household modeling is crucial for care coordination, preventive interventions, and patient engagement strategies.
The individual data model focuses on patients or members as primary entities, capturing demographic information, medical histories, and personalized care requirements. Salesforce recommends the Person Account Model for new implementations, as it combines account and contact information into a single record, simplifying management and reducing data redundancy. Implementing this model ensures streamlined workflows, improved data integrity, and enhanced reporting capabilities.
Clinical Data Model
The clinical data model organizes medical information, including diagnoses, lab results, medications, and care encounters. This model supports care plan development, risk assessment, and clinical decision-making. Health Cloud enables the integration of clinical data with external electronic health record systems through HL7 or FHIR protocols, ensuring a comprehensive and up-to-date view of patient health. By structuring clinical data effectively, organizations can monitor treatment outcomes, identify trends, and deliver personalized care interventions.
Insurance and Claims Data Models
Insurance and claims data models support payer organizations in managing health plan interactions, coverage verification, and claim adjudication. These models encompass insurance policies, provider networks, claim submissions, and approval workflows. Effective configuration of these models allows healthcare administrators to automate utilization management, monitor policy adherence, and ensure timely reimbursement. By integrating claims data with clinical and patient information, organizations achieve a holistic perspective on care delivery and financial performance.
Care Program and Management Data Models
Care programs represent structured interventions designed to improve patient health outcomes. Health Cloud allows administrators to create and configure care programs that track patient participation, adherence, and progress. These programs can encompass educational content, medication management, follow-up procedures, and financial assistance, providing a comprehensive support system for patients.
Care program management requires careful configuration of workflows, tasks, and team assignments. Each care program is associated with specific objectives and metrics, enabling administrators to monitor effectiveness and adjust interventions as needed. By leveraging care programs, organizations can proactively manage patient health, improve adherence, and optimize resource allocation.
Social Determinants of Health
Health Cloud incorporates social determinants of health data to capture nonclinical factors that influence patient well-being, such as socioeconomic status, living environment, and access to resources. Integrating this information into care workflows allows providers to tailor interventions, identify potential barriers to adherence, and implement holistic care strategies. Social determinants data enhances predictive modeling, risk assessment, and personalized care planning, enabling healthcare organizations to address both clinical and contextual factors affecting health outcomes.
Provider Data Model and Network Management
Provider data models allow healthcare organizations and insurers to manage provider networks, affiliations, and contractual agreements. Salesforce Health Cloud enables administrators to track relationships between practitioners and facilities, configure provider profiles, and manage contract terms. Provider relationship cards facilitate a clear view of connections between accounts and contacts, supporting referral management, scheduling, and network optimization.
Accurate provider modeling ensures that patients have access to appropriate care, care coordinators can navigate networks efficiently, and administrators can maintain compliance with network agreements and quality standards. This model also supports intelligent appointment management and ensures alignment between provider availability and patient needs.
Utilization Management Data Model
Utilization management (UM) is a critical process for payers and care organizations, enabling the evaluation of medical services, preauthorization requests, and clinical policies. Health Cloud provides objects and workflows to automate UM processes, including drug requests, service authorizations, concurrent reviews, and appeals. Implementing the UM data model allows organizations to standardize care evaluation, reduce administrative overhead, and ensure compliance with clinical policies and regulatory requirements.
By integrating UM workflows with provider and patient data, Health Cloud supports real-time decision-making, enhances transparency, and enables efficient escalation of complex cases. The combination of structured UM data with care programs and clinical information allows organizations to optimize resource allocation and improve patient outcomes.
Health Cloud Integration Standards
Health Cloud supports integration with external systems through HL7 v2 and FHIR R4 protocols, ensuring interoperability with electronic health records, appointment management platforms, and insurance databases. HL7 facilitates the transfer of clinical and administrative data between disparate systems, while FHIR provides a modern API framework for structured data exchange.
Deployment of integration strategies requires mapping source data to Health Cloud objects, configuring middleware as needed, and validating data accuracy. Integration ensures that patient records are comprehensive, real-time, and accessible to authorized users. This interoperability enhances operational efficiency, reduces manual entry errors, and supports coordinated care across multiple healthcare stakeholders.
Intelligent Sales and Appointment Management Workflows
Health Cloud extends operational capabilities beyond clinical care through intelligent sales and appointment management functionalities. Intelligent sales modules allow med tech and healthcare product teams to manage surgical case visits, track inventory, and execute orders effectively. Configuring these workflows involves assigning relevant permission sets, mapping sales data, and integrating with operational records.
Appointment management integration enables care coordinators and call center agents to schedule, reschedule, and confirm patient visits efficiently. This functionality ensures that multiple appointment sources are synchronized, reducing conflicts and improving patient engagement. Automation of reminders, notifications, and follow-up communications enhances adherence and operational efficiency.
Care Plan and Template Configuration
Care plans are central to patient management within Health Cloud, providing structured guidance for addressing clinical and nonclinical issues. Each care plan consists of a problem, goal, task, and care team. Problems represent prioritized health issues, goals establish desired outcomes, tasks outline actionable steps, and care teams coordinate the execution of interventions.
Administrators can create care plan templates to standardize workflows, reduce repetitive configuration, and ensure consistent quality across patient populations. Templates allow personalization for individual patients while maintaining operational efficiency, enhancing engagement, and promoting adherence. Care plans integrate with care programs, provider workflows, and utilization management processes to deliver comprehensive patient support.
Patient Assessments and Discovery Framework
Health Cloud provides assessment capabilities to gather patient information, identify risks, and tailor care plans. Using the Discovery Framework and OmniStudio, administrators can create dynamic assessments, such as screeners or questionnaires, that adapt to patient responses. Assessments can be administered by healthcare professionals in person, over the phone, or electronically through secure portals.
Configuring assessments requires mapping data to Health Cloud objects, establishing scoring and decision criteria, and integrating results into care plans. Automated notifications ensure that care teams are alerted to significant findings, enabling timely interventions. Assessments support population health initiatives, predictive analytics, and individualized care strategies, providing actionable insights for both clinical and administrative teams.
Risk Score and Predictive Analytics Integration
Risk scores provide quantifiable measures of patient health risks, allowing organizations to prioritize interventions and allocate resources effectively. Health Cloud enables recalculation of risk scores through scheduled batch processes, ensuring that updates reflect changes in patient conditions, care program participation, or clinical data.
Predictive analytics capabilities, such as Einstein Analytics, allow organizations to identify adherence risks, forecast patient needs, and optimize care program strategies. Deployment and configuration of predictive models involve defining metrics, mapping relevant data sources, and establishing thresholds for alerts and notifications. Integration of risk scores with care plans and utilization management processes ensures that interventions are proactive, personalized, and evidence-based.
Remote Monitoring and Telehealth Integration
Health Cloud supports remote monitoring of patient metrics through connected devices, enabling continuous tracking of vital signs, medication adherence, and lifestyle factors. Deployment involves defining care metric targets, establishing code sets and units of measure, and configuring dashboards for care coordinators to view real-time data.
Integration with telehealth platforms allows care teams to conduct virtual visits, review patient-generated data, and adjust care plans without requiring in-person consultations. Remote monitoring enhances patient engagement, supports chronic disease management, and enables timely interventions, contributing to improved outcomes and operational efficiency.
Advanced Operational Functionalities and Best Practices in Salesforce Health Cloud
Salesforce Health Cloud offers a sophisticated ecosystem of features that empower healthcare organizations to optimize clinical, administrative, and operational processes. Beyond basic implementation and deployment, advanced functionalities allow organizations to maximize efficiency, enhance patient engagement, and derive actionable insights from integrated data sources. Mastery of these advanced capabilities is essential for professionals seeking to excel in Health Cloud operations and to drive strategic outcomes for both patients and organizations.
Comprehensive Care Plan Management
Health Cloud’s care plan capabilities extend beyond simple task lists to encompass holistic patient management frameworks. Each care plan integrates multiple components: problems, goals, tasks, and care teams. Problems represent prioritized clinical or nonclinical health concerns, goals define measurable outcomes, tasks provide actionable steps toward achieving goals, and care teams coordinate execution across multiple stakeholders.
Advanced configuration of care plans includes automating task assignments, linking goals to clinical and social determinants data, and generating alerts for care team members when tasks require attention. Health Cloud enables care plan templates that standardize workflows while allowing customization for individual patients, ensuring that interventions are personalized yet efficient. Effective management of care plans improves adherence, enhances patient outcomes, and optimizes resource allocation across care teams.
Predictive Analytics and Risk Stratification
Predictive analytics within Health Cloud leverages integrated data from clinical, administrative, and social sources to anticipate patient needs, identify high-risk populations, and inform proactive interventions. Using Einstein Analytics and custom scoring models, organizations can calculate risk scores for individual patients and recalibrate them based on updated health metrics, care program participation, or social determinants of health.
Deployment of predictive analytics involves establishing data pipelines, mapping relevant sources, defining thresholds for alerts, and integrating predictive insights into care workflows. Risk stratification allows care teams to prioritize patients based on the likelihood of adverse events or nonadherence, ensuring that limited resources are directed toward those who require immediate attention. By integrating predictive insights with care plans and utilization management processes, organizations can enhance clinical decision-making and improve population health outcomes.
Utilization Management and Decision Automation
Advanced utilization management functionalities enable automated evaluation of medical service requests, preauthorization workflows, and concurrent reviews. Health Cloud provides objects and guided processes that streamline approvals, escalate complex cases, and facilitate transparent communication among payers, providers, and patients.
Automation reduces manual intervention, improves SLA compliance, and ensures that requests are processed efficiently. Integration of utilization management with provider networks, patient care plans, and claims data allows organizations to optimize decisions based on clinical guidelines, policy compliance, and historical utilization trends. By deploying decision automation strategically, healthcare organizations enhance operational efficiency, reduce administrative burden, and improve patient satisfaction.
Provider Network Optimization and Relationship Mapping
Health Cloud facilitates comprehensive management of provider networks through detailed relationship mapping and provider affiliation tracking. Provider cards and relationship cards provide insights into connections between practitioners, facilities, and patients. These tools allow administrators and care coordinators to identify referral pathways, optimize network coverage, and ensure that patients receive care from appropriate providers.
Advanced configuration includes maintaining real-time data synchronization, integrating provider availability with appointment management systems, and automating provider search functionalities based on specialty, location, and patient requirements. By optimizing provider networks, organizations improve patient access to care, reduce wait times, and enhance operational coordination.
Remote Monitoring and Telehealth Integration
Remote monitoring capabilities are integral to contemporary healthcare delivery models. Health Cloud enables care teams to capture patient-generated data from connected devices, including vital signs, medication adherence, and lifestyle metrics. Dashboards and visualizations allow care coordinators to monitor trends, identify anomalies, and intervene proactively.
Integration with telehealth platforms allows virtual consultations, real-time assessment reviews, and remote care plan adjustments. Implementation includes defining care metric targets, configuring notifications for deviations, and integrating data streams into patient records. These functionalities reduce hospital readmissions, improve chronic disease management, and enhance patient engagement by allowing care teams to maintain continuous oversight beyond traditional clinical settings.
Intelligent Sales and Field Operations
For med tech and healthcare product organizations, Health Cloud offers intelligent sales capabilities that optimize field operations, inventory management, and surgical case workflows. Deployment involves configuring ActionPlans, Health Cloud Foundation, and Industries Visits permission sets to provide sales representatives with actionable insights.
Advanced features include tracking surgical case visit details, real-time inventory visibility, automated e-signature order approvals, and optimized routing for field visits. Sales representatives can manage interactions efficiently, ensure the availability of products for procedures, and capture critical operational data. This integration of clinical, operational, and sales data enhances revenue optimization, field efficiency, and patient care support in procedure-based workflows.
Appointment Management and Operational Efficiency
Appointment management in Health Cloud integrates multiple scheduling sources to provide a seamless experience for patients, providers, and care coordinators. Administrators configure appointment objects, automate reminders, and synchronize external systems to prevent conflicts and enhance adherence.
Advanced workflows may include prioritization of urgent cases, automated rescheduling based on provider availability, and integration with care programs to ensure that patients receive necessary follow-ups. By centralizing appointment management and optimizing workflows, organizations improve patient satisfaction, reduce administrative burden, and enhance continuity of care.
Data Integration and Interoperability
A key strength of Health Cloud lies in its ability to integrate seamlessly with external systems, including electronic health records, claims platforms, and telehealth systems. Integration standards such as HL7 v2 and FHIR R4 facilitate the exchange of clinical and administrative data, ensuring that patient records are complete, current, and actionable.
Advanced integration strategies involve mapping source system fields to Health Cloud objects, configuring middleware where necessary, and establishing automated validation to ensure data accuracy. By maintaining interoperability, organizations support coordinated care, reduce data duplication, and enable real-time clinical decision-making.
Reporting, Dashboards, and Strategic Analytics
Health Cloud provides sophisticated reporting and dashboard capabilities that support strategic planning, operational oversight, and clinical decision-making. Administrators can configure custom dashboards to monitor care program effectiveness, utilization management metrics, risk stratification trends, and patient adherence.
Advanced analytics can include predictive modeling, trend forecasting, and KPI tracking aligned with organizational objectives. Integration of these insights into operational workflows ensures that care teams and administrators can act proactively, optimize resource allocation, and improve patient outcomes. Effective use of reporting and analytics transforms data into actionable intelligence, providing a foundation for continuous improvement.
Permission Sets, Security, and Compliance
Maintaining compliance with healthcare regulations is fundamental in Health Cloud deployments. Advanced security configurations involve establishing role hierarchies, sharing rules, and granular permission sets that control access to sensitive patient data. Health Cloud PSL and Platform PSL licenses provide baseline access, while additional permission sets enable functionality for specific workflows such as utilization management, care plan oversight, or analytics.
Regular audits of permission assignments, access patterns, and data visibility are essential to maintain compliance with HIPAA, GDPR, and organizational policies. By combining robust security practices with operational workflows, Health Cloud ensures that sensitive information remains protected while enabling authorized users to perform their duties effectively.
Best Practices for Health Cloud Professionals
Health Cloud professionals achieve operational excellence by adhering to several best practices. First, they maintain a holistic understanding of healthcare workflows, ensuring that technical configurations align with clinical, administrative, and operational objectives. Second, they leverage standardized templates, care plans, and automation to enhance efficiency and reduce errors.
Third, professionals prioritize integration and interoperability, ensuring that Health Cloud interacts seamlessly with external systems. Fourth, they monitor key metrics through dashboards, reports, and predictive analytics to drive data-informed decisions. Fifth, they maintain rigorous security and compliance oversight, aligning user access with role responsibilities and regulatory requirements.
Finally, ongoing professional development is essential. Health Cloud evolves continuously, introducing new features, integration capabilities, and operational modules. Staying abreast of platform updates, industry standards, and emerging healthcare trends allows professionals to leverage Health Cloud’s full potential and deliver measurable value to patients, providers, and organizations.
Strategic Integration of Patient-Centric Workflows
Health Cloud emphasizes patient-centered care, integrating workflows across clinical, operational, and administrative domains. Care programs, remote monitoring, risk stratification, and appointment management converge to create a unified patient experience. Advanced configuration ensures that care teams have real-time access to data, predictive insights, and actionable workflows.
Strategic integration also involves aligning patient engagement with organizational objectives, such as adherence improvement, cost reduction, and clinical outcome optimization. By harmonizing technology, data, and human resources, Health Cloud supports proactive, coordinated, and efficient healthcare delivery, establishing a foundation for sustainable patient-centered operations.
Conclusion
Salesforce Health Cloud provides a comprehensive, integrated platform that empowers healthcare organizations to streamline clinical, operational, and administrative workflows. From foundational concepts like data models, patient representation, and provider networks to advanced functionalities including predictive analytics, utilization management, remote monitoring, and intelligent sales, Health Cloud enables a holistic approach to patient-centered care. Its modular architecture, combined with robust integration standards such as HL7 and FHIR, ensures interoperability with electronic health records, appointment systems, and insurance platforms. Professionals leveraging the platform can optimize care programs, enhance patient engagement, and make data-driven decisions while maintaining compliance and security. By mastering implementation, deployment, and advanced operational capabilities, Health Cloud users can improve care outcomes, increase organizational efficiency, and deliver personalized interventions. Ultimately, the platform serves as a strategic tool for transforming healthcare delivery, aligning technology with clinical objectives, and fostering continuous improvement across the entire care ecosystem.