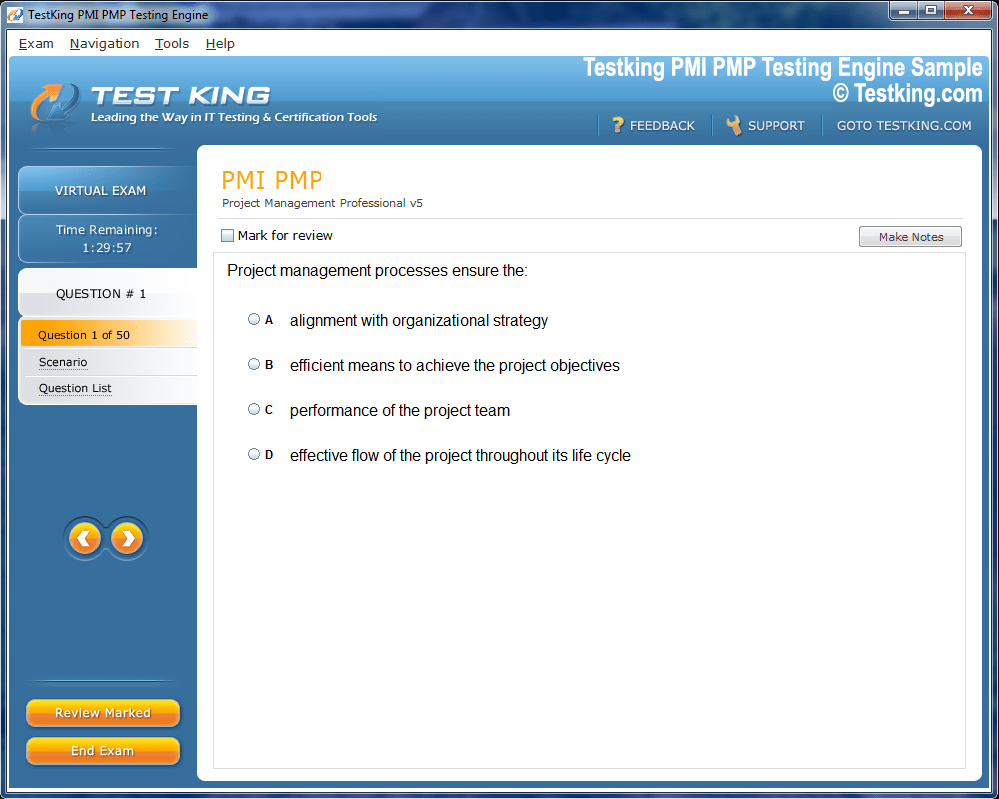
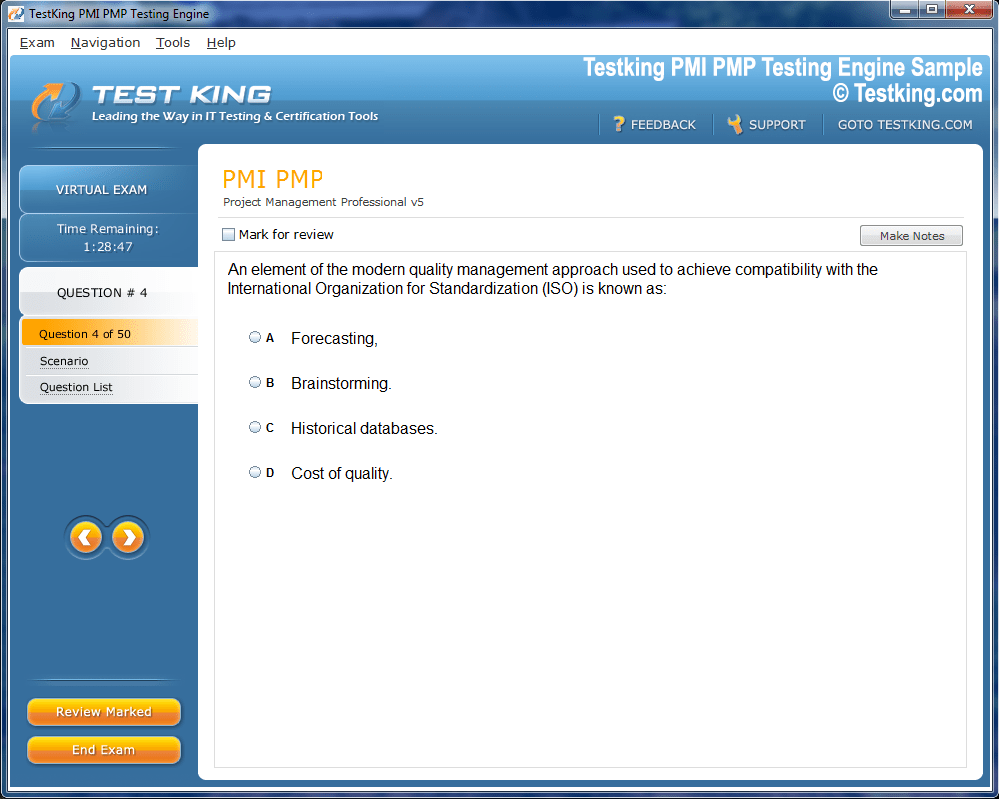
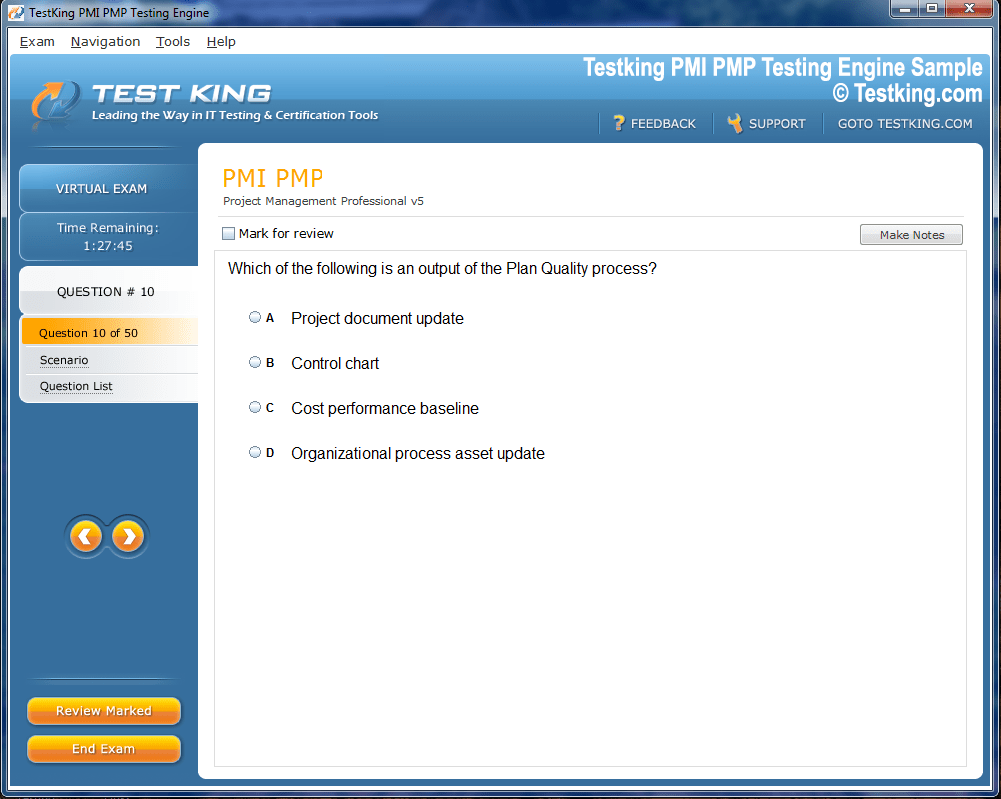
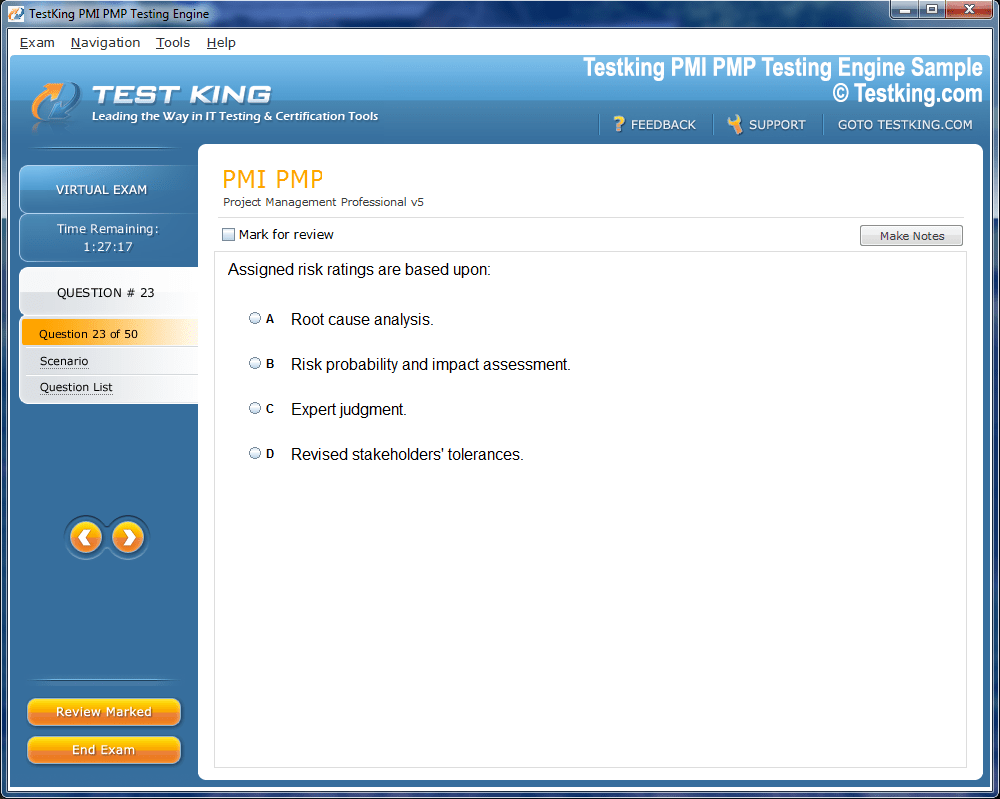
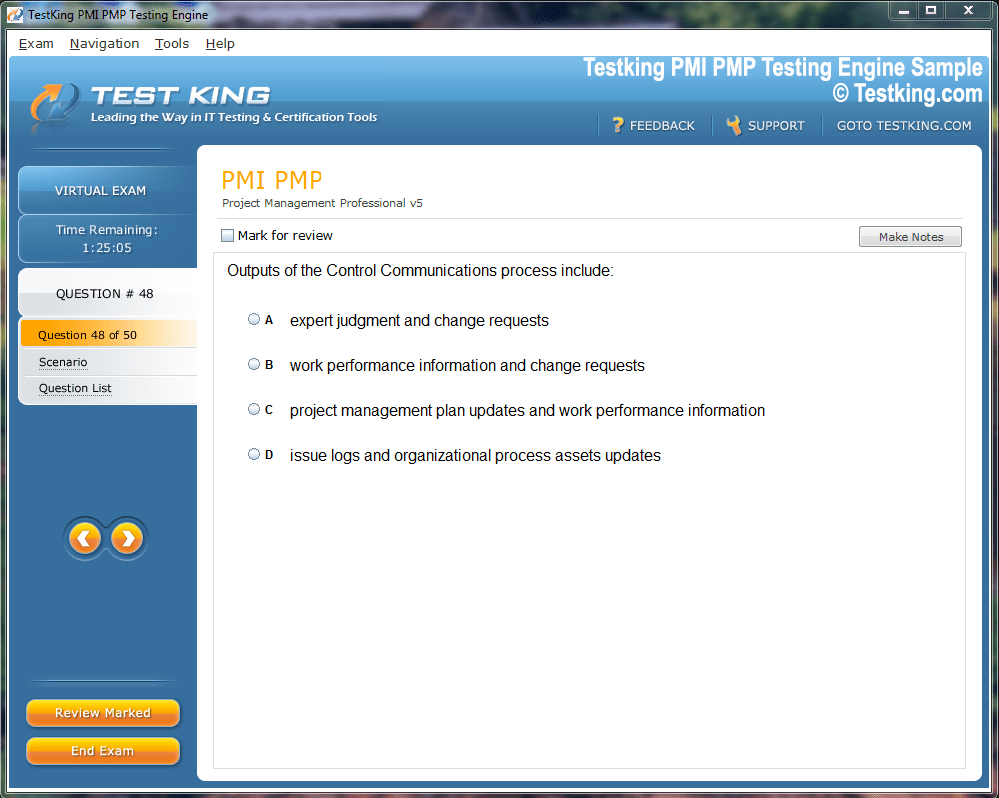
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our AHM-250 testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Top AHIP Exams
AHIP AHM-250 Mastering Health Plans and Administrative Skills
Healthcare management has evolved into a multifaceted discipline that integrates administrative acumen with a thorough understanding of healthcare systems, insurance mechanisms, and regulatory frameworks. The complexity of the modern healthcare ecosystem necessitates professionals who are adept not only in operational procedures but also in the philosophical and ethical dimensions of the industry. The AHIP AHM-250 examination, formally titled Healthcare Management: An Introduction, serves as a benchmark for measuring the proficiency of candidates in these essential areas. This self-study program allows participants to engage in comprehensive preparation at their own pace, providing a structured path to mastering foundational concepts and practical applications in healthcare management.
The AHM-250 exam is designed to assess a wide spectrum of knowledge about health insurance plans, their underlying principles, and the lexicon commonly utilized within the sector. It evaluates understanding of various types of health insurance products, the operational intricacies of healthcare organizations, and the impact of legislative and regulatory interventions on plan administration. Furthermore, it probes the ethical considerations intrinsic to the industry, compelling candidates to cultivate an awareness of moral dilemmas and decision-making paradigms that influence healthcare delivery and policy.
Scope of Health Insurance Knowledge in the AHM-250 Exam
A central component of the AHIP AHM-250 program is its emphasis on health insurance literacy. Candidates are expected to demonstrate a grasp of the diverse array of plans available in the marketplace, ranging from traditional indemnity plans to contemporary managed care arrangements. Understanding the structural and functional distinctions among these plans is essential for anyone aspiring to a leadership role within the healthcare sector. This includes familiarity with plan benefits, enrollment procedures, risk-sharing mechanisms, and cost-containment strategies.
Moreover, the exam addresses the operational domains of health plans, encompassing areas such as claims administration, utilization management, network design, and provider relations. Candidates must appreciate how these operational elements coalesce to ensure the efficiency and sustainability of healthcare delivery. By engaging with these concepts, examinees gain insights into the logistical and strategic considerations that underpin effective health plan management, equipping them to navigate the complexities of organizational operations.
The Philosophical and Ethical Foundations of Healthcare
Healthcare management is not solely a technical or procedural endeavor; it is also guided by philosophical and ethical principles that shape organizational culture and decision-making. The AHIP AHM-250 exam incorporates questions that challenge candidates to consider the moral implications of administrative choices, resource allocation, and policy implementation. Ethical competence in healthcare involves recognizing conflicts of interest, ensuring equitable access to services, and maintaining integrity in interactions with patients, providers, and regulatory bodies.
The examination encourages candidates to reflect on scenarios that may involve competing priorities, such as cost efficiency versus patient-centered care or adherence to regulatory mandates versus innovation in service delivery. Developing an ethical framework enhances managerial judgment and fosters accountability, both of which are critical attributes for professionals operating in dynamic healthcare environments. This dimension of the AHM-250 program distinguishes it from purely procedural training, as it underscores the importance of principled leadership in the health insurance industry.
Legislative and Regulatory Awareness
The influence of legislation and regulation on healthcare operations cannot be overstated. Policies enacted at the federal, state, and local levels shape the structure, funding, and permissible activities of health plans. Candidates preparing for the AHM-250 examination must cultivate an awareness of the regulatory landscape, including statutes that govern insurance coverage, privacy, consumer protection, and reimbursement practices. Understanding the ramifications of these regulations enables managers to anticipate compliance challenges and implement strategies that align with legal requirements.
In addition to compliance, candidates learn to analyze how policy changes affect strategic planning and operational priorities. For example, modifications in reimbursement models, reporting obligations, or benefit mandates may necessitate adjustments in network management, claims processing, or member education initiatives. By mastering these concepts, healthcare professionals can proactively address regulatory shifts, thereby mitigating operational risks and enhancing organizational resilience.
Target Audience for the AHM-250 Examination
The AHM-250 examination is relevant to a diverse cohort of professionals whose roles intersect with healthcare administration and health insurance management. Employees within healthcare provider organizations or insurance companies can leverage the knowledge gained through this program to qualify for supervisory or managerial positions. Case administrators and medical directors benefit from expanding their administrative acumen, allowing them to engage more effectively with operational and strategic decision-making processes.
Educators in healthcare administration programs also gain from familiarity with the AHM-250 curriculum, as it enriches their teaching content with practical insights and current industry standards. Insurance agents and brokers specializing in life and health insurance can enhance their understanding of plan structures and regulatory constraints, improving their advisory capacity for clients. Financial executives managing health-related expenditures are better equipped to optimize resource allocation and client strategies when conversant with plan intricacies. Finally, employees involved in medical management within hospitals, health systems, or insurance plans gain a holistic perspective on operational integration, compliance, and ethical oversight.
Study Materials and Preparation Strategies
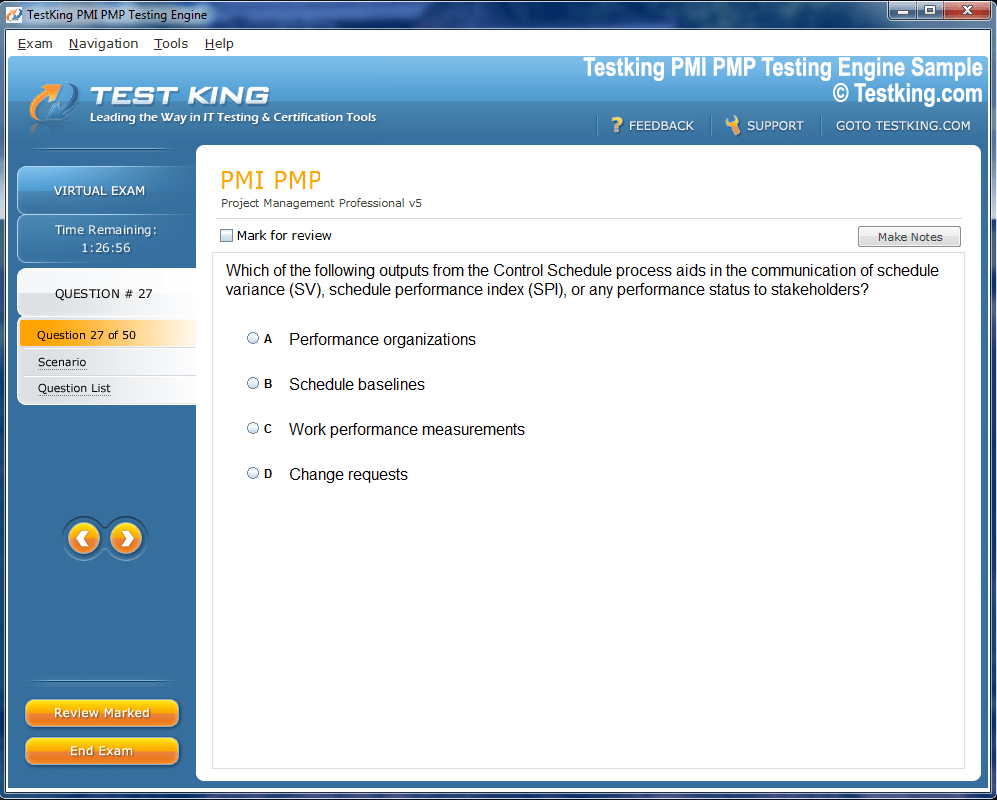
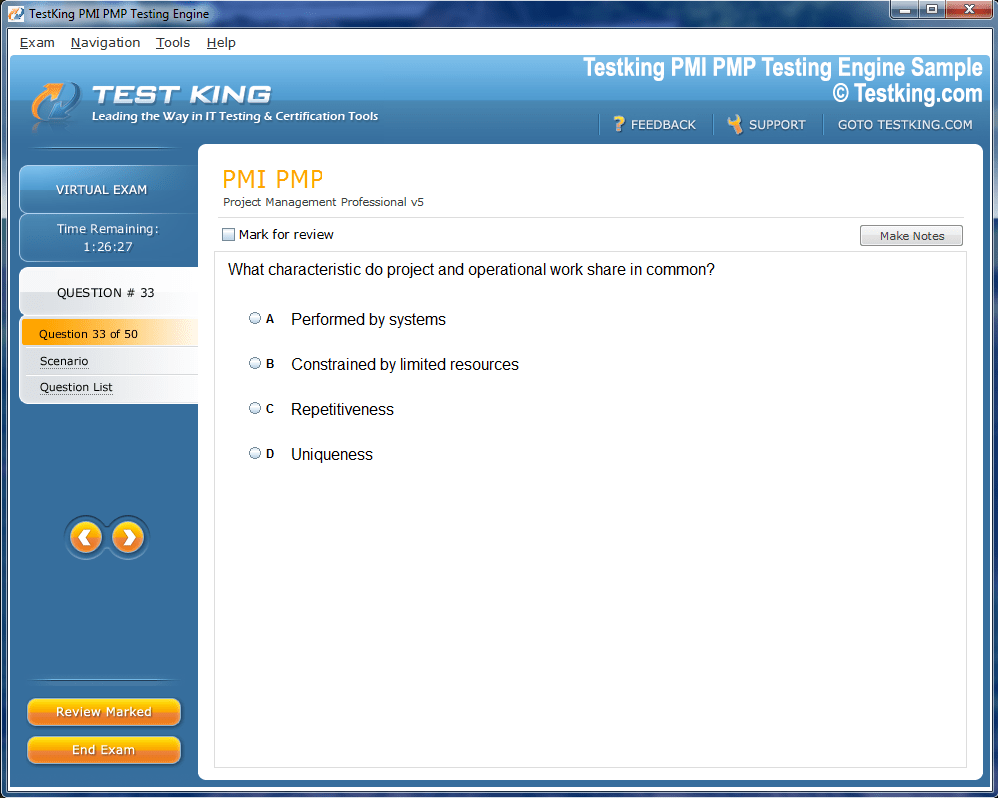
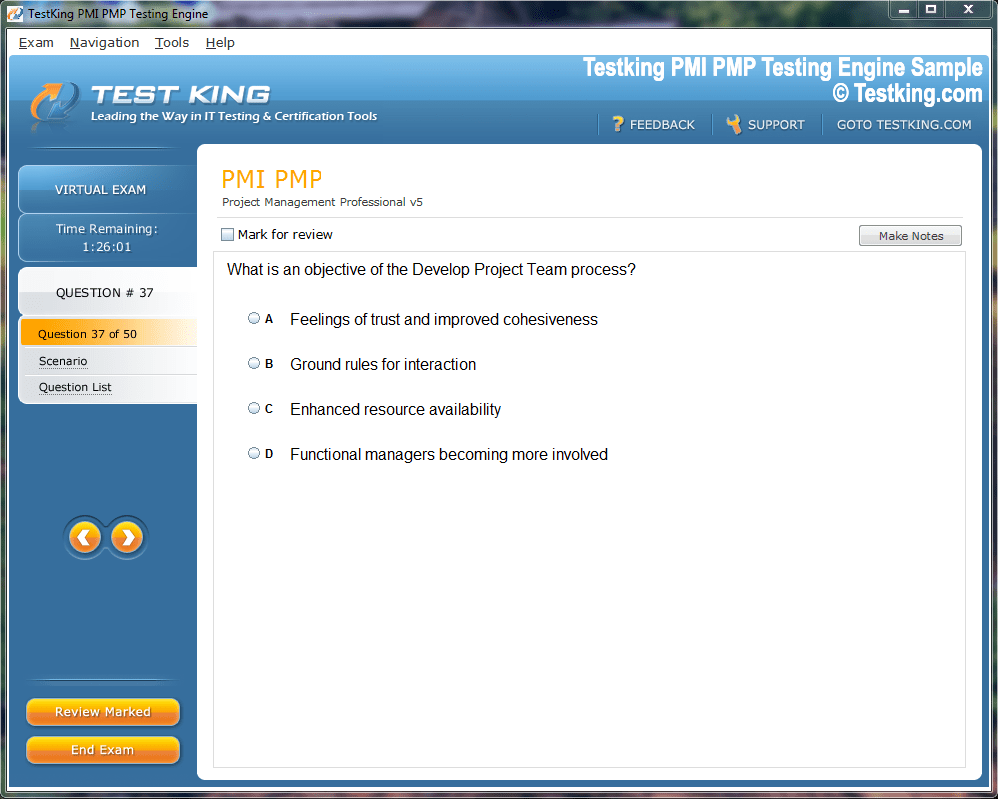
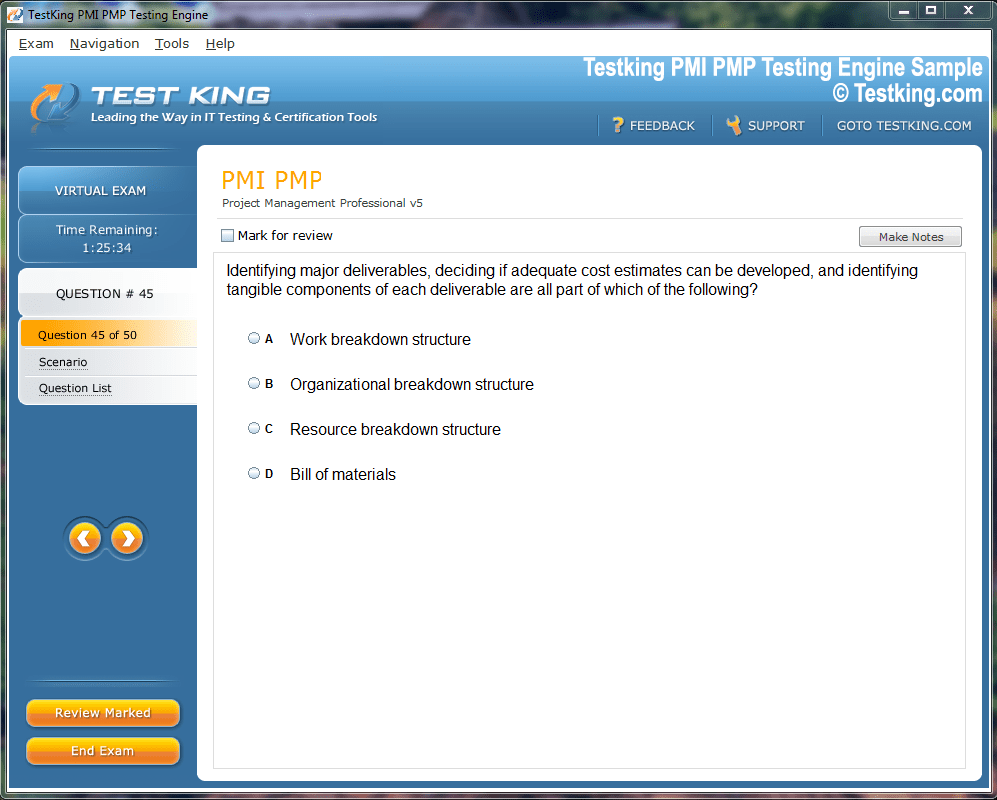
Preparation for the AHM-250 exam necessitates a disciplined approach that combines conceptual comprehension with practical application. Study materials designed for the examination are structured to reflect the current syllabus and incorporate real-world scenarios to illustrate complex concepts. Regular updates ensure alignment with any modifications to exam content, thereby maintaining the relevance and accuracy of practice questions. Candidates benefit from engaging with these materials through repeated review, scenario-based exercises, and self-assessment tools that reinforce retention and application.
The practice exams associated with the AHM-250 program simulate the format and style of actual test questions, enabling candidates to familiarize themselves with time management and question interpretation. By engaging in iterative practice, examinees can identify knowledge gaps, refine analytical skills, and build confidence in navigating diverse question types. This methodical approach enhances the likelihood of success while promoting a deeper understanding of healthcare management principles.
Practical Implications of AHM-250 Knowledge
Mastery of the content assessed in the AHM-250 examination has tangible implications for professional practice. A thorough understanding of health insurance plans and operational processes enables managers to design, implement, and evaluate programs that enhance efficiency, quality, and member satisfaction. Regulatory literacy ensures that organizational activities adhere to legal mandates, reducing exposure to penalties and reputational risks. Ethical competence fosters trust among stakeholders, reinforcing the credibility of management decisions and strengthening organizational culture.
Additionally, the insights gained from the AHM-250 program facilitate strategic planning and problem-solving within healthcare organizations. Managers equipped with this knowledge can anticipate industry trends, assess the impact of policy changes, and implement innovations that improve service delivery. The combination of technical proficiency, ethical awareness, and regulatory understanding forms a comprehensive skill set that is indispensable for contemporary healthcare leadership.
Enhancing Analytical and Decision-Making Skills
The AHM-250 examination emphasizes the development of analytical and decision-making capabilities essential for effective healthcare management. Candidates are encouraged to interpret data, evaluate operational performance, and formulate evidence-based recommendations. This analytical rigor extends to financial analysis, resource allocation, and risk management, all of which are integral to sustaining health plan operations. By cultivating these skills, professionals can navigate complex scenarios with informed judgment, balancing operational efficiency with patient-centered objectives.
Case studies and scenario-based questions within the exam framework challenge examinees to apply theoretical knowledge to practical situations. This experiential learning approach enhances critical thinking, enabling candidates to synthesize information from multiple sources, weigh alternatives, and arrive at judicious conclusions. Such capabilities are particularly valuable in dynamic healthcare environments where rapid decision-making and adaptive strategies are frequently required.
Ethical Challenges and Professional Responsibility
The healthcare sector frequently presents situations where ethical considerations intersect with managerial responsibilities. Professionals may confront dilemmas related to resource distribution, patient privacy, conflict of interest, or regulatory compliance. The AHM-250 exam introduces these scenarios to cultivate a nuanced understanding of professional responsibility. Candidates learn to navigate competing priorities while upholding ethical standards, promoting equitable treatment, and fostering transparency in organizational operations.
Ethical competence also encompasses proactive engagement with emerging issues such as data security, telehealth expansion, and healthcare disparities. By anticipating ethical implications and formulating appropriate responses, healthcare managers contribute to the sustainability and credibility of their organizations. This emphasis on moral reasoning complements technical and operational expertise, producing well-rounded professionals capable of leading with integrity.
The Role of Legislation and Policy Interpretation
A robust comprehension of legislative and policy frameworks is critical for effective healthcare management. Candidates are expected to recognize the implications of federal and state statutes, including those that govern insurance coverage, reimbursement structures, and consumer protection. The ability to interpret and operationalize regulatory requirements ensures compliance and informs strategic decision-making, enabling organizations to respond effectively to evolving mandates.
In practice, this involves understanding how policy changes impact operational areas such as network management, benefit design, and member services. Managers must anticipate regulatory shifts, assess potential consequences, and implement mitigation strategies to maintain service quality and organizational stability. This proactive approach reflects the integration of legal awareness with operational and ethical considerations, underscoring the multidimensional nature of healthcare management.
Comprehensive Overview of Health Insurance Plans
A critical component of healthcare management involves an intricate understanding of the diverse array of health insurance plans available in the contemporary market. These plans, each with distinct structures, benefits, and regulatory obligations, constitute the backbone of healthcare financing and delivery. The AHIP AHM-250 examination emphasizes the ability to differentiate among plan types, comprehend their operational modalities, and anticipate the implications for both enrollees and providers. Candidates are encouraged to explore the nuances of indemnity plans, preferred provider organizations, health maintenance organizations, and consumer-directed arrangements, among others, while recognizing how these frameworks respond to evolving healthcare demands.
Indemnity plans, for instance, operate on a fee-for-service basis, allowing patients substantial freedom in selecting providers while often imposing deductibles and coinsurance. In contrast, managed care models, such as health maintenance organizations, emphasize network utilization, preventive care, and cost containment strategies. Preferred provider organizations combine elements of flexibility and network-based cost controls, balancing patient autonomy with financial prudence. Consumer-directed health plans introduce high-deductible structures paired with health savings accounts, empowering members to make informed financial and healthcare choices while encouraging personal responsibility.
Operational Complexities of Health Plans
Operational proficiency is paramount for professionals preparing for the AHM-250 examination. The administration of health plans involves an array of interdependent processes that ensure the efficient delivery of services, accurate claims processing, and member satisfaction. Candidates must acquire a robust understanding of these operational domains, including utilization review, provider network management, benefit design, and actuarial assessment. Each function necessitates meticulous attention to detail, coordination across departments, and adherence to regulatory requirements, highlighting the complexity of health plan administration.
Claims processing, for instance, requires accurate verification, adjudication, and timely reimbursement to both providers and enrollees. Errors or delays can undermine organizational credibility and lead to financial liabilities. Utilization management, on the other hand, evaluates the necessity, appropriateness, and efficiency of services rendered, ensuring that care aligns with clinical guidelines and cost considerations. Provider network management entails negotiating contracts, maintaining quality standards, and monitoring performance, balancing the interests of the organization and its members. These operational elements interconnect to form a cohesive system that underpins the effective functioning of health plans.
Legislative Implications on Health Plan Management
Legislation exerts a profound influence on the operational, financial, and ethical dimensions of healthcare management. The AHIP AHM-250 program places considerable emphasis on the understanding of legal frameworks, regulatory compliance, and policy interpretation. Candidates are expected to examine how statutes, such as those governing insurance coverage, privacy, and reimbursement, shape organizational behavior, resource allocation, and strategic planning. An awareness of legislative developments enables professionals to anticipate operational adjustments, mitigate risks, and align management practices with statutory obligations.
Healthcare policy shifts may introduce changes in reimbursement structures, reporting requirements, or eligibility criteria, necessitating swift organizational responses. For example, modifications in Medicaid or Medicare provisions can impact provider contracts, payment models, and member enrollment procedures. Understanding the interrelation between legislative mandates and operational execution allows managers to implement proactive strategies, ensuring that organizational objectives harmonize with regulatory compliance. By mastering this domain, candidates develop the foresight required for effective healthcare leadership.
Ethical Considerations in Healthcare Administration
Ethical reasoning constitutes an essential pillar of healthcare management, informing decision-making processes and shaping organizational culture. The AHM-250 examination explores ethical dilemmas that professionals may encounter, such as balancing cost containment with patient-centered care, addressing disparities in access, and managing conflicts of interest. Developing ethical literacy equips candidates with the skills to navigate morally complex situations while maintaining professional integrity and organizational accountability.
Ethical challenges extend beyond routine operational decisions, encompassing issues related to privacy, data security, informed consent, and equitable resource allocation. For instance, healthcare managers may confront scenarios in which budgetary constraints necessitate prioritization of certain services, potentially impacting vulnerable populations. Ethical acumen enables leaders to evaluate alternatives, consider stakeholder implications, and implement policies that uphold fairness and transparency. By internalizing these principles, professionals contribute to an organizational ethos that prioritizes trust, integrity, and social responsibility.
Targeted Candidates for the AHIP AHM-250 Program
The AHIP AHM-250 examination serves a diverse population of healthcare professionals seeking to augment their administrative, operational, and strategic competencies. Employees within healthcare provider organizations, insurance companies, and health systems often leverage the program to advance into management positions. Case administrators and medical directors benefit from exposure to comprehensive administrative frameworks, enhancing their capacity to make informed decisions across multiple operational domains.
Educators specializing in healthcare administration gain insight into contemporary industry practices, enriching the curriculum offered to students and bridging the gap between theory and practice. Insurance agents and brokers, particularly those focused on life and health products, acquire nuanced knowledge of plan structures, regulatory parameters, and operational intricacies, enabling them to advise clients more effectively. Financial executives managing client resources develop a deeper understanding of cost-containment strategies, reimbursement models, and policy implications. Collectively, these professionals emerge better prepared to navigate the complex landscape of healthcare management.
Study Resources and Preparation Techniques
Effective preparation for the AHM-250 exam necessitates engagement with comprehensive study materials and practice tools designed to reflect current industry standards and exam content. These resources encompass detailed explanations of health plan types, operational processes, regulatory frameworks, and ethical considerations, offering candidates a holistic understanding of healthcare management. The inclusion of scenario-based exercises and illustrative examples promotes experiential learning, enhancing the ability to apply theoretical concepts to real-world contexts.
Practice exams constitute an integral component of preparation, simulating the structure and style of the actual test. By interacting with these tools, candidates gain familiarity with time management, question interpretation, and analytical evaluation. Repeated practice reinforces knowledge retention and cultivates confidence, enabling examinees to approach the examination with both competence and composure. Additionally, the continuous updating of study materials ensures alignment with any modifications in exam content, enhancing the relevance and efficacy of preparation efforts.
Practical Applications of Exam Knowledge
The competencies assessed in the AHM-250 examination have direct relevance to professional practice, informing both operational management and strategic decision-making. A comprehensive understanding of health insurance plans, operational workflows, and regulatory requirements enables managers to design and implement programs that optimize efficiency, quality, and member satisfaction. Ethical awareness further enhances organizational integrity, fostering trust among patients, providers, and stakeholders.
In practical terms, mastery of exam content facilitates proactive problem-solving, informed policy implementation, and effective resource allocation. Managers can anticipate industry trends, evaluate the potential impact of regulatory changes, and devise strategies that align organizational objectives with broader healthcare priorities. This integrated approach underscores the value of the AHM-250 program in cultivating professionals capable of balancing operational exigencies with ethical, financial, and regulatory considerations.
Developing Analytical and Strategic Thinking
Analytical and strategic thinking are central to effective healthcare management, enabling professionals to navigate complex operational and policy environments. The AHM-250 exam challenges candidates to interpret data, assess organizational performance, and formulate evidence-based recommendations. These skills extend across financial analysis, risk assessment, and operational optimization, contributing to the sustained efficacy of health plan operations.
Scenario-based questions encourage candidates to evaluate multiple perspectives, synthesize information from disparate sources, and apply reasoning to arrive at judicious conclusions. This iterative process of analysis and evaluation strengthens critical thinking and enhances decision-making capabilities, equipping professionals to respond adaptively to emerging challenges in healthcare administration. The integration of analytical rigor with operational insight is a distinguishing feature of the AHM-250 examination, fostering a cadre of professionals proficient in both theory and practice.
Ethical Decision-Making in Complex Scenarios
Healthcare professionals often encounter situations where ethical considerations intersect with operational imperatives, requiring careful deliberation and judgment. The AHM-250 exam emphasizes ethical decision-making, highlighting scenarios in which conflicting priorities may arise, such as balancing cost efficiency with patient-centered outcomes or reconciling regulatory compliance with innovative care delivery. Candidates are trained to evaluate alternatives, consider stakeholder implications, and implement solutions that uphold ethical standards while achieving organizational objectives.
Ethical decision-making also encompasses emerging issues such as telehealth expansion, data privacy, and healthcare equity. By engaging with these topics, candidates cultivate the ability to anticipate potential challenges, develop policies that mitigate risk, and promote transparency and accountability. This ethical orientation complements operational expertise, producing healthcare managers equipped to lead responsibly and sustainably in complex environments.
Interrelation of Legislation, Operations, and Ethics
A nuanced understanding of healthcare management necessitates recognizing the interplay among legislation, operational processes, and ethical principles. Legislative mandates influence organizational operations, shaping workflows, reimbursement structures, and compliance protocols. Simultaneously, ethical considerations inform the application of these mandates, guiding decision-making to ensure fairness, equity, and integrity.
Professionals who grasp these interconnections can implement policies that harmonize legal compliance, operational efficiency, and ethical accountability. This holistic perspective enhances organizational performance, mitigates risk, and reinforces stakeholder trust. The AHM-250 examination fosters this integrated understanding, preparing candidates to approach healthcare management with both strategic foresight and moral discernment.
The Significance of Ethical and Regulatory Proficiency
Proficiency in ethics and regulatory compliance is essential for sustaining organizational credibility and operational effectiveness. Candidates preparing for the AHM-250 exam are encouraged to internalize principles of professional responsibility, equitable treatment, and transparent decision-making. Concurrently, regulatory literacy equips managers to navigate evolving policy landscapes, anticipate compliance challenges, and implement corrective measures proactively.
The combination of ethical discernment and regulatory awareness underpins sound healthcare management, enabling organizations to respond adaptively to industry changes while maintaining public trust. By mastering these competencies, professionals are better positioned to oversee complex operations, guide policy implementation, and foster organizational resilience.
Understanding Health Plan Products and Member Benefits
A fundamental aspect of healthcare management involves a deep comprehension of health plan products and the range of benefits they offer. The AHIP AHM-250 examination emphasizes this domain, expecting candidates to demonstrate knowledge of product design, coverage options, and the financial structures underpinning each plan. Health plans are intricate arrangements that combine cost-sharing mechanisms, network considerations, and service coverage to meet the diverse needs of enrollees. Understanding these elements is crucial for professionals tasked with designing, managing, or evaluating health plan offerings.
Traditional indemnity plans, for instance, typically provide broad provider access while imposing deductibles, coinsurance, and copayments. Managed care products, such as health maintenance organizations and preferred provider organizations, incorporate network restrictions, preventive care protocols, and utilization management strategies to contain costs and optimize care quality. Consumer-directed plans, including high-deductible health plans paired with health savings accounts, encourage enrollees to make informed financial and healthcare decisions. Candidates preparing for the AHM-250 exam must evaluate these products’ structural differences, implications for members, and operational challenges for providers.
Operational Areas of Health Plans
Health plan operations encompass a spectrum of functions essential for delivering services effectively, maintaining compliance, and ensuring member satisfaction. The AHM-250 program covers operational domains such as claims processing, provider network management, utilization review, and member engagement. Candidates are expected to analyze how these functions interrelate, identify inefficiencies, and apply strategies to optimize outcomes.
Claims processing requires precise verification, adjudication, and reimbursement procedures to maintain organizational integrity and member trust. Utilization management evaluates the necessity, appropriateness, and efficiency of services, ensuring that care aligns with clinical guidelines and cost considerations. Provider network management entails contract negotiation, quality monitoring, and performance evaluation, balancing organizational objectives with member access. Member engagement involves communication strategies, educational initiatives, and feedback mechanisms to enhance satisfaction and compliance with plan provisions. Mastery of these operational areas is essential for healthcare managers to oversee complex workflows and support strategic initiatives effectively.
The Impact of Legislation and Regulatory Oversight
Healthcare legislation and regulatory oversight profoundly influence plan design, operational procedures, and strategic decision-making. Candidates for the AHM-250 exam must understand statutory requirements affecting insurance coverage, reimbursement mechanisms, privacy protection, and consumer rights. Regulatory awareness allows managers to anticipate operational adjustments, ensure compliance, and mitigate legal and financial risks.
Policies such as the Affordable Care Act, Medicaid and Medicare provisions, and state-specific insurance regulations shape organizational behavior, network formation, and service delivery. Compliance with reporting requirements, documentation standards, and operational protocols is essential for sustaining organizational credibility and avoiding penalties. Candidates must also assess how emerging policy changes influence resource allocation, workflow adjustments, and strategic priorities, equipping them to navigate the dynamic regulatory environment effectively.
Ethical Considerations in Plan Administration
Ethics play a pivotal role in healthcare management, guiding decision-making, resource allocation, and organizational culture. The AHIP AHM-250 program emphasizes the evaluation of ethical dilemmas, such as balancing financial constraints with patient-centered care or addressing disparities in access to services. Candidates develop frameworks for resolving conflicts of interest, ensuring transparency, and promoting equitable treatment across diverse populations.
Ethical challenges extend to emerging healthcare trends, including telehealth, data privacy, and healthcare equity. Healthcare managers must consider the implications of policy changes, technological advancements, and financial pressures while upholding principles of fairness, integrity, and accountability. The ability to integrate ethical reasoning with operational and strategic decision-making is critical for effective leadership in the complex healthcare environment.
Who Benefits from the AHM-250 Program
The AHM-250 examination is relevant to a broad spectrum of healthcare professionals. Employees of health systems, hospitals, and insurance organizations seeking advancement into managerial roles gain knowledge and skills critical for leadership. Case administrators and medical directors benefit from exposure to administrative, operational, and regulatory principles that enhance their decision-making capabilities.
Educators teaching healthcare administration can incorporate practical insights from the program into their curriculum, bridging theoretical and real-world applications. Insurance agents and brokers specializing in life and health products develop a comprehensive understanding of plan structures, operational processes, and regulatory considerations, improving their advisory capabilities. Financial executives tasked with managing client health resources acquire expertise in cost containment, reimbursement strategies, and benefit optimization. Collectively, these professionals gain the competencies necessary to navigate complex healthcare landscapes with efficacy and ethical awareness.
Applying Exam Knowledge in Professional Practice
Knowledge gained through the AHM-250 program has immediate applicability in professional practice. Mastery of health insurance products, operational workflows, regulatory compliance, and ethical considerations equips managers to design, implement, and evaluate programs that enhance efficiency, quality, and member satisfaction. Ethical competence fosters trust among patients, providers, and stakeholders, reinforcing organizational credibility.
In practical terms, AHM-250 proficiency enables managers to anticipate industry trends, respond to policy changes, optimize resource allocation, and implement effective operational strategies. This holistic approach integrates technical, ethical, and regulatory competencies, allowing professionals to address complex challenges and contribute meaningfully to organizational success.
Ethical Decision-Making in Complex Contexts
Healthcare managers frequently encounter complex ethical scenarios that require careful deliberation. The AHM-250 examination explores challenges such as resource allocation, privacy considerations, compliance conflicts, and equity in service provision. Candidates learn to evaluate alternatives, anticipate consequences, and implement solutions that balance ethical principles with operational and financial realities.
Emerging issues, including the expansion of telehealth services, cybersecurity, and healthcare disparities, require ethical foresight and proactive policy development. By integrating ethical reasoning with operational and strategic expertise, professionals enhance organizational integrity, stakeholder trust, and service quality. Ethical decision-making is not an isolated skill but a critical dimension of comprehensive healthcare management, guiding leaders through multifaceted challenges with prudence and integrity.
Integrating Legislation, Operations, and Ethics
Effective healthcare management requires an integrated understanding of legislation, operational functions, and ethical principles. Regulatory frameworks dictate compliance requirements, while operational processes translate these mandates into actionable workflows. Ethical considerations ensure that decisions are fair, transparent, and aligned with organizational values.
Professionals who grasp these interconnections can implement strategies that harmonize compliance, efficiency, and ethical responsibility. This holistic perspective enhances organizational performance, mitigates risks, and fosters stakeholder confidence. The AHM-250 program cultivates this integrated understanding, preparing candidates to navigate the complexities of healthcare management with strategic insight and ethical discernment.
Enhancing Operational Efficiency
Operational efficiency is central to successful health plan management. Candidates for the AHM-250 exam examine processes such as claims adjudication, provider contracting, utilization review, and member engagement. Optimizing these functions improves resource utilization, reduces administrative burdens, and enhances service quality.
Managers who understand the intricacies of operational workflows can identify inefficiencies, implement best practices, and coordinate activities across departments. This operational literacy supports strategic planning, facilitates seamless service delivery, and ensures compliance with regulatory requirements. Mastery of these concepts enhances practical proficiency and reinforces the relevance of the AHM-250 program in professional contexts.
Strategic Applications of Health Plan Knowledge
The competencies acquired through the AHM-250 program have far-reaching implications for strategic planning and decision-making. Knowledge of plan types, member benefits, operational domains, regulatory frameworks, and ethical principles equips managers to anticipate trends, assess organizational performance, and develop policies that optimize outcomes.
By applying strategic insights, healthcare leaders can enhance operational effectiveness, improve patient and member satisfaction, and ensure alignment with organizational objectives. The program fosters a comprehensive skill set that integrates analytical thinking, operational expertise, and ethical awareness, enabling professionals to navigate the multifaceted challenges inherent in healthcare management.
Ethical and Professional Responsibility
Ethical and professional responsibility remain foundational to healthcare management. Candidates are expected to internalize principles of fairness, transparency, accountability, and equitable treatment. Ethical competence extends to navigating emerging challenges, including telehealth integration, data privacy, and resource prioritization.
Coupled with regulatory awareness, ethical proficiency ensures that managers can guide organizational operations responsibly, maintaining credibility and trust among stakeholders. By balancing operational, financial, regulatory, and ethical considerations, healthcare professionals cultivate the judgment and integrity necessary for effective leadership.
In-Depth Exploration of Health Insurance Plan Types
Healthcare management requires an extensive understanding of the variety of health insurance plans available to consumers. The AHIP AHM-250 examination emphasizes the knowledge of these plans, their unique characteristics, and how they affect both enrollees and healthcare providers. Candidates must explore indemnity plans, health maintenance organizations, preferred provider organizations, and consumer-driven plans to comprehend their operational and financial implications.
Indemnity plans, often referred to as fee-for-service plans, allow patients significant freedom in selecting providers while requiring them to bear deductibles and coinsurance costs. Health maintenance organizations emphasize preventive care, network utilization, and cost containment strategies, creating a framework where services are managed to maintain both quality and affordability. Preferred provider organizations offer flexibility within a contracted provider network, balancing accessibility with financial prudence. Consumer-directed plans, incorporating high-deductible structures with health savings accounts, promote enrollee engagement in healthcare decisions while incentivizing cost awareness. Understanding these distinctions is critical for effective management and informed decision-making.
Operational Competencies in Healthcare Management
Health plan operations are complex and multifaceted, encompassing claims processing, provider network management, utilization review, and member engagement. The AHIP AHM-250 program underscores the necessity of mastering these operational areas to ensure effective service delivery, regulatory compliance, and member satisfaction. Candidates are trained to analyze workflows, identify inefficiencies, and implement strategies that enhance organizational performance.
Claims processing involves verifying service validity, adjudicating coverage, and reimbursing providers and members accurately and promptly. Utilization review assesses the necessity and efficiency of healthcare services, ensuring alignment with clinical guidelines and cost considerations. Provider network management encompasses contract negotiation, performance monitoring, and quality assurance, requiring managers to balance organizational objectives with member access. Member engagement entails communication, education, and feedback mechanisms to maintain satisfaction and adherence to plan provisions. Expertise in these domains is vital for leadership roles that demand operational oversight and strategic planning.
Legislative and Regulatory Impacts on Health Plans
Healthcare legislation and regulatory oversight shape the operational, financial, and strategic dimensions of health plans. Candidates for the AHM-250 exam must understand laws governing coverage, reimbursement, privacy, and consumer protections. Regulatory literacy enables managers to anticipate adjustments, mitigate risk, and ensure compliance while optimizing service delivery.
Policies such as Medicaid, Medicare, and state-specific insurance regulations directly influence plan design, provider contracts, and member access. Compliance with reporting requirements, documentation protocols, and operational standards is critical to maintaining organizational credibility and avoiding penalties. Candidates are also expected to analyze the consequences of legislative changes, assess their operational impact, and implement strategies to maintain efficiency and regulatory alignment. This knowledge equips professionals to navigate a dynamic policy landscape with foresight and precision.
Ethical Frameworks in Healthcare Administration
Ethics is a foundational pillar of healthcare management, guiding decision-making, resource allocation, and organizational culture. The AHIP AHM-250 exam emphasizes ethical reasoning in scenarios such as balancing cost containment with patient-centered care, addressing disparities in access, and managing conflicts of interest. Candidates develop frameworks for transparent, equitable, and principled decision-making.
Ethical challenges also encompass emerging healthcare trends, including telehealth implementation, data privacy concerns, and population health initiatives. Healthcare managers must consider the ethical implications of policy shifts, technological innovations, and financial pressures while ensuring fair treatment and accountability. Integrating ethical reasoning with operational and strategic decision-making strengthens organizational integrity and enhances stakeholder trust.
Target Candidates for the AHIP AHM-250 Program
The AHM-250 program is designed for a broad spectrum of healthcare professionals seeking to enhance administrative, operational, and strategic competencies. Employees within healthcare provider organizations, insurance companies, and health systems can leverage the program to advance into managerial roles. Case administrators and medical directors gain exposure to administrative principles, regulatory frameworks, and operational strategies that improve decision-making capacity.
Educators teaching healthcare administration can integrate practical insights into curricula, bridging the gap between theoretical knowledge and real-world applications. Insurance agents and brokers specializing in life and health products acquire expertise in plan design, operational management, and regulatory compliance, enhancing advisory capabilities. Financial executives managing client resources develop proficiency in cost-containment strategies, benefit optimization, and risk assessment. These professionals collectively benefit from the program, acquiring competencies essential for navigating complex healthcare landscapes.
Study Materials and Preparation Strategies
Preparing for the AHM-250 exam requires engagement with comprehensive study resources that reflect current industry standards and exam content. Materials cover health plan types, operational functions, regulatory frameworks, and ethical considerations. Scenario-based exercises and illustrative examples promote experiential learning, allowing candidates to apply theoretical knowledge in practical contexts.
Practice exams simulate the format, timing, and analytical requirements of the actual test. Repeated engagement with these tools reinforces knowledge retention, sharpens analytical skills, and enhances confidence. Continuous updates to study materials ensure alignment with changes in exam content, maintaining relevance and reliability throughout the preparation process. This structured approach to preparation equips candidates with the competence necessary to excel in both the examination and professional practice.
Applying Knowledge to Professional Practice
The competencies assessed in the AHM-250 program have immediate applicability in professional contexts. Knowledge of health insurance products, operational processes, regulatory frameworks, and ethical principles enables managers to design and implement programs that improve efficiency, quality, and member satisfaction. Ethical competence fosters trust among patients, providers, and stakeholders, reinforcing organizational credibility and sustainability.
Mastery of exam content facilitates strategic decision-making, proactive problem-solving, and resource optimization. Managers can anticipate industry trends, evaluate policy impacts, and implement operational improvements that align with organizational objectives. This integration of knowledge across technical, ethical, and regulatory domains ensures well-rounded professional preparedness and the ability to navigate complex healthcare management challenges.
Analytical and Strategic Thinking in Healthcare
Analytical and strategic thinking are crucial for effective healthcare management. The AHM-250 examination emphasizes skills such as data interpretation, performance evaluation, and evidence-based decision-making. Candidates are trained to apply these skills in financial analysis, operational optimization, risk management, and policy assessment.
Scenario-based questions encourage synthesis of information, evaluation of alternatives, and formulation of judicious solutions. This iterative process strengthens critical thinking, enhances decision-making capabilities, and prepares professionals to respond effectively to operational, regulatory, and ethical challenges. By integrating analytical rigor with operational expertise, the AHM-250 program cultivates professionals capable of strategic leadership and informed judgment in complex healthcare environments.
Advanced Concepts in Healthcare Management
The AHIP AHM-250 program provides a sophisticated framework for understanding healthcare management, emphasizing both foundational principles and advanced operational concepts. Candidates are expected to develop expertise in health plan structures, member benefits, operational domains, regulatory compliance, and ethical considerations. Mastery of these areas enables professionals to address complex challenges, implement strategic initiatives, and contribute to organizational sustainability.
Advanced healthcare management requires the integration of multiple skill sets. Candidates must analyze operational data, interpret regulatory mandates, and evaluate the financial and ethical implications of decisions. This multidimensional approach ensures that healthcare managers are capable of navigating evolving policy landscapes, technological innovations, and shifting patient demographics. The program’s emphasis on critical thinking, analytical reasoning, and ethical judgment equips candidates with the tools necessary for strategic leadership in diverse healthcare settings.
Health Plan Products and Member Engagement
A profound understanding of health plan products is crucial for effective healthcare management. Candidates must be familiar with indemnity plans, health maintenance organizations, preferred provider organizations, and consumer-driven health plans. Each type of plan possesses unique characteristics that influence cost-sharing, network utilization, and member engagement strategies.
Member engagement is a central focus of operational effectiveness. Healthcare managers must implement communication strategies, educational programs, and feedback mechanisms to enhance participation, adherence, and satisfaction. High levels of engagement improve outcomes, reduce administrative inefficiencies, and foster positive relationships between members, providers, and the organization. The AHM-250 program underscores the importance of linking product knowledge with engagement strategies to achieve both clinical and operational objectives.
Operational Domains in Healthcare Organizations
Operational expertise is a cornerstone of healthcare management. Candidates examine processes such as claims adjudication, provider network administration, utilization review, and member services management. Each operational domain requires meticulous attention to detail, coordination across departments, and adherence to regulatory and ethical standards.
Claims adjudication involves verifying service validity, processing payments accurately, and maintaining timely reimbursement. Provider network administration ensures that contracted providers meet quality standards and performance expectations. Utilization review evaluates the necessity and efficiency of services, aligning clinical interventions with cost and quality considerations. Member services management focuses on satisfaction, education, and accessibility, enhancing both compliance and engagement. Mastery of these operational domains enables managers to optimize workflows and support organizational strategy effectively.
The Influence of Legislation and Regulation
Legislative frameworks profoundly affect health plan operations, product design, and organizational strategy. Candidates for the AHM-250 exam must understand regulatory requirements related to coverage, reimbursement, privacy, and consumer protection. Knowledge of these mandates ensures compliance, reduces risk, and informs operational decision-making.
Healthcare managers must evaluate the impact of regulatory changes on workflow, financial performance, and member experience. Policies such as Medicaid, Medicare, and state-specific insurance regulations directly shape plan operations, network formation, and benefit structures. By integrating regulatory knowledge with operational expertise, managers can implement proactive strategies that maintain compliance, improve efficiency, and enhance organizational resilience.
Ideal Candidates for the AHIP AHM-250 Program
The AHM-250 program is designed for a diverse range of healthcare professionals. Employees within healthcare systems, hospitals, and insurance organizations seeking advancement into managerial roles benefit from comprehensive exposure to operational, regulatory, and ethical principles. Case administrators and medical directors expand their administrative competence, enhancing their ability to make informed strategic decisions.
Educators teaching healthcare administration can integrate practical insights into curriculum development, bridging theoretical and real-world knowledge. Insurance agents and brokers specializing in life and health products gain expertise in plan design, operational management, and regulatory compliance, strengthening client advisory capabilities. Financial executives managing health-related resources acquire proficiency in cost-containment strategies, reimbursement models, and benefit optimization. Collectively, these professionals gain competencies essential for leadership in complex healthcare environments.
Study Resources and Exam Preparation
Effective preparation for the AHM-250 exam involves engagement with comprehensive study materials that reflect current industry standards. These resources cover health plan types, operational functions, regulatory frameworks, and ethical principles. Scenario-based exercises and illustrative examples foster experiential learning, enabling candidates to apply theoretical knowledge in practice.
Practice exams replicate the format, timing, and analytical requirements of the actual test. Repeated practice enhances knowledge retention, improves analytical skills, and builds confidence. Continuous updates to study resources ensure alignment with evolving exam content, maintaining relevance and reliability. Structured preparation equips candidates with the competencies required for both examination success and professional application.
Practical Application of Knowledge
Knowledge acquired through the AHM-250 program translates directly into professional practice. Mastery of health plan products, operational processes, regulatory requirements, and ethical considerations enables managers to implement effective strategies that improve efficiency, quality, and member satisfaction. Ethical competence fosters trust among patients, providers, and stakeholders, reinforcing organizational credibility.
Healthcare managers utilize their knowledge to anticipate trends, assess organizational performance, optimize resources, and implement evidence-based interventions. This holistic application of competencies enhances operational outcomes, informs strategic planning, and supports organizational sustainability. The integration of technical, regulatory, and ethical knowledge is critical for effective leadership in contemporary healthcare organizations.
Analytical Skills and Strategic Thinking
Analytical and strategic thinking are vital for healthcare management. The AHM-250 examination emphasizes interpreting data, evaluating operational performance, and formulating evidence-based decisions. Candidates apply analytical skills to financial management, risk assessment, operational optimization, and policy evaluation.
Scenario-based questions develop the ability to synthesize information, consider multiple perspectives, and implement reasoned solutions. This iterative approach strengthens critical thinking, enhances decision-making capacity, and prepares professionals to navigate operational, regulatory, and ethical challenges. By combining analytical rigor with operational expertise, candidates acquire the skills necessary for strategic leadership in complex healthcare environments.
Strategic Utilization of Health Plan Knowledge
The knowledge gained through the AHM-250 program informs strategic planning and organizational development. Understanding health plan products, member benefits, operational domains, and regulatory frameworks allows managers to anticipate trends, evaluate performance, and implement effective solutions.
Strategic application of this knowledge improves operational outcomes, enhances member satisfaction, and aligns organizational objectives with industry best practices. By integrating analytical thinking, operational expertise, and ethical reasoning, healthcare professionals are equipped to address complex challenges and guide their organizations toward sustainable success.
Analytical Proficiency in Healthcare Management
Analytical proficiency underpins informed decision-making in healthcare operations. The AHM-250 program emphasizes data interpretation, performance evaluation, and strategic assessment. Candidates learn to identify trends, assess operational metrics, and implement evidence-based solutions.
Analytical skills enable managers to optimize workflows, allocate resources efficiently, and enhance service quality. Integrating analytical capabilities with operational and ethical considerations strengthens decision-making and prepares professionals to respond proactively to organizational challenges. This analytical foundation is a core competency developed through the AHM-250 program.
Applying Regulatory Knowledge to Practice
Understanding regulatory requirements is essential for healthcare managers. The AHM-250 program highlights how legislation impacts operational processes, plan design, and organizational strategy. Compliance ensures legal adherence, mitigates risk, and supports sustainable operations.
Healthcare managers interpret regulatory changes, evaluate their operational impact, and implement corrective measures. This knowledge ensures integrity, maintains service quality, and fosters organizational accountability. Mastery of regulatory frameworks enables professionals to lead confidently and responsibly in evolving healthcare environments.
Conclusion
The AHIP AHM-250 Healthcare Management program provides a comprehensive framework for developing expertise across health plan products, operational management, regulatory compliance, and ethical decision-making. Through rigorous study of plan types, member benefits, claims processing, provider networks, and utilization review, candidates acquire the analytical skills and strategic insight necessary for effective leadership in complex healthcare environments. Regulatory literacy and ethical acumen ensure professionals can navigate evolving legislation, uphold organizational integrity, and deliver equitable, high-quality care. The integration of practical knowledge with scenario-based exercises fosters critical thinking, problem-solving, and informed decision-making, preparing candidates to address multifaceted challenges in healthcare management. By mastering these competencies, professionals enhance operational efficiency, optimize resources, and promote stakeholder trust, ultimately contributing to organizational sustainability and improved patient outcomes. The AHM-250 program equips healthcare managers to lead with confidence, foresight, and ethical responsibility.