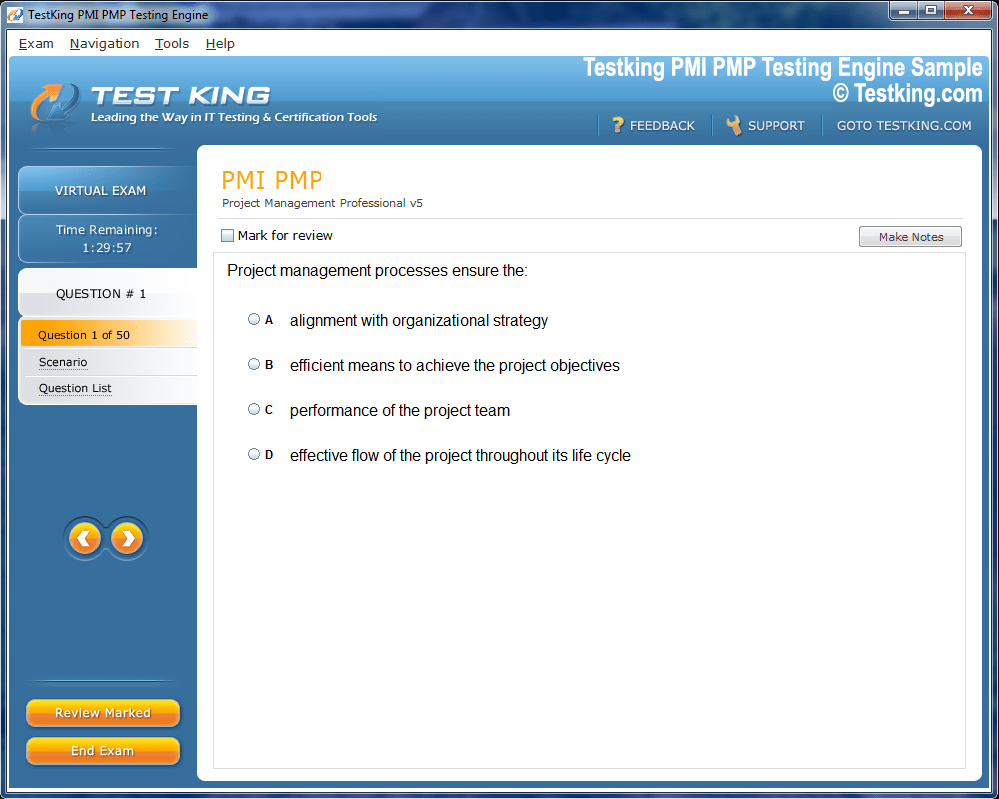
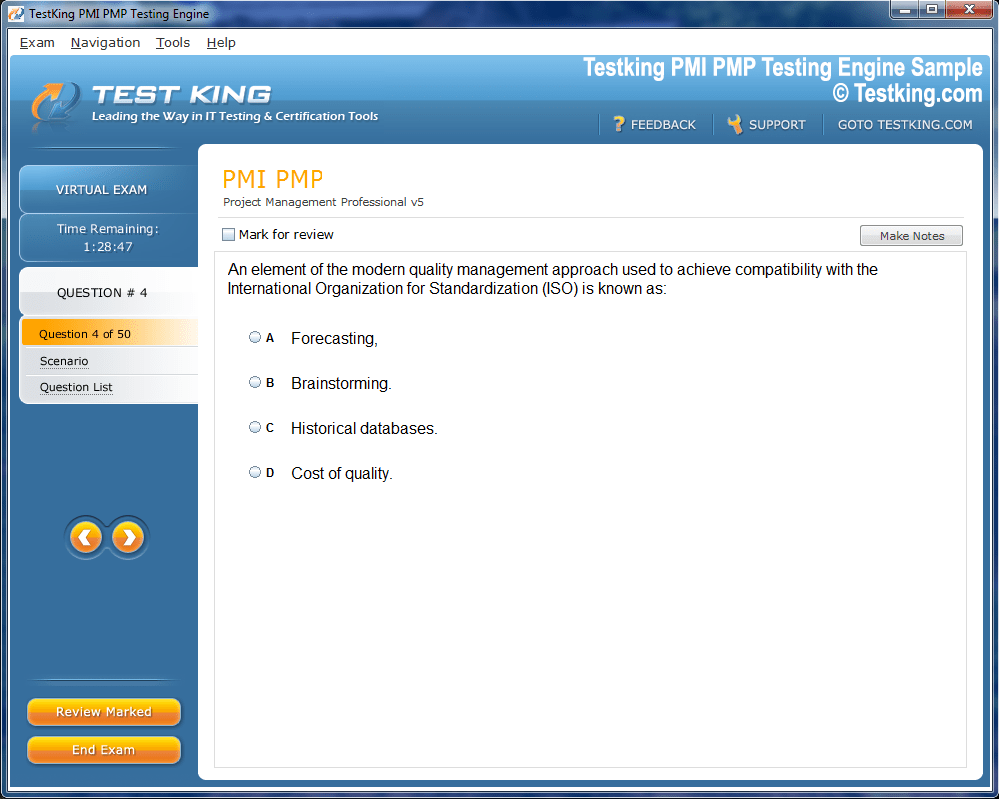
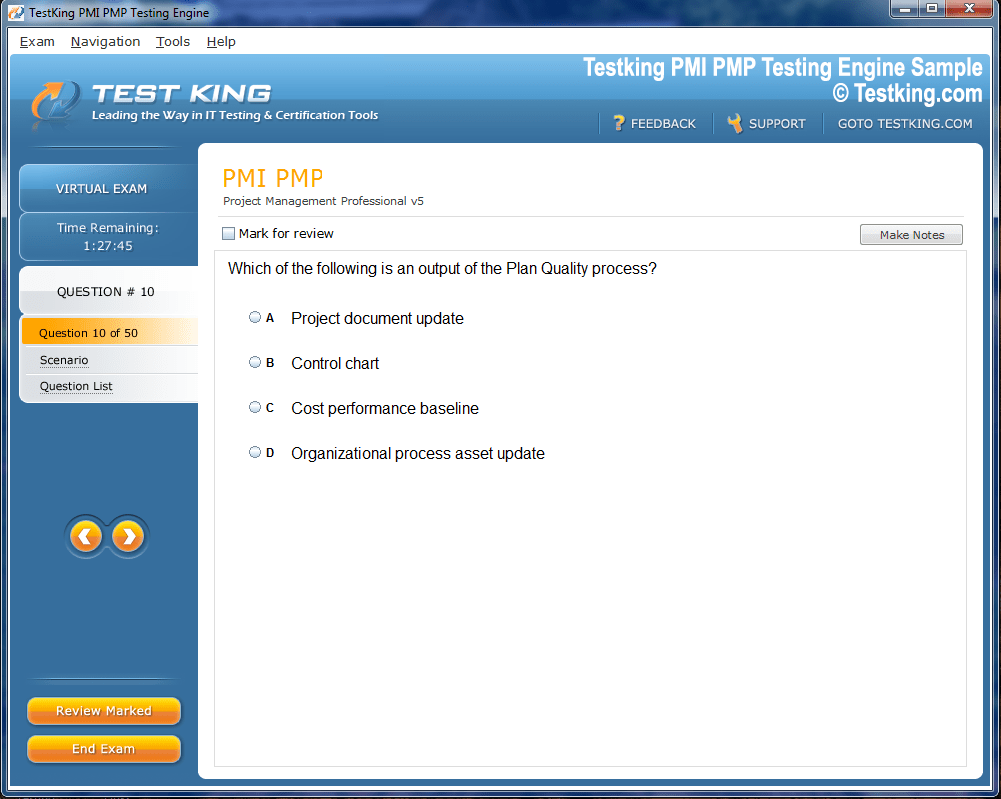
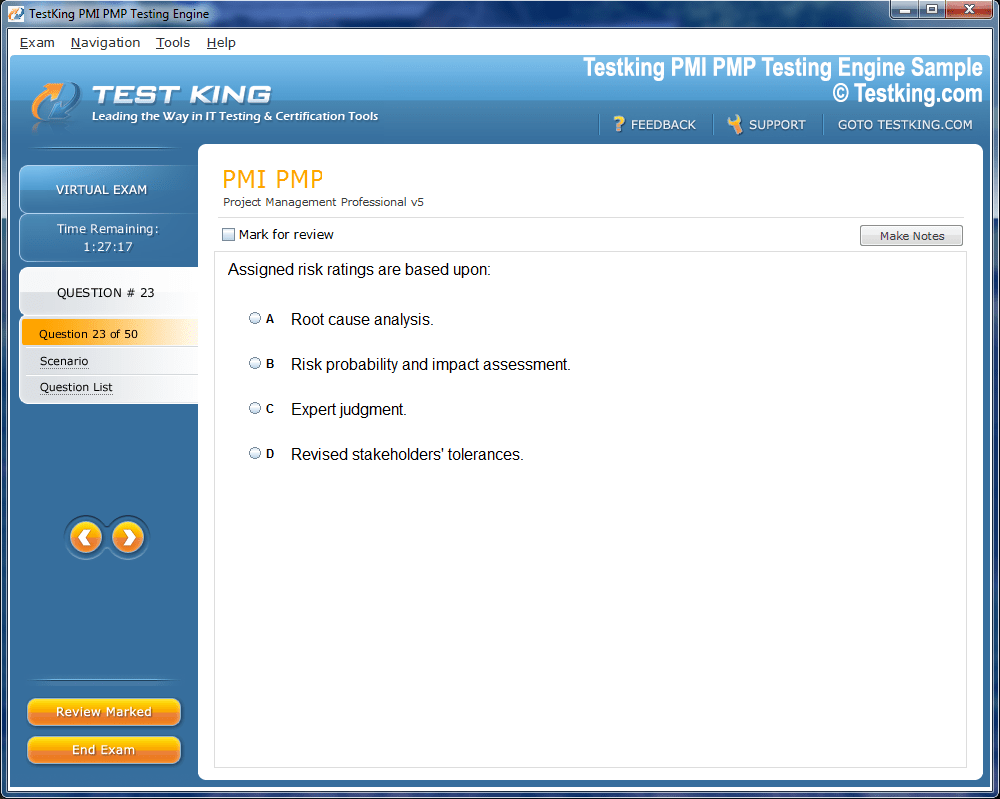
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our AHM-520 testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Top AHIP Exams
Preparing Effectively for the AHIP AHM-520 Exam Journey
The healthcare industry operates as a complex ecosystem driven by policy, regulation, financial stability, and risk evaluation. Within this intricate network, the AHIP AHM-520 exam has emerged as an essential credential for professionals seeking to validate their competence in health insurance and risk management. The examination, developed by America’s Health Insurance Plans, has become a benchmark for those determined to strengthen their expertise in the administrative and operational functions of the health insurance sector. Understanding this certification requires more than a surface-level overview—it involves delving into the structure of the exam, its underlying principles, and its significance in shaping a proficient and compliant workforce.
The AHIP AHM-520 exam does not exist in isolation. It is one of the core modules offered through AHIP's broader educational programs, which collectively aim to cultivate knowledge across the diverse components of healthcare management. As the healthcare landscape continues to evolve, marked by regulatory changes, shifting risk pools, and the integration of new technologies, the exam ensures that professionals possess the analytical and operational insight necessary to navigate these challenges effectively.
In this first installment, the focus lies on understanding the broader purpose of the AHIP AHM-520 exam, its alignment with the objectives of the health insurance industry, and how it serves as an essential stepping stone for career growth and institutional compliance.
The Foundation and Purpose of the AHIP AHM-520 Exam
America’s Health Insurance Plans (AHIP) serves as the unifying voice for health insurance organizations across the United States. Through advocacy, education, and certification programs, AHIP strives to promote a sustainable healthcare system centered on efficiency, equity, and innovation. The AHM-520 exam, titled “Health Insurance Operations: Strategic and Operational Functions,” represents one of AHIP’s most specialized certifications.
The purpose of the exam extends beyond testing theoretical knowledge—it evaluates an individual’s ability to apply core principles of health insurance operations in practical scenarios. It assesses the understanding of underwriting principles, pricing methodologies, risk management frameworks, and the financial mechanisms that sustain the health insurance infrastructure. The exam aims to ensure that candidates are not only familiar with policy and regulation but can also interpret and implement them effectively within real-world contexts.
AHIP designed this exam to bridge the gap between conceptual understanding and operational proficiency. For individuals working within insurance carriers, health plans, or consulting firms, the AHM-520 certification validates that they can contribute meaningfully to decision-making processes, compliance efforts, and financial strategies. In an era where regulatory oversight is intensifying and consumer expectations are shifting, the ability to align operational processes with industry standards has become indispensable.
The Relevance of Health Insurance Education in Modern Healthcare
Health insurance serves as the backbone of the healthcare delivery system. Without structured financing, the industry would struggle to provide equitable access, manage costs, or distribute resources effectively. As such, education surrounding health insurance operations has become a cornerstone of professional development for those aspiring to work in the sector.
The AHM-520 exam encapsulates this educational imperative by encompassing the major functional areas of insurance operations. It focuses on underwriting, which involves assessing the risk associated with insuring individuals or groups; pricing, which ensures that the cost of coverage reflects projected claims; and financial management, which sustains the solvency and stability of the organization.
Beyond financial and operational considerations, the exam also reinforces the importance of ethical and regulatory compliance. With the healthcare system governed by numerous state and federal laws, from the Affordable Care Act to state insurance mandates, understanding the regulatory environment is crucial. Professionals who possess this knowledge are better equipped to ensure compliance, minimize legal risk, and promote transparency in insurance practices.
Furthermore, as value-based care and digital transformation reshape the healthcare ecosystem, the AHM-520 curriculum emphasizes adaptability. It encourages candidates to think strategically about how operational efficiency can coexist with patient-centered care, ensuring that health insurance continues to function as a mechanism of both financial protection and health promotion.
Exam Structure and Core Competencies
To appreciate the magnitude of the AHM-520 exam, it is necessary to examine its structure and the competencies it seeks to evaluate. The exam typically includes multiple-choice questions that require candidates to apply both conceptual understanding and analytical reasoning.
The content is organized into several domains that represent the essential operational pillars of the health insurance industry:
Underwriting and Risk Evaluation: This area examines how insurers assess the probability and potential cost of claims. Candidates must understand how demographic, geographic, and behavioral factors influence risk assessment and how data analytics contributes to more precise underwriting decisions.
Pricing and Product Design: The exam explores how insurance plans are priced based on actuarial data, medical cost trends, and competitive market analysis. It evaluates how pricing strategies align with organizational goals and regulatory constraints.
Financial Management and Performance: Financial sustainability remains a vital aspect of any health insurance organization. The AHM-520 exam tests knowledge of revenue models, expense management, reserves, and financial reporting principles that underpin operational integrity.
Regulatory Compliance: The health insurance industry operates within a highly regulated environment. The exam assesses understanding of relevant laws, standards, and administrative guidelines that govern the conduct of insurers and protect consumer interests.
Operational Strategy and Management: Beyond the technical aspects, the exam measures a candidate’s ability to think strategically about process optimization, stakeholder communication, and interdepartmental collaboration.
Each of these domains reflects the multifaceted nature of health insurance operations. A candidate must not only memorize definitions but also grasp the interrelationships among these components. This holistic understanding ensures that professionals can adapt to evolving business models and regulatory frameworks.
The Significance of Certification in Career Advancement
Obtaining the AHIP AHM-520 certification signifies more than academic achievement—it demonstrates professional credibility and a commitment to continuous improvement. In a competitive industry where compliance, efficiency, and adaptability determine success, possessing specialized credentials can distinguish a candidate from their peers.
Employers across health insurance companies, managed care organizations, and consulting firms recognize AHIP certification as evidence of a candidate’s capability to manage complex operational tasks. For individuals aspiring to managerial or analytical roles, this certification provides an advantage by showcasing a mastery of industry standards and practices.
Beyond individual advancement, the AHM-520 exam contributes to organizational growth. Certified professionals bring structured problem-solving skills, operational insight, and a heightened awareness of compliance obligations. Their expertise supports strategic decision-making and risk mitigation, fostering a culture of accountability and innovation within their organizations.
Moreover, the certification aligns with broader trends in professional development, where employers increasingly value specialized knowledge verified through standardized assessments. As regulatory frameworks evolve and the need for data-driven decision-making grows, the demand for certified professionals in health insurance operations continues to expand.
Building a Framework for Exam Preparation
Preparing for the AHM-520 exam requires a methodical approach that balances comprehension with application. Candidates benefit from developing a study plan grounded in the exam blueprint, which outlines the content areas and relative weight of each section.
The blueprint serves as a roadmap, allowing individuals to allocate time effectively and prioritize topics that carry greater significance. Since the exam encompasses a broad range of concepts, from financial analysis to regulatory compliance, organizing study sessions around thematic clusters can enhance retention and understanding.
Engaging with AHIP’s official course materials remains the most effective preparation strategy. These resources are meticulously designed to align with the competencies tested in the exam. They include case studies, conceptual explanations, and practical examples that mirror real-world scenarios. Reviewing these materials thoroughly helps candidates connect theoretical concepts with operational realities.
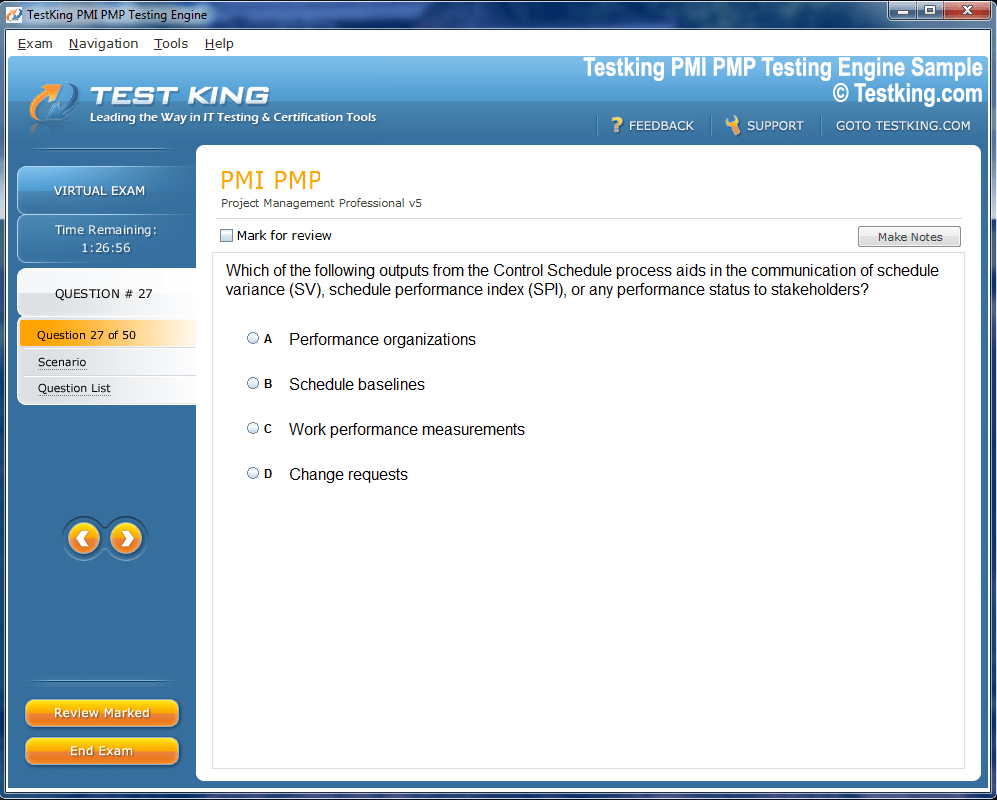
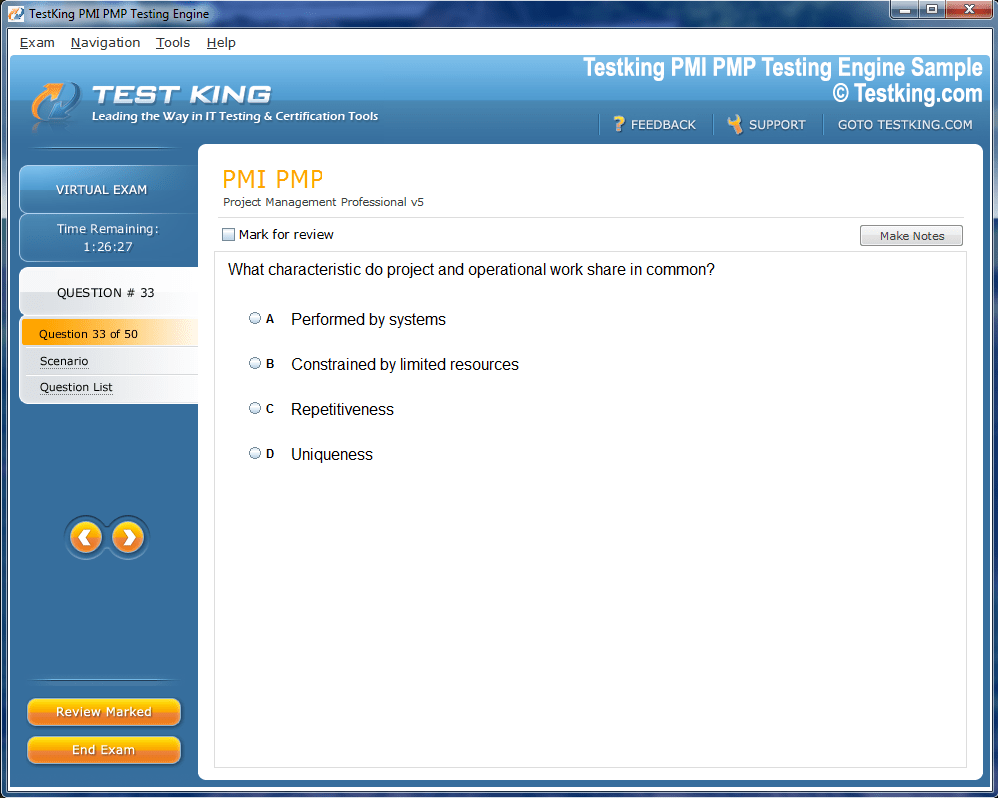
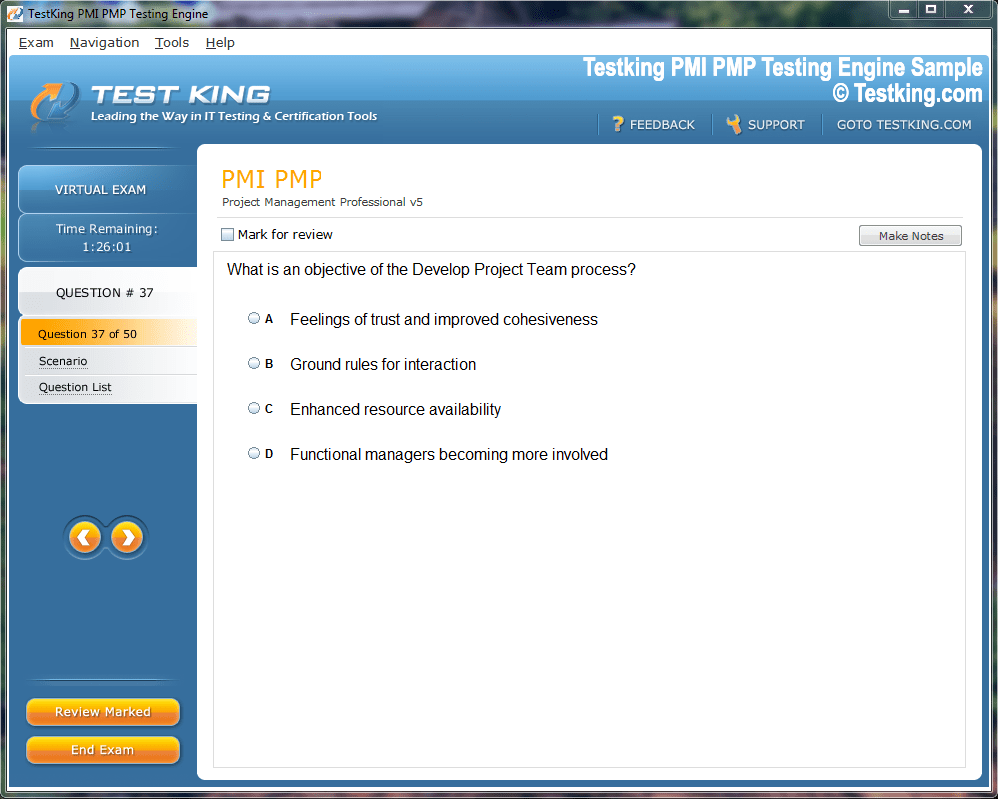
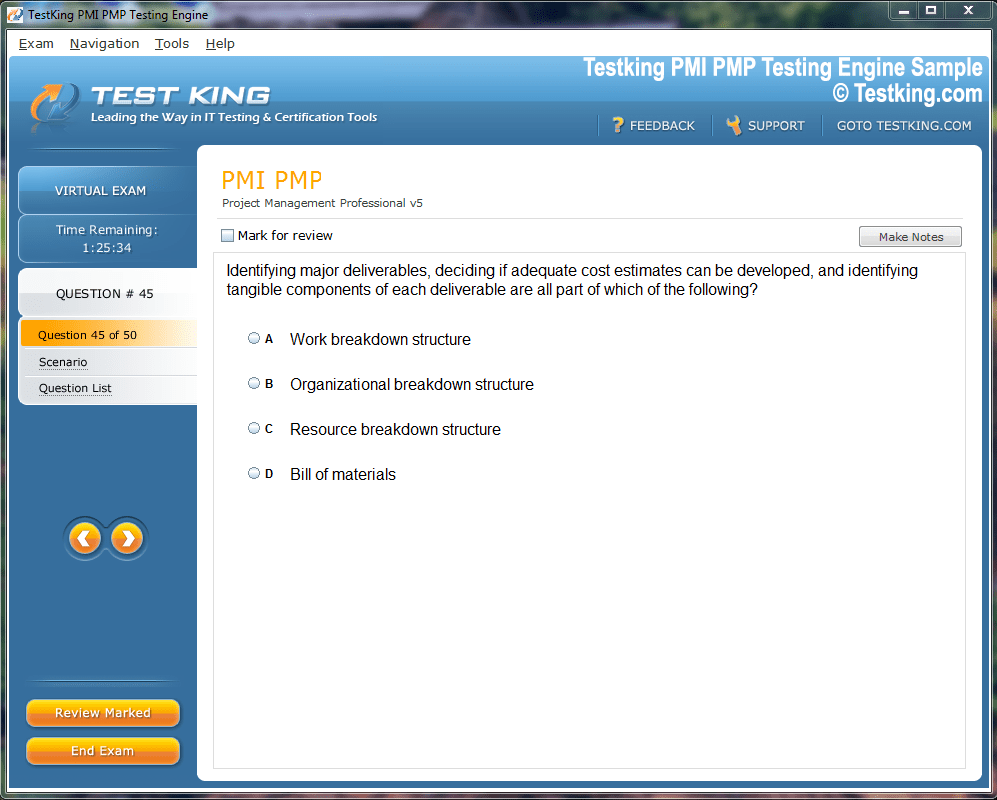
Practice exams play an equally vital role in preparation. They familiarize candidates with the exam format, timing, and complexity of questions. By simulating actual test conditions, practice exams help identify areas of weakness and build confidence. Consistent practice also improves time management, ensuring that candidates can complete the test efficiently within the allotted time frame.
For those who benefit from collaborative learning, study groups provide an avenue to exchange ideas, discuss challenging concepts, and clarify doubts. Explaining material to others reinforces comprehension and uncovers nuances that may otherwise be overlooked.
Additionally, AHIP occasionally offers webinars and training sessions conducted by industry experts. These interactive opportunities allow candidates to gain practical insights, ask questions, and strengthen their conceptual foundations. Integrating such sessions into one’s preparation plan can provide a comprehensive understanding of the subject matter.
Understanding the Broader Impact of Risk Management
Risk management stands as the cornerstone of health insurance operations. The AHM-520 exam emphasizes this discipline, underscoring its significance in maintaining organizational solvency and protecting both insurers and policyholders.
Effective risk management involves identifying, analyzing, and mitigating potential financial losses arising from unpredictable events. Within the context of health insurance, this includes managing medical cost variability, evaluating claims experience, and anticipating regulatory changes that could affect financial performance.
Candidates studying for the AHM-520 exam are expected to understand the intricate relationship between risk and pricing. Premiums must be set at a level that reflects expected costs while ensuring profitability and market competitiveness. The balance between affordability and sustainability lies at the heart of health insurance strategy.
Furthermore, the exam delves into the role of reinsurance as a tool for spreading risk. By transferring portions of their risk exposure to other entities, insurers safeguard their financial position and enhance stability. This mechanism highlights the interconnected nature of the global insurance ecosystem.
Understanding the principles of risk management also involves exploring the ethical dimensions of decision-making. Insurers must maintain fairness and transparency while balancing commercial objectives with social responsibility. This ethical component forms an implicit but essential theme throughout the AHM-520 curriculum.
Strategic Preparation for the AHIP AHM-520 Exam
The AHIP AHM-520 exam is a sophisticated evaluation that measures both the theoretical understanding and applied competence of professionals within the health insurance and risk management sphere. Success in this examination demands not only a thorough grasp of insurance operations but also the ability to integrate concepts into coherent analytical frameworks. Preparing for such a test involves more than memorizing content; it requires cultivating a disciplined mindset, applying strategic study techniques, and maintaining intellectual persistence.
Strategic preparation forms the bedrock of success for this exam. Candidates who approach the process methodically tend to demonstrate a stronger command of material and perform more consistently under examination conditions.
Understanding the Intellectual Demands of the AHM-520 Exam
The AHIP AHM-520 exam is designed to evaluate how well a candidate can synthesize and apply complex ideas. It assesses knowledge across multiple domains of health insurance operations, requiring precision, judgment, and conceptual flexibility. These qualities cannot be acquired overnight; they must be cultivated through disciplined and deliberate preparation.
One of the intellectual demands of the exam lies in the intersection between financial analysis and regulatory comprehension. The test evaluates the ability to interpret how rules, policies, and actuarial models coalesce into sustainable operational practices. Candidates are expected to demonstrate a mature understanding of how health insurance companies maintain solvency, assess risk pools, and price products responsibly.
The exam also emphasizes operational strategy—how organizations manage workflows, optimize administrative processes, and ensure compliance. Candidates must navigate abstract concepts such as risk diversification, capital adequacy, and cost containment while connecting them to tangible industry practices.
Preparing for these multifaceted requirements demands more than surface familiarity. It requires internalization—the deep, meaningful understanding of how theory manifests in practice. Successful candidates therefore adopt learning approaches that go beyond rote memorization, focusing instead on conceptual mastery and contextual awareness.
Crafting a Study Plan Rooted in Structure and Consistency
The foundation of exam readiness is a structured study plan. The AHM-520 exam’s vast syllabus can overwhelm even experienced professionals without careful time management. Building a systematic plan helps distribute study sessions evenly and ensures that no domain receives disproportionate attention.
The first step is to acquire and review the official AHIP AHM-520 exam blueprint. This document outlines the content categories, competencies, and percentage weight of each section. By studying the blueprint, candidates gain clarity on where to allocate the most time and effort.
Once the blueprint is understood, the next step involves dividing the preparation period into phases. The initial phase should focus on comprehensive reading—covering all the official study materials to build foundational understanding. During this stage, candidates should aim for breadth rather than depth, emphasizing familiarity with all topics.
The second phase involves deep learning—analyzing case studies, exploring real-world examples, and cross-referencing theoretical principles with practical application. This is where candidates move from awareness to comprehension.
The final phase centers on consolidation. Here, review sessions, practice exams, and timed exercises become the primary focus. The goal is to reinforce memory, refine problem-solving techniques, and simulate test-day conditions.
Consistency is critical throughout the process. Short, focused study sessions tend to be more effective than sporadic, marathon sessions. Maintaining a consistent rhythm prevents cognitive fatigue and promotes long-term retention.
Using Cognitive Science to Enhance Learning Efficiency
Studying for the AHIP AHM-520 exam can be made significantly more effective by applying principles derived from cognitive science. Understanding how memory, attention, and comprehension function allows candidates to study more intelligently rather than more intensively.
One such principle is spaced repetition—the systematic review of material at increasing intervals over time. Instead of rereading content in one sitting, candidates revisit key topics periodically, which reinforces memory and strengthens recall.
Another effective method is active recall. Rather than passively reviewing notes, candidates should challenge themselves to retrieve information without prompts. This could involve explaining a concept aloud, writing summaries from memory, or answering self-generated questions. Active recall strengthens neural connections and enhances long-term retention.
Interleaved learning, or alternating between topics during study sessions, can also be highly effective. Instead of studying underwriting principles for hours without interruption, alternating between underwriting, pricing, and financial management forces the brain to continually retrieve and reorganize information, improving comprehension and adaptability.
Additionally, elaborative interrogation—asking “why” and “how” questions—encourages deeper understanding. For instance, when studying risk management, a candidate might ask: “Why do insurers diversify portfolios?” or “How does regulatory oversight influence capital allocation?” Such reflection fosters critical thinking and contextual insight.
Sleep and nutrition play a crucial role in cognitive performance as well. Adequate rest ensures that learned material consolidates into long-term memory, while a balanced diet sustains focus and energy. Candidates who maintain physical health during preparation often experience greater mental clarity and resilience.
Leveraging Official Resources and Supplementary Learning
The AHIP AHM-520 exam is supported by a comprehensive suite of learning materials developed by America’s Health Insurance Plans. These resources are indispensable because they are designed by the same organization that administers the exam, ensuring alignment with the actual test structure and expectations.
Candidates should begin with the official course textbook, which provides an authoritative overview of health insurance operations, financial management, and risk analysis. Each chapter builds upon the previous one, introducing concepts progressively while linking theoretical frameworks to operational realities.
In addition to the textbook, AHIP often provides online learning modules, study guides, and practice exams. These materials allow candidates to assess their readiness through self-testing and reinforce their understanding through guided review.
However, some candidates benefit from integrating supplementary materials to broaden their comprehension. Industry journals, white papers, and analytical reports provide insights into emerging trends in health insurance operations and regulatory evolution. By relating these real-world developments to the foundational principles covered in the AHM-520 course, candidates cultivate a richer and more dynamic perspective.
Furthermore, candidates employed within the health insurance industry can apply their learning directly in the workplace. Observing underwriting practices, financial reviews, or compliance meetings provides practical exposure that enhances academic understanding. This experiential learning bridges the gap between theory and application, making the content more tangible and memorable.
The Role of Analytical Thinking in Exam Success
Analytical reasoning is the hallmark of an accomplished AHM-520 candidate. The exam does not simply test whether one can recall definitions; it evaluates the ability to apply analytical judgment to multifaceted scenarios. Developing analytical acumen requires deliberate effort and structured practice.
To sharpen this skill, candidates should analyze case studies and construct hypothetical models. For instance, when studying financial management, they can create simplified versions of balance sheets or simulate pricing strategies under varying risk assumptions. Such exercises reveal the practical consequences of theoretical principles, enhancing conceptual clarity.
Another powerful approach involves engaging in comparative analysis. Candidates might examine different underwriting methods or pricing frameworks, exploring how each influences financial outcomes and risk exposure. By comparing contrasting methodologies, one gains a nuanced appreciation of how decisions are shaped by context, data, and organizational objectives.
Critical reasoning also involves questioning assumptions. Health insurance operates in a volatile environment influenced by regulation, market behavior, and public policy. Effective analysts must evaluate how these variables interact, anticipating challenges before they arise. Incorporating this mindset into exam preparation allows candidates to think beyond the obvious and develop the capacity for strategic foresight.
Analytical thinking should also extend to time management during the test itself. Candidates must evaluate question difficulty, allocate time proportionately, and avoid the trap of excessive deliberation on a single question. The same logical principles that apply to financial analysis can be applied to optimizing test performance—assess the situation, prioritize efficiently, and execute decisively.
The Importance of Contextual Awareness in Health Insurance
The AHIP AHM-520 exam places strong emphasis on understanding how operational functions interact within the larger healthcare ecosystem. Success therefore depends on recognizing context—the broader environmental, economic, and regulatory conditions that influence decision-making in the industry.
For instance, pricing decisions cannot be isolated from demographic trends, medical cost inflation, or regulatory requirements. A health plan that fails to consider these contextual factors risks financial instability and reputational damage. The exam expects candidates to recognize such interdependencies.
Similarly, underwriting practices must adapt to market behavior, competitive pressures, and ethical expectations. Effective underwriting balances quantitative precision with human judgment, ensuring that risk assessment aligns with both profitability goals and social responsibility.
Financial management, too, must be understood contextually. Reserves, liquidity ratios, and investment strategies are shaped not only by mathematical formulas but also by economic cycles and policy mandates.
This contextual awareness extends to compliance. Regulations are not static; they evolve with legislative changes, judicial interpretations, and policy shifts. Professionals who remain attuned to these dynamics contribute to the resilience and credibility of their organizations.
Preparing for the AHM-520 exam therefore involves developing the ability to perceive patterns, connections, and implications beyond the immediate topic. The more a candidate understands how individual components fit into the broader system, the more effectively they can analyze and respond to exam questions.
Mastering Risk Management and Financial Integrity in the AHIP AHM-520 Exam
Health insurance operates at the intersection of risk, regulation, and financial responsibility. For candidates pursuing the AHIP AHM-520 exam, understanding the profound relationship between these dimensions is essential. Risk management, in particular, forms the intellectual nucleus of the entire health insurance framework, while financial integrity ensures that organizations maintain stability amidst uncertainty. Together, these disciplines shape the operational resilience of insurers and determine the effectiveness of health coverage as a social and economic instrument.
The Strategic Role of Risk Management in Health Insurance
In the domain of health insurance, risk management serves as both a defensive and strategic function. It protects organizations from unexpected losses while enabling them to design products that meet market needs. Effective risk management is not merely about minimizing exposure—it involves optimizing risk to ensure both sustainability and profitability.
The AHIP AHM-520 exam challenges candidates to understand how risk manifests at multiple levels: underwriting, claims processing, pricing, and regulatory compliance. Each layer demands precision, as even minor miscalculations can have extensive repercussions.
At its core, risk management begins with risk identification, the process of recognizing potential sources of uncertainty that could affect organizational performance. These include medical cost fluctuations, demographic variations, provider behavior, policy changes, and macroeconomic shifts. Once risks are identified, professionals move to risk assessment, quantifying the probability and potential impact of these factors using actuarial models and statistical tools.
The next step, risk control, focuses on developing mechanisms to mitigate adverse outcomes. This could involve diversifying risk pools, adjusting premium structures, implementing utilization management programs, or securing reinsurance. Finally, risk monitoring ensures that mitigation strategies remain effective over time, adapting to changing market and regulatory conditions.
Candidates must appreciate that risk management is not static—it evolves with medical innovation, data analytics, and consumer expectations. The ability to perceive risk dynamically distinguishes a competent professional from a reactive one.
Underwriting as the Core of Risk Evaluation
Underwriting is the operational embodiment of risk management. It transforms abstract risk assessments into concrete decisions about whether and how to insure individuals or groups. Within the AHIP AHM-520 exam, underwriting principles occupy a central role, as they encapsulate the analytical precision and ethical responsibility inherent in health insurance operations.
The underwriting process evaluates the risk profile of applicants by analyzing health status, age, location, occupation, and other determinants. This assessment guides decisions on eligibility, coverage level, and premium pricing. Candidates must understand that the goal is not to deny coverage but to balance affordability for consumers with sustainability for insurers.
There are two primary forms of underwriting: individual underwriting, where policies are customized based on personal data, and group underwriting, which evaluates the collective risk of an organization or association. Group underwriting typically leverages the law of large numbers to spread risk across a broader base, allowing for more predictable cost estimation.
The exam also expects candidates to grasp the ethical and regulatory implications of underwriting decisions. Regulations such as the Affordable Care Act have transformed traditional underwriting practices by limiting the extent to which health conditions and demographics can influence pricing and eligibility. Professionals must therefore navigate the tension between actuarial fairness and regulatory compliance.
Advanced underwriting now integrates predictive analytics and machine learning to enhance accuracy. Data-driven models can identify patterns in claims behavior, medical trends, and population health indicators, enabling insurers to anticipate risk with greater sophistication. However, these technological tools also introduce challenges related to data privacy and algorithmic bias—issues that demand vigilant oversight and ethical discernment.
The Economics of Pricing and Its Relationship to Risk
Pricing represents the translation of risk into monetary terms. It embodies the insurer’s assessment of expected costs, administrative expenses, and desired margins. Within the context of the AHIP AHM-520 exam, pricing stands as a bridge between actuarial analysis and market strategy.
The foundation of insurance pricing lies in actuarial science, where statistical models forecast the likelihood and magnitude of future claims. These projections consider a multitude of variables—age distribution, chronic disease prevalence, provider reimbursement rates, and utilization trends. The objective is to determine premiums that cover anticipated costs while remaining competitive in the market.
However, pricing is not purely mathematical. It is influenced by market competition, consumer behavior, regulatory constraints, and broader economic conditions. For instance, an insurer might maintain lower premiums in a highly competitive environment, accepting narrower profit margins in exchange for market share growth. Conversely, in a market dominated by high-cost providers or limited competition, pricing flexibility may be constrained.
The exam challenges candidates to think critically about pricing strategy—how to achieve equilibrium between risk exposure and financial sustainability. Overpricing may alienate customers, while underpricing threatens solvency. The ability to balance these forces reflects strategic acumen and operational prudence.
Another dimension of pricing is experience rating versus community rating. Experience rating bases premiums on the historical claims experience of a group, while community rating spreads risk more evenly across a population regardless of individual or group claims history. Understanding when and how to apply these methodologies is vital, as each approach carries implications for equity, predictability, and compliance.
Financial Integrity and Organizational Sustainability
Financial integrity serves as the bedrock of the health insurance industry. Without sound financial management, even the most sophisticated risk models collapse under real-world pressures. The AHIP AHM-520 exam emphasizes financial principles because they underpin every operational and strategic decision made within an insurance organization.
Financial integrity begins with capital management—ensuring that the organization maintains sufficient reserves to meet obligations. Insurers must hold statutory reserves as mandated by regulators, which act as safeguards against unexpected claims surges or economic downturns. Proper reserve estimation requires actuarial precision, as underestimating liabilities can threaten solvency while overestimating may constrain growth.
The concept of liquidity management is equally critical. Health insurance organizations must ensure that they can access cash or liquid assets promptly to pay claims and administrative expenses. Poor liquidity can erode consumer trust and invite regulatory intervention.
Another cornerstone of financial integrity is investment strategy. Insurers typically invest premium income to generate returns that supplement operational revenue. However, investments must align with risk tolerance and statutory restrictions. The AHM-520 curriculum expects candidates to understand how portfolio diversification, duration matching, and asset-liability management contribute to overall financial health.
Moreover, financial reporting and transparency sustain the credibility of insurers in the eyes of regulators, policyholders, and investors. Adherence to accounting standards, accurate valuation of liabilities, and timely disclosure of financial performance are non-negotiable elements of integrity.
Financial management also intersects with strategic planning. Profitability must be balanced with compliance and consumer protection. The ability to align financial goals with ethical and regulatory obligations reflects a mature understanding of the industry’s moral and economic responsibilities.
Regulatory Oversight and the Framework of Accountability
Regulation serves as the framework within which health insurers operate. It establishes boundaries, ensures fairness, and maintains consumer protection. The AHIP AHM-520 exam evaluates how well candidates comprehend the interconnected web of laws, administrative rules, and oversight mechanisms governing health insurance operations.
Regulatory oversight originates at both federal and state levels. Agencies such as state insurance departments enforce solvency standards, review premium filings, and monitor market conduct. Federal legislation, including the Affordable Care Act and the Health Insurance Portability and Accountability Act, defines requirements for coverage, nondiscrimination, and data privacy.
Candidates must understand that compliance is not merely a procedural obligation but a strategic imperative. Noncompliance can lead to severe penalties, reputational harm, and operational disruptions. Therefore, effective organizations embed compliance within their governance structures, ensuring that every department—underwriting, claims, finance, and marketing—aligns with regulatory expectations.
An integral concept is corporate governance, which defines the internal system of accountability within an insurer. It encompasses board oversight, internal audits, ethical standards, and transparency measures. Strong governance ensures that decision-making reflects both fiduciary responsibility and public trust.
The exam also underscores the importance of consumer protection regulations. These rules mandate clarity in policy communication, fairness in claims handling, and adherence to coverage guarantees. Professionals must interpret and apply these provisions to safeguard consumer interests without compromising financial prudence.
In a constantly shifting regulatory environment, adaptability becomes indispensable. Health insurance professionals must remain vigilant, updating internal processes as laws evolve. The ability to interpret regulation dynamically represents not only compliance but strategic resilience.
The Ethical Foundation of Financial and Risk Decisions
Ethics represents the invisible architecture supporting every decision in health insurance operations. Financial and risk-related choices, when guided by ethical principles, sustain public confidence and institutional legitimacy. The AHIP AHM-520 exam implicitly emphasizes ethical reasoning throughout its focus areas, recognizing that technical competence without integrity can lead to systemic failure.
At its core, ethical decision-making in health insurance involves balancing competing interests—profitability, fairness, and access. Professionals must ensure that decisions made in underwriting, pricing, or claims management reflect transparency and justice.
For example, when evaluating risk, insurers may face dilemmas concerning data usage. Predictive analytics can improve accuracy but may inadvertently perpetuate inequities if algorithms rely on biased data. Ethical professionals recognize these risks and implement safeguards to preserve fairness.
Financial ethics similarly require prudence and honesty. Misrepresenting financial strength, manipulating reserves, or obscuring liabilities can erode trust and invite regulatory sanction. Integrity demands that financial disclosures accurately reflect the organization’s condition and that profitability never supersedes moral responsibility.
The ethical dimension extends to leadership behavior. Executives and managers set the tone for corporate culture. A transparent, accountable, and equitable culture promotes compliance and strengthens the organization’s reputation.
Ultimately, ethics is not an external constraint but an internal compass. It transforms regulation from an obligation into a shared value, ensuring that health insurance fulfills its role as a social good as well as a commercial enterprise.
Regulatory Compliance and Governance in the AHIP AHM-520 Exam
Health insurance exists within one of the most heavily regulated sectors of the economy. The complex interaction of state and federal laws, administrative rules, and judicial interpretations defines the boundaries within which insurers must operate. For professionals preparing for the AHIP AHM-520 exam, understanding this regulatory framework is indispensable. It forms the foundation upon which ethical practice, financial transparency, and operational integrity are built.
Regulatory compliance is not a peripheral concern—it is an intrinsic part of daily decision-making across all levels of a health insurance organization. Whether pricing a new product, processing claims, or managing financial reserves, every action must align with established laws and standards. Governance, meanwhile, ensures that this alignment is systemic rather than incidental. It transforms compliance from an isolated task into a continuous institutional discipline.
The Foundations of Health Insurance Regulation
Health insurance regulation in the United States is the product of historical evolution. It reflects a balance between public protection and market autonomy, shaped by decades of legislative development and policy reform. Understanding these origins allows candidates to appreciate why certain rules exist and how they maintain equilibrium between consumer interests and corporate sustainability.
The earliest regulatory principles emerged at the state level, where insurance departments were tasked with ensuring solvency and fair conduct among insurers. This state-based system remains central today, as each state retains authority to license insurers, review premium filings, and enforce market conduct standards.
The federal government’s involvement expanded significantly in the twentieth century, particularly through the enactment of the Employee Retirement Income Security Act, the Health Insurance Portability and Accountability Act, and the Affordable Care Act. Each introduced new dimensions of oversight, from privacy and nondiscrimination to access and affordability.
The AHIP AHM-520 exam requires candidates to understand how these multiple layers of authority coexist. It tests the ability to interpret how state and federal requirements interact, overlap, or occasionally conflict. Professionals must learn to navigate this complex regulatory mosaic without compromising compliance or efficiency.
Another critical aspect is the principle of solvency oversight. Regulators must ensure that insurers possess sufficient financial resources to meet future obligations. Solvency regulations protect policyholders from the catastrophic consequences of insurer insolvency, reinforcing public confidence in the system. Candidates must grasp how these solvency requirements—such as capital adequacy ratios, reserve standards, and investment restrictions—function in practice.
The Scope of Federal Regulation in Health Insurance
While state governments maintain primary regulatory authority, federal laws establish broad frameworks that influence all health insurance operations. These laws embody social policy objectives, balancing consumer protection with systemic sustainability.
One of the most influential federal statutes is the Health Insurance Portability and Accountability Act. It introduced privacy protections for health information and established standards for data security. Compliance with its provisions requires rigorous administrative controls, employee training, and technological safeguards.
The Affordable Care Act, meanwhile, transformed both the market structure and operational requirements of insurers. It introduced community rating standards, essential health benefits, and prohibitions on discrimination based on preexisting conditions. For professionals, this law exemplifies how social policy can reshape actuarial and operational practices.
Federal oversight also extends to programs such as Medicare and Medicaid, which establish reimbursement frameworks and influence the economics of private insurance markets. Insurers participating in these programs must adhere to additional layers of reporting, auditing, and quality monitoring.
The AHM-520 exam challenges candidates to understand the conceptual underpinnings of such regulations rather than memorizing statutes. It demands comprehension of how legal requirements translate into operational procedures, compliance systems, and governance structures.
State-Based Regulation and Market Conduct Oversight
State regulation remains the cornerstone of U.S. insurance governance. Each state’s insurance department acts as a gatekeeper, responsible for licensing entities, approving policy forms, reviewing premium rates, and monitoring claims practices.
Market conduct examinations form a key instrument of state oversight. These examinations assess whether insurers treat consumers fairly, handle claims promptly, and provide accurate information in marketing materials. A pattern of violations can result in sanctions, fines, or loss of licensure.
The AHIP AHM-520 exam emphasizes the operational implications of these state-based rules. Professionals must recognize how compliance influences daily business processes—such as product development, underwriting, and policy administration. They must also understand how state variations create complexity for national insurers operating across multiple jurisdictions.
Another central element of state regulation is rate review. Insurers must justify proposed premium changes by demonstrating their actuarial soundness and alignment with regulatory guidelines. Regulators evaluate assumptions regarding claims costs, administrative expenses, and profit margins. This process ensures that pricing remains fair and transparent while safeguarding solvency.
State regulators also enforce consumer complaint resolution procedures, ensuring that disputes between policyholders and insurers are addressed equitably. The oversight mechanisms reinforce public trust by guaranteeing accountability and responsiveness within the marketplace.
The Structure and Purpose of Corporate Governance
Corporate governance represents the internal mechanism through which health insurance organizations maintain accountability, ethical integrity, and strategic coherence. It ensures that decisions reflect fiduciary responsibility toward policyholders, shareholders, and society at large.
The AHIP AHM-520 exam evaluates understanding of governance structures because they underpin compliance, financial management, and operational ethics. Governance is not confined to the boardroom—it influences the entire organizational culture.
At its highest level, governance is executed by a board of directors. The board establishes strategic direction, monitors performance, and ensures adherence to legal and ethical standards. Independent directors often serve on audit or compliance committees to provide impartial oversight.
Senior management implements board policies through internal controls, risk management frameworks, and compliance programs. Every employee, in turn, bears responsibility for upholding ethical standards and reporting potential violations. This chain of accountability transforms governance from theory into daily practice.
Transparency forms a central tenet of good governance. Accurate reporting, open communication, and consistent disclosure of information to regulators and stakeholders ensure that organizations operate with integrity. The absence of transparency often signals systemic weaknesses that may culminate in regulatory intervention.
Governance also intersects with enterprise risk management. Boards must ensure that risk-taking aligns with strategic goals and that mitigation strategies protect both financial and reputational capital. The integration of governance and risk management reinforces the long-term sustainability of the organization.
Building a Culture of Compliance
Compliance is most effective when it transcends formal policy and becomes ingrained in organizational culture. For candidates preparing for the AHIP AHM-520 exam, understanding how to cultivate such a culture is crucial.
A compliance culture is characterized by awareness, accountability, and ethical conviction. Employees at all levels must comprehend the regulatory expectations governing their activities and feel empowered to act when they perceive potential violations.
Developing this culture begins with education. Regular training sessions, accessible policy manuals, and continuous communication ensure that compliance principles remain visible and relevant. When employees understand the rationale behind regulations, adherence becomes a matter of shared purpose rather than mere obligation.
Leadership plays an indispensable role. Executives who demonstrate commitment to compliance—by allocating resources, rewarding ethical behavior, and addressing violations decisively—set the tone for the entire organization. Their actions signal that compliance is not a cost but an investment in credibility.
Reporting mechanisms form another cornerstone of compliance culture. Anonymous hotlines, internal audits, and regular assessments create avenues for early detection of potential breaches. The ability to identify and rectify issues internally minimizes external enforcement risks and strengthens institutional integrity.
Ultimately, compliance culture is sustained by continuous reinforcement. It thrives on open communication, cross-departmental collaboration, and the alignment of incentives with ethical performance. When embedded deeply, it becomes a competitive advantage rather than a regulatory burden.
Ethical Decision-Making Within Regulatory Frameworks
Regulation establishes boundaries, but ethics determines how those boundaries are interpreted and applied. The AHIP AHM-520 exam underscores this distinction by assessing how candidates navigate ethical dilemmas that arise in operational contexts.
Ethical decision-making involves recognizing that legality does not always equate to morality. A decision may comply with the letter of the law yet violate its spirit. For example, designing policies that technically meet minimum coverage requirements but intentionally confuse consumers undermines ethical integrity even if it avoids legal sanction.
Professionals in health insurance must therefore apply ethical reasoning to decisions concerning pricing, claims adjudication, data usage, and communication. They must consider not only organizational benefit but also consumer welfare and public perception.
A valuable ethical model is the principle of proportionality—balancing competing obligations such as profit maximization, risk control, and social equity. This principle encourages decision-makers to seek outcomes that maintain fairness without jeopardizing organizational viability.
Transparency and honesty remain indispensable ethical values. Accurate disclosure of policy terms, truthful marketing, and responsible data stewardship contribute to consumer confidence and regulatory trust.
Ethical maturity, as examined in the AHM-520, reflects the ability to anticipate consequences and act with integrity even under pressure. It represents the alignment of professional competence with moral discernment.
Internal Auditing and Continuous Monitoring
Internal auditing operates as the operational backbone of compliance assurance. It provides independent evaluation of whether systems, processes, and practices conform to legal requirements and internal policies.
Auditing extends beyond financial verification; it encompasses operational efficiency, data security, and ethical compliance. By reviewing documentation, interviewing personnel, and testing internal controls, auditors identify vulnerabilities before they escalate into violations.
Continuous monitoring complements auditing by embedding oversight into daily operations. Automated systems can flag anomalies in claims processing, detect unusual financial transactions, or track deviations from policy standards. This proactive approach transforms compliance from a retrospective exercise into a real-time safeguard.
The AHIP AHM-520 exam expects candidates to appreciate how auditing and monitoring reinforce governance. Both mechanisms contribute to risk mitigation, transparency, and accountability. Professionals who understand their integration can design more robust compliance infrastructures.
Regular audits also facilitate communication with regulators. Demonstrating a history of proactive monitoring and corrective action often mitigates penalties during enforcement reviews. Thus, auditing serves not only as a compliance tool but also as a strategic asset.
Operational Excellence and Performance Management in the AHIP AHM-520 Exam
Health insurance organizations thrive on precision, efficiency, and ethical reliability. Beyond the domains of risk management and compliance, operational excellence defines the functional success of an insurer. For candidates preparing for the AHIP AHM-520 exam, understanding how operational processes interconnect with financial outcomes, consumer satisfaction, and regulatory expectations is fundamental.
Operational excellence in health insurance is the continuous pursuit of quality, accountability, and adaptability. It ensures that resources are used effectively, errors are minimized, and every department—from underwriting to claims processing—functions in harmony. The discipline goes beyond internal optimization; it extends to the organization’s ability to deliver value consistently within an ever-changing healthcare ecosystem.
The Essence of Operational Efficiency in Health Insurance
Efficiency in the health insurance industry transcends the mere reduction of administrative costs. It represents the deliberate alignment of workflows, technologies, and personnel toward delivering accurate, timely, and transparent services. The AHIP AHM-520 exam evaluates how well candidates comprehend these systemic interdependencies.
The structure of operational efficiency begins with process mapping—the identification and documentation of every step involved in service delivery. Whether processing claims, issuing policies, or resolving customer inquiries, each stage must be scrutinized for redundancy, bottlenecks, and risk exposure.
Once processes are clearly defined, organizations implement performance indicators to measure productivity, error rates, and turnaround times. These metrics form the empirical foundation of performance improvement. Continuous measurement allows management to detect inefficiencies early and intervene with targeted corrective action.
Another dimension of efficiency lies in automation and technology integration. Digital transformation allows insurers to replace manual, error-prone procedures with intelligent systems capable of real-time validation, data analysis, and workflow optimization. The use of automated adjudication tools, for instance, reduces processing time while enhancing accuracy in claim determinations.
However, efficiency must coexist with compliance and quality. The indiscriminate pursuit of speed can erode accuracy or fairness, undermining consumer trust and regulatory standing. True operational excellence, therefore, requires balance—a harmony between cost reduction and ethical responsibility.
Performance Management as a Strategic Imperative
Performance management provides the framework through which organizations evaluate success, promote accountability, and ensure alignment with strategic objectives. For health insurers, performance management extends from individual employees to entire business units.
The AHIP AHM-520 exam introduces candidates to key performance methodologies such as benchmarking, balanced scorecards, and key performance indicators (KPIs). These concepts transform abstract organizational goals into measurable, actionable targets.
Benchmarking compares internal performance with industry standards or best-in-class competitors. By identifying performance gaps, insurers can prioritize improvement initiatives and adopt proven practices from peers.
The balanced scorecard approach, pioneered in strategic management theory, integrates financial metrics with operational, customer, and learning perspectives. This holistic method ensures that short-term financial results do not overshadow long-term sustainability. In health insurance, a balanced scorecard might include indicators such as claims turnaround time, policyholder satisfaction, regulatory compliance scores, and employee engagement levels.
Performance management also encompasses continuous feedback systems. Regular evaluations and open communication channels between management and staff create a culture of accountability. When employees understand how their daily actions contribute to organizational goals, motivation and consistency improve.
Ultimately, effective performance management requires an organizational ethos of transparency and collaboration. Metrics and evaluations should be perceived not as punitive tools but as instruments for learning and development.
Quality Assurance and Service Consistency
Quality assurance represents the commitment to delivering reliable, accurate, and consumer-centered services. It is both a technical discipline and a moral obligation. In the context of the AHIP AHM-520 exam, quality assurance reflects the operational translation of ethical standards into measurable performance outcomes.
Health insurance quality assurance encompasses policy administration, claims accuracy, customer communication, and compliance with benefit terms. Every transaction must uphold legal standards and organizational integrity.
The first step toward quality assurance is establishing standards—clear criteria that define acceptable performance. These standards may derive from regulatory requirements, industry guidelines, or internal best practices. Once defined, standards serve as the benchmark for performance evaluation.
Next comes quality control, which involves real-time monitoring of operational processes. Automated systems can detect anomalies in claims data or flag deviations from established protocols. Continuous monitoring reduces the likelihood of systemic errors.
Equally important is quality improvement, a proactive process focused on long-term enhancement rather than short-term correction. Through root-cause analysis and trend evaluation, organizations identify persistent issues and implement structural changes to prevent recurrence.
For candidates, mastering quality assurance involves understanding both its quantitative and qualitative dimensions. While error rates and turnaround times are vital metrics, so too are empathy, communication clarity, and responsiveness—attributes that define the human aspect of insurance operations.
Process Optimization and Continuous Improvement
In modern insurance management, stagnation equates to obsolescence. Continuous improvement represents the ongoing refinement of operations in pursuit of greater effectiveness and adaptability.
The philosophy of continuous improvement originates from manufacturing methodologies such as Total Quality Management and Lean Management, but its principles apply seamlessly to health insurance. These methods emphasize incremental changes, employee involvement, and data-driven decision-making.
Lean methodologies focus on eliminating waste—activities that consume resources without creating value. In an insurance context, this could include redundant data entry, excessive document handling, or unnecessary approval layers.
Another complementary methodology is Six Sigma, which concentrates on minimizing variation and defects. By applying statistical analysis to operational data, insurers can achieve near-perfect accuracy in repetitive processes like claims adjudication or billing.
For candidates, the AHM-520 exam assesses understanding of how these methodologies enhance efficiency and compliance. Mastery involves recognizing that process optimization is not a project with an endpoint but a perpetual discipline that sustains organizational relevance in a competitive environment.
Data Analytics as the Engine of Operational Insight
Data analytics has become the intellectual centerpiece of contemporary health insurance operations. The ability to collect, interpret, and apply vast volumes of data distinguishes efficient, adaptive insurers from stagnant ones.
In the context of the AHIP AHM-520 exam, data analytics bridges operational performance with strategic foresight. It transforms raw information into actionable intelligence, enabling professionals to predict trends, identify inefficiencies, and make evidence-based decisions.
Operational analytics monitors performance indicators such as claims volume, processing time, and error frequency. These insights allow managers to pinpoint bottlenecks and optimize staffing levels or process flow.
Predictive analytics extends further, using statistical models to forecast future events such as claims surges or emerging patterns of fraud. When properly integrated, predictive analytics allows proactive rather than reactive management.
Equally critical is descriptive analytics, which helps professionals understand historical data trends. For instance, examining seasonal variations in claim submissions or regional differences in utilization can inform resource allocation and policy design.
While data analytics enhances precision, it also introduces ethical and regulatory considerations. Insurers must ensure data accuracy, protect consumer privacy, and comply with data-handling regulations. Analytical power must always be tempered by accountability and transparency.
The Intersection of Technology and Human Expertise
Technology has reshaped every dimension of health insurance, from policy issuance to claims adjudication. Yet despite automation’s transformative power, human expertise remains irreplaceable.
Digital platforms now enable customers to enroll online, access claims data in real time, and communicate directly with service representatives. Artificial intelligence assists underwriters in evaluating risk profiles, while robotic process automation accelerates repetitive administrative tasks.
However, technology must be viewed as an enabler, not a substitute for professional judgment. Systems can process information, but they cannot replicate empathy, ethical reasoning, or contextual interpretation. The AHIP AHM-520 exam recognizes this distinction, emphasizing that professionals must understand technology’s potential while safeguarding human oversight.
The integration of technology demands change management—the structured approach to guiding individuals and organizations through transformation. Employees must receive training, communication, and support to adapt effectively to new systems. Resistance to change, if unaddressed, can undermine even the most sophisticated technological investments.
Therefore, candidates must understand that technological adoption requires both operational strategy and cultural sensitivity. When harmonized correctly, human expertise and digital tools create a synergy that elevates efficiency, accuracy, and consumer satisfaction.
Measuring Consumer Experience and Engagement
Operational excellence ultimately manifests in consumer satisfaction. Health insurance, though complex and technical, remains a service industry whose credibility depends on policyholders’ trust. Measuring and managing consumer experience is therefore an essential competency for professionals and a key theme in the AHIP AHM-520 exam.
Consumer experience encompasses all interactions between a policyholder and the insurer—enrollment, communication, claims processing, and problem resolution. Each interaction influences perception and loyalty.
Organizations measure consumer satisfaction through surveys, feedback forms, and service metrics such as Net Promoter Scores. These data reveal not only performance gaps but also opportunities for innovation.
Engagement goes beyond satisfaction. It reflects the degree to which consumers feel informed, valued, and empowered. Digital platforms that allow policyholders to track benefits, submit claims electronically, or access health education resources enhance engagement and transparency.
Candidates should understand the link between consumer experience and regulatory compliance. Many state and federal regulations now incorporate service quality standards, requiring insurers to meet defined benchmarks in communication and response times.
In a competitive marketplace, superior service becomes a strategic differentiator. Insurers that prioritize transparency and empathy gain reputational strength and customer retention, reinforcing both ethical and economic sustainability.
Workforce Development and Organizational Learning
Behind every successful insurance organization stands a skilled and adaptable workforce. Operational excellence depends on employees who possess both technical proficiency and ethical judgment.
The AHIP AHM-520 exam underscores the importance of human capital development in sustaining organizational success. Continuous education ensures that employees remain current with evolving regulations, technologies, and market dynamics.
Training programs should extend beyond technical skills. They must include modules on ethical decision-making, customer communication, and cultural sensitivity. These soft skills often determine the quality of consumer interaction and organizational culture.
Knowledge management systems preserve institutional memory by documenting best practices, case studies, and procedural guidelines. When employees share knowledge freely, the organization becomes more resilient and innovative.
Performance appraisals, mentoring, and professional development opportunities motivate employees to pursue excellence. Recognition of achievement reinforces desired behaviors, transforming individual ambition into collective progress.
An organization that invests in its workforce builds not only competence but also loyalty. Employees who feel valued become ambassadors of integrity and service excellence.
Strategic Alignment and the Pursuit of Sustainable Growth
Operational excellence must serve a larger purpose—the achievement of sustainable growth. Sustainability in health insurance involves financial stability, regulatory compliance, social responsibility, and innovation.
Strategic alignment ensures that operational decisions support broader organizational objectives. For instance, process improvement initiatives should not only reduce costs but also enhance policyholder satisfaction and regulatory compliance.
The AHIP AHM-520 exam encourages candidates to see the interdependence between strategy and operations. Strategic vision defines the destination; operational excellence determines the path.
Sustainability also implies adaptability. The healthcare industry is in constant flux due to demographic changes, technological advancements, and policy reforms. Organizations that cultivate flexibility within their operations can adjust swiftly without sacrificing quality or integrity.
Furthermore, sustainability encompasses environmental and social responsibility. Many insurers now implement digital workflows to reduce paper usage or support community health initiatives that promote preventive care. These efforts reflect a broader understanding of the insurer’s role as a societal steward rather than merely a financial intermediary.
Preparing Mentally and Strategically for the AHIP AHM-520 Exam
The AHIP AHM-520 exam is not merely an assessment of knowledge but a measure of how effectively candidates can synthesize, apply, and reason through complex concepts under timed conditions. Mental preparedness, strategic planning, and systematic test-taking are essential for success.
For candidates, the first step in preparation is understanding the cognitive and emotional demands of the exam. It requires sustained concentration, analytical precision, and adaptability. Recognizing this challenge allows individuals to approach study and test-day strategy with intentionality rather than anxiety.
Constructing a Pre-Exam Routine
Establishing a consistent pre-exam routine can significantly influence performance. The routine encompasses preparation in the days, hours, and minutes leading up to the test.
In the days preceding the exam, candidates should focus on consolidation rather than intensive learning. Reviewing key concepts, summarizing notes, and completing practice questions strengthens recall without overloading the mind. Cognitive science suggests that spacing study sessions and revisiting material in intervals improves retention and reduces mental fatigue.
On the night before the exam, adequate sleep is critical. Sleep facilitates memory consolidation and cognitive processing, ensuring that information learned during preparation is accessible during the test. Disrupted sleep, conversely, can impair judgment, concentration, and problem-solving ability.
On exam day, a structured morning routine can reduce stress and increase alertness. Balanced nutrition, hydration, and brief physical activity enhance focus and energy. Arriving early at the testing center allows time for acclimatization and minimizes anxiety caused by last-minute delays.
Understanding the Exam Structure
A deep understanding of the AHIP AHM-520 exam structure is essential for effective time management and strategic answering. The exam typically assesses multiple competencies, including underwriting, pricing, risk assessment, financial management, operational processes, and compliance knowledge.
Familiarity with the exam blueprint allows candidates to anticipate the distribution of topics, weighting of questions, and complexity levels. Understanding this structure enables prioritization—allocating more time to sections with higher point values or those historically more challenging.
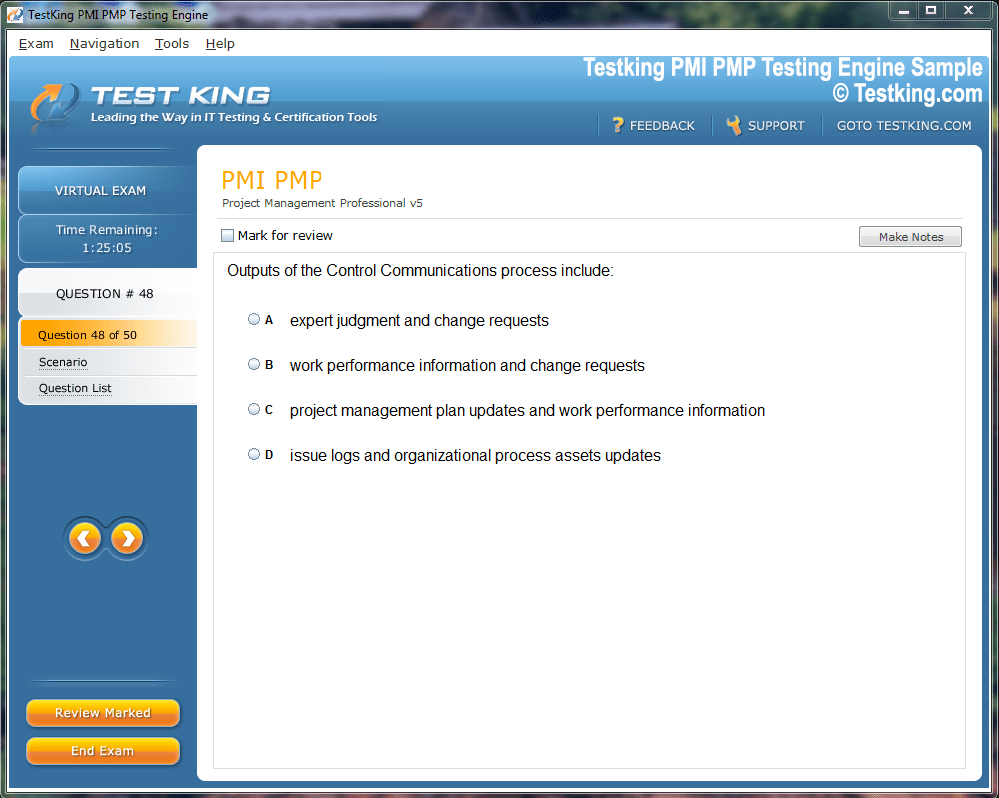
Practice exams simulate the timing, format, and question types encountered in the actual test. They serve multiple purposes: reinforcing content knowledge, improving pacing, and familiarizing candidates with the cognitive demands of the exam. Repeated exposure to practice questions reduces uncertainty and builds confidence.
Analyzing performance on practice exams is as critical as taking them. Identifying recurring errors, misunderstood concepts, or timing bottlenecks allows targeted remediation before the exam day. This reflective approach maximizes learning efficiency and enhances overall performance.
Time Management and Strategic Question Navigation
Time management is often the decisive factor in high-stakes examinations. Even well-prepared candidates may falter if they misallocate time or dwell excessively on individual questions.
A recommended approach is to divide the exam duration proportionally across sections, with built-in flexibility for challenging questions. Initial questions should be addressed efficiently to secure points while preserving mental energy for complex problem-solving later.
Candidates should also apply triage strategies. If a question is unclear or unusually difficult, it is often more effective to mark it for review and proceed, rather than becoming fixated. Returning to it after addressing more manageable questions optimizes scoring potential.
Answering strategy should balance accuracy and speed. Multiple-choice questions may include distractors designed to test comprehension and reasoning. Careful reading, elimination of implausible options, and consideration of regulatory or ethical implications increase the likelihood of selecting correct answers.
Additionally, time should be reserved for review. Revisiting marked questions and verifying calculations or interpretations can prevent avoidable errors and reinforce confidence in responses.
Test-Taking Techniques for Multiple-Choice Questions
Multiple-choice questions dominate the AHIP AHM-520 exam format. While they may appear straightforward, they are designed to assess reasoning, not rote recall. Strategic approaches maximize the probability of success.
Elimination of distractors is a fundamental tactic. Each question contains plausible options; careful analysis allows removal of clearly incorrect choices, narrowing focus to the most viable answer.
Answering in context is also important. Candidates should consider regulatory, operational, and ethical principles when evaluating options. An answer that is mathematically correct but inconsistent with compliance standards or operational best practices is likely incorrect.
Time management strategies are essential here. Spending excessive time on one complex question can jeopardize completion of easier items later. Triage techniques—marking and revisiting challenging questions—optimize overall scoring potential.
Another approach is logical inference. Even if a candidate does not recall a fact precisely, reasoning based on principles, patterns, and deductive logic often identifies the most likely answer.
Conclusion
Successfully preparing for and passing the AHIP AHM-520 exam requires a comprehensive understanding of the health insurance industry, encompassing regulatory frameworks, risk management, financial integrity, operational excellence, and ethical decision-making. The exam evaluates not only technical knowledge but also the ability to integrate concepts across multiple domains, interpret complex scenarios, and apply professional judgment under timed conditions.
Preparation begins with mastering foundational concepts, including underwriting principles, pricing strategies, claims management, and regulatory compliance. Equally important is the cultivation of analytical skills, operational awareness, and familiarity with practical tools such as data analytics, performance metrics, and quality assurance frameworks. Candidates must synthesize these disciplines to address multi-step problems, scenario-based questions, and integrative exercises effectively.
Equally vital is exam-day readiness. Time management, cognitive strategies, stress control, and strategic navigation of questions all contribute to performance. Mental preparation and structured routines reduce anxiety, maintain focus, and optimize recall during the exam. Candidates benefit from practice tests, reflective learning, and deliberate problem-solving to reinforce knowledge and confidence.
Ultimately, success in the AHIP AHM-520 exam reflects a combination of intellectual rigor, ethical discernment, operational insight, and strategic thinking. Mastery of these principles not only ensures favorable exam outcomes but also equips professionals to contribute meaningfully to the health insurance industry. By integrating technical knowledge, analytical reasoning, and ethical standards, candidates emerge prepared for both the exam and the broader challenges of a dynamic, complex healthcare environment.