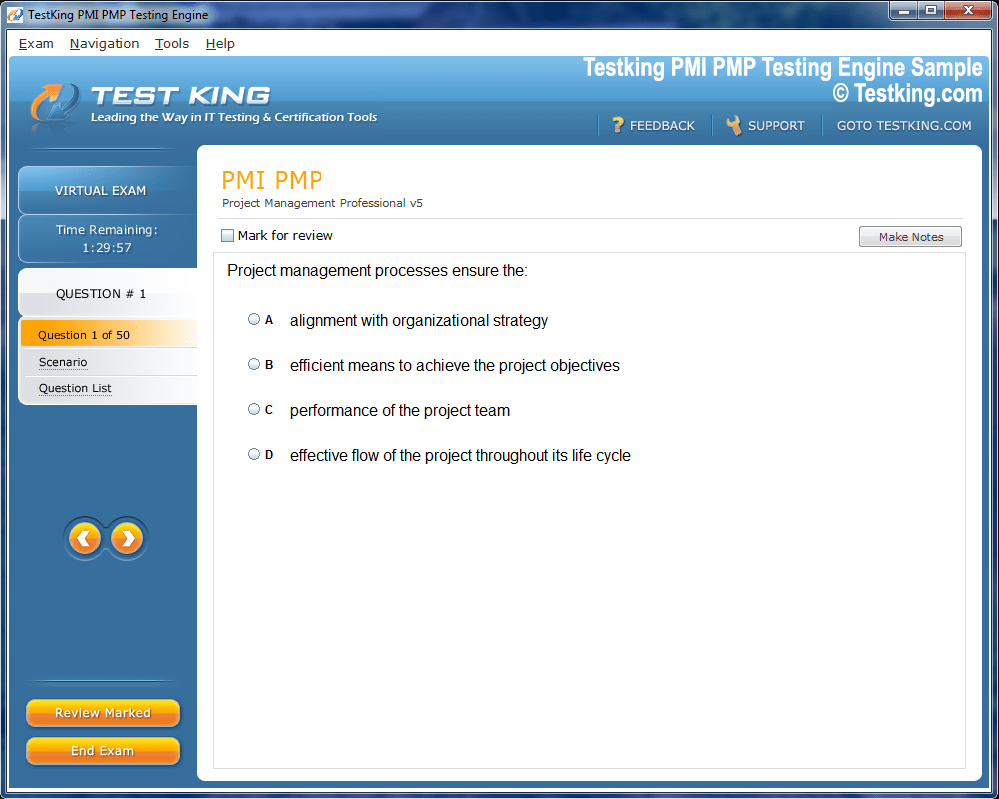
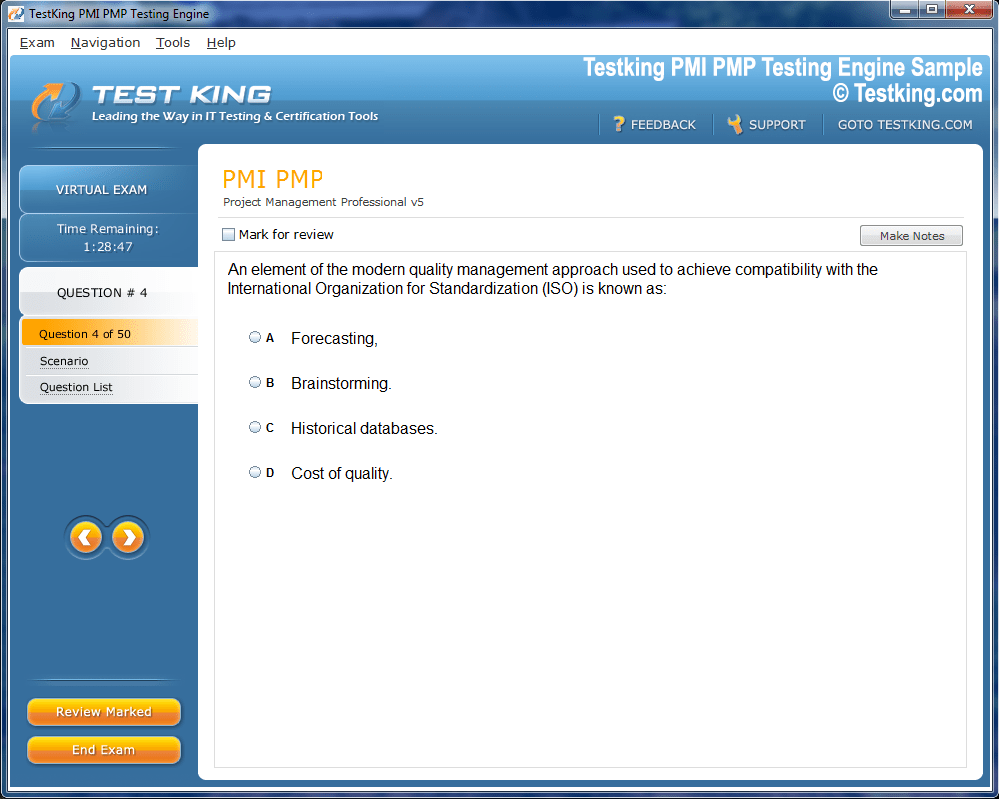
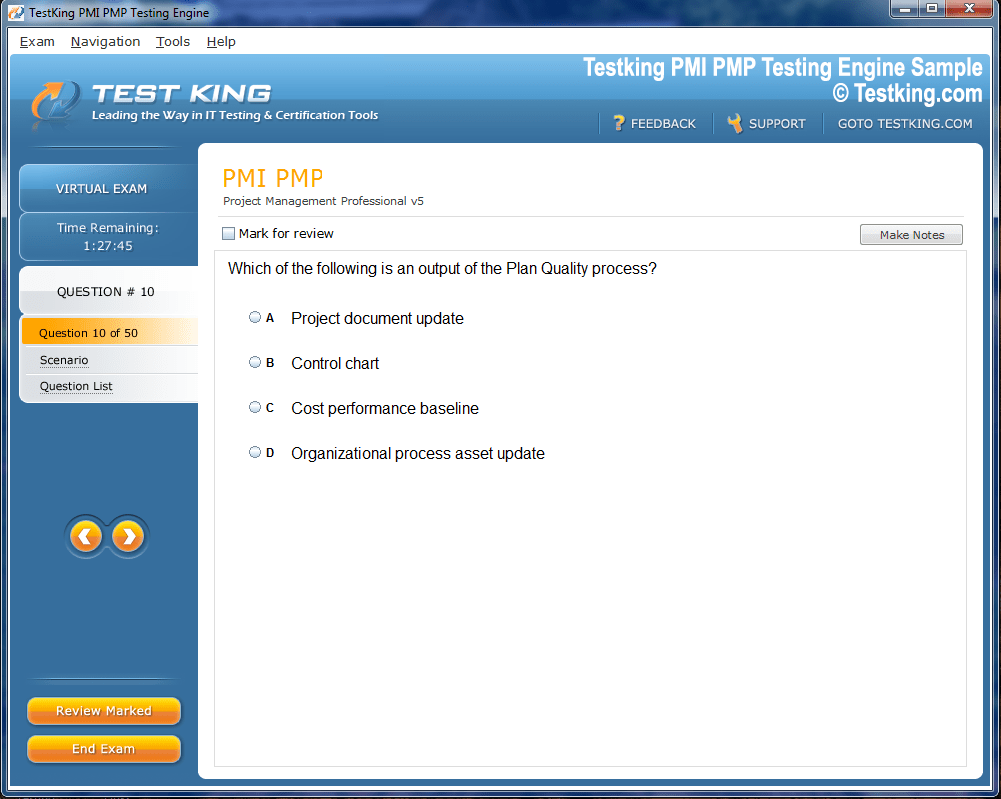
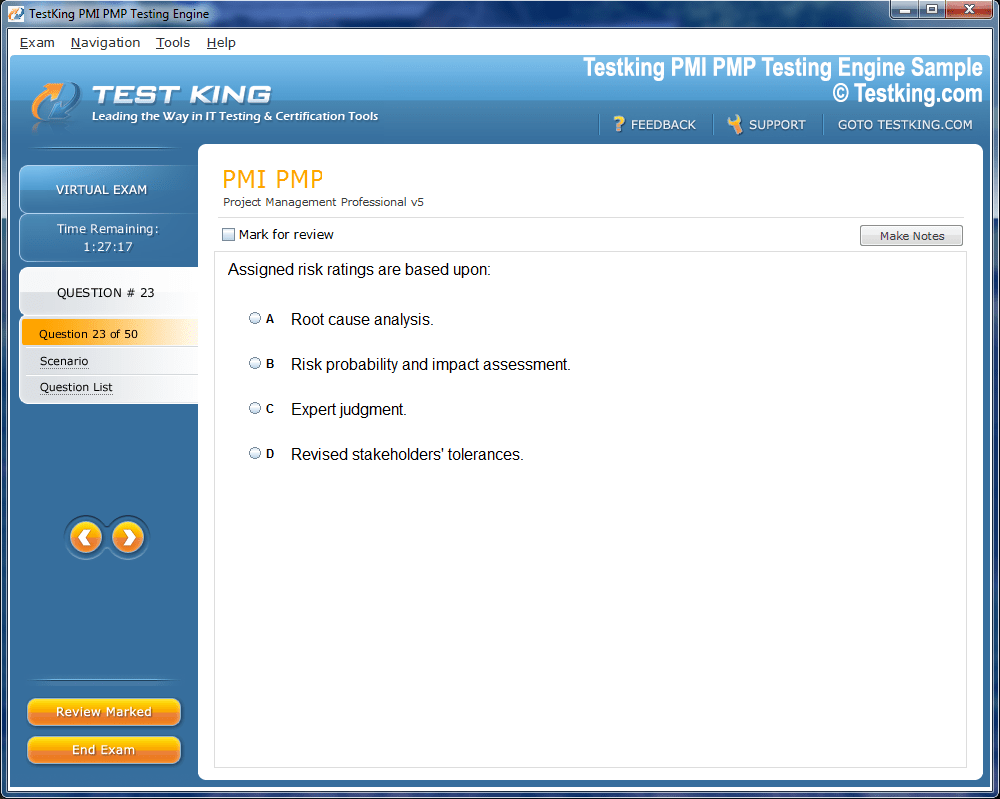
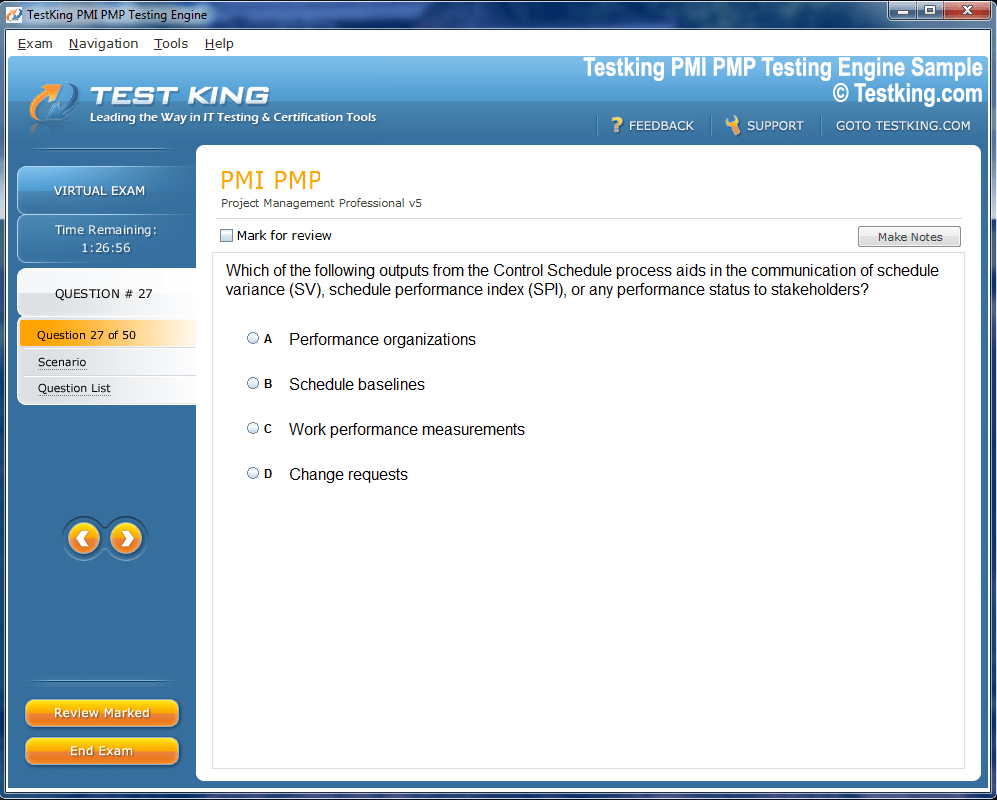
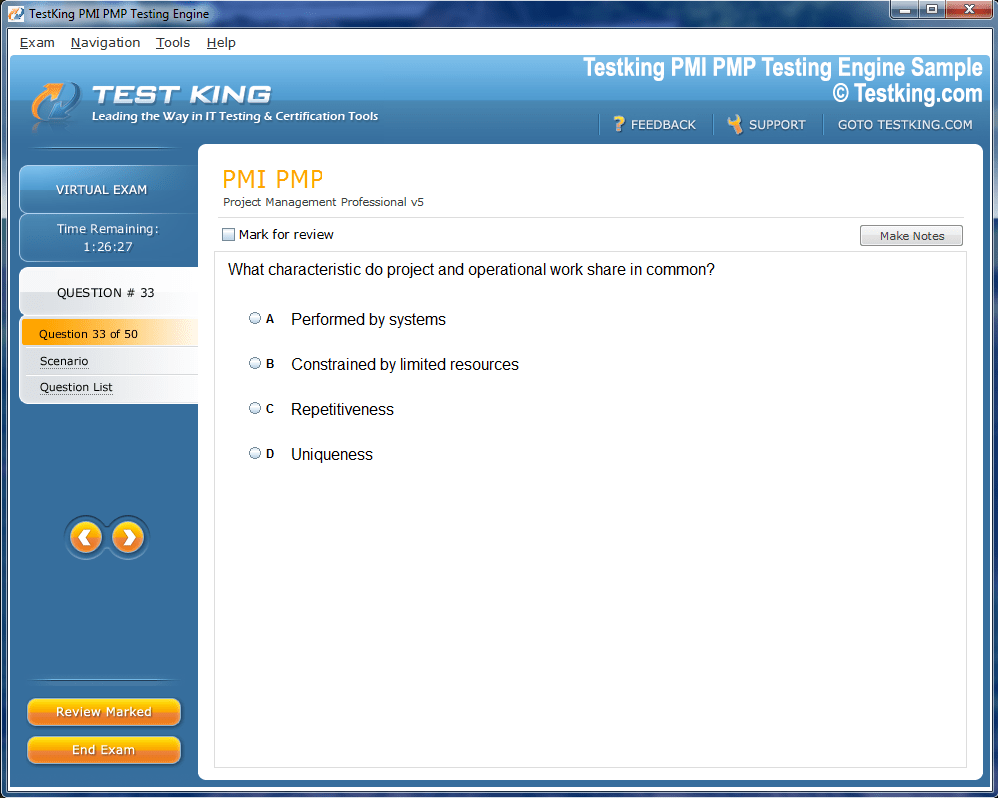
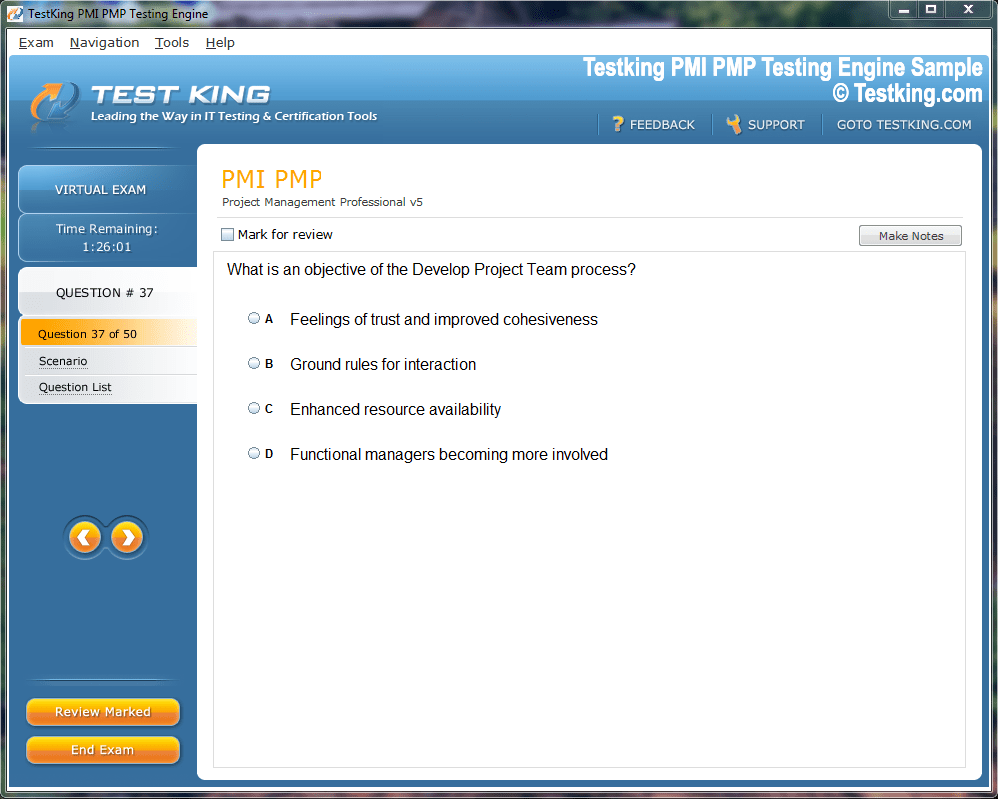
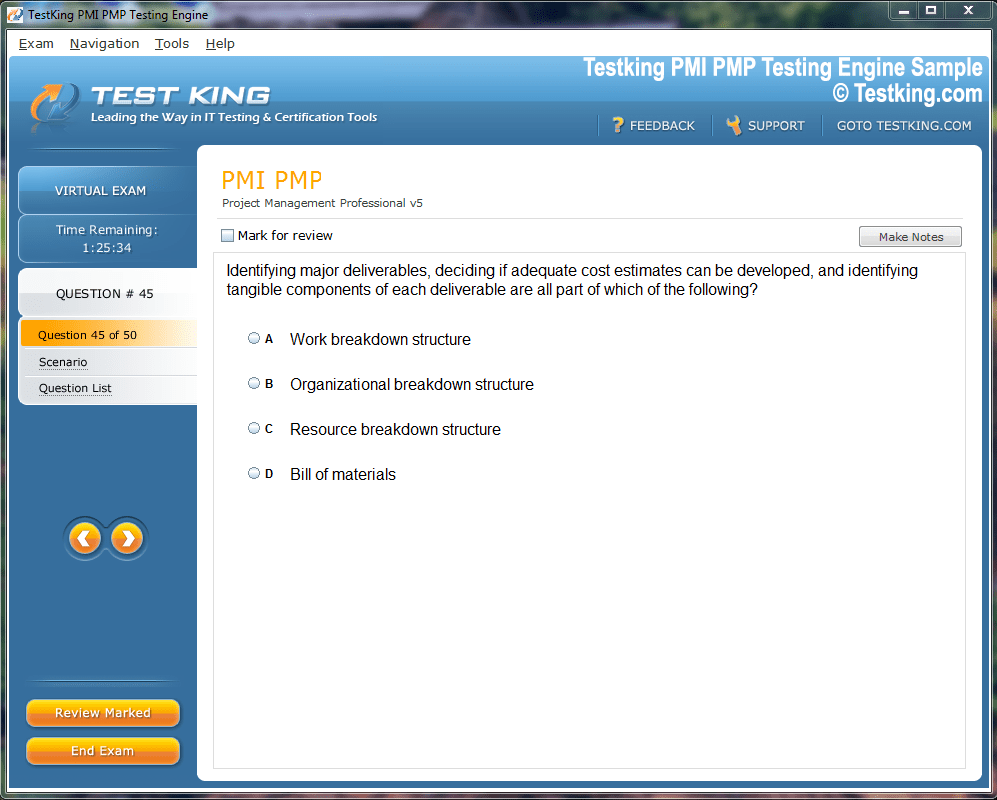
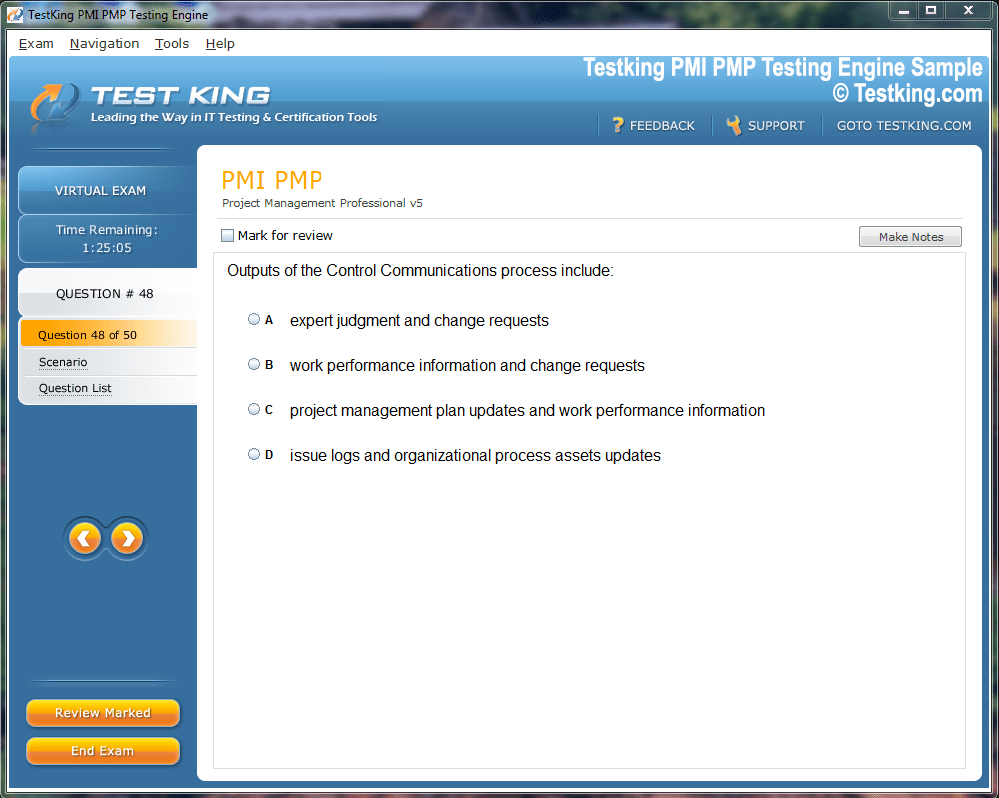
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our CPB testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Top AAPC Exams
A Comprehensive Guide to AAPC CPB Certification Success
In the intricate and often labyrinthine realm of healthcare finance, the role of a Certified Professional Biller (CPB) is indispensable. These professionals operate at the nexus of medical billing, coding, and compliance, ensuring that healthcare providers maintain financial stability while adhering to the rigorous standards of regulatory frameworks. A CPB is not merely an administrator of invoices or claims; they are meticulous stewards of revenue integrity, orchestrating a seamless interplay between clinical documentation, insurance reimbursement, and regulatory compliance. Their function is paramount in facilitating the continuum of care, as precise billing practices directly affect a healthcare organization's capacity to provide high-quality patient services.
Certified Professional Billers possess an extensive repertoire of knowledge in diverse medical coding systems, including Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), and the International Classification of Diseases, 10th Edition, Clinical Modification (ICD-10-CM). This knowledge allows them to interpret complex clinical documentation and translate it into codes that comply with payer requirements. Such expertise is not only technical but also analytical, as CPBs must evaluate claims for accuracy, completeness, and alignment with prevailing reimbursement methodologies. By mitigating errors and optimizing claim submissions, CPBs safeguard revenue streams, reduce the likelihood of denied or delayed claims, and fortify institutional trust with insurers.
Beyond coding, CPBs are deeply involved in navigating the multifaceted landscape of insurance plans, which encompasses private commercial carriers, Medicare, Medicaid, and various managed care organizations. Each insurer operates under distinct policies, reimbursement rules, and claim adjudication procedures. A CPB’s ability to discern these differences ensures that providers receive equitable payment for services rendered. Their work often involves reconciling complex remittance advice, understanding explanation of benefits statements, and advocating for fair reimbursement when discrepancies arise. This requires a blend of analytical acuity and meticulous attention to detail, coupled with the capacity to communicate effectively with insurance representatives and internal stakeholders.
The CPB credential itself represents a mark of excellence, denoting not only technical mastery but also a commitment to ethical standards and professional accountability. Achieving certification signals to employers and peers that the individual possesses the rigor and precision required to operate in an environment where errors can carry significant financial and legal ramifications. Moreover, CPBs must continually update their knowledge in response to evolving healthcare regulations, reimbursement methodologies, and industry standards. Their ongoing education ensures that they remain adept at interpreting new coding guidelines, complying with shifting privacy regulations, and incorporating emerging technologies into billing practices.
In practice, a Certified Professional Biller’s daily responsibilities span a wide spectrum. They manage claims from inception to resolution, including verifying patient information, reviewing clinical documentation, applying accurate codes, and submitting claims electronically or via paper. They analyze denial reports, appeal adverse decisions, and coordinate with clinical and administrative staff to clarify ambiguous documentation. Revenue cycle management is a central component of their role, encompassing everything from pre-authorization verification to post-payment audits. By executing these duties with precision, CPBs help organizations maintain cash flow, reduce financial risk, and ensure operational efficiency.
The importance of CPBs extends beyond operational efficiency into regulatory compliance and fraud prevention. Healthcare institutions are bound by stringent rules, including the Health Insurance Portability and Accountability Act (HIPAA), anti-fraud statutes, and various state and federal guidelines. Inaccurate or fraudulent billing can lead to severe penalties, legal action, and reputational damage. CPBs serve as guardians against such pitfalls, identifying potential red flags, ensuring documentation supports every claim, and maintaining rigorous standards of transparency and accountability. Their role is both proactive and preventive, minimizing exposure to audits, investigations, and financial losses.
Another significant facet of the CPB profession is its intersection with technology. Modern healthcare billing relies heavily on electronic health records (EHR) systems, automated claim submission platforms, and sophisticated billing software. CPBs must not only understand these technological tools but also leverage them to optimize workflows, track claim status, and generate actionable financial reports. Familiarity with data analytics and reporting tools allows CPBs to identify patterns, detect anomalies, and propose improvements in revenue cycle management processes. This technological fluency, combined with industry knowledge, positions CPBs as essential contributors to organizational strategy and financial decision-making.
The analytical and administrative capabilities of CPBs are complemented by soft skills that are critical for success. Effective communication, negotiation, and problem-solving are integral to resolving claim disputes, coordinating with multiple departments, and interpreting complex payer requirements. Empathy and professionalism also play roles, particularly when interacting with patients regarding billing questions, insurance coverage, or payment plans. The ability to navigate sensitive financial conversations while maintaining clarity and accuracy underscores the multifaceted nature of the CPB’s responsibilities.
Achieving CPB certification typically involves meeting certain eligibility requirements, which include practical experience in medical billing or a related field. Candidates must demonstrate proficiency in coding systems, claims processing, reimbursement methodologies, and compliance regulations. While formal educational prerequisites may vary, many candidates benefit from completing relevant coursework or training programs in medical billing and coding. Once these criteria are met, candidates sit for the CPB exam, a comprehensive assessment designed to evaluate their knowledge, analytical skills, and problem-solving capabilities across real-world billing scenarios.
Preparation for the CPB exam requires disciplined study and strategic planning. Candidates often utilize a combination of official study guides, practice exams, and scenario-based exercises to develop fluency in coding principles and billing procedures. A robust understanding of medical terminology, anatomy, and documentation standards is essential, as these areas form the foundation for accurate coding and claim submission. In addition, familiarity with healthcare regulations, insurance plans, and reimbursement methodologies enhances a candidate’s ability to navigate complex billing situations and anticipate potential challenges.
Once certified, CPBs are expected to maintain their credentials through continuing education. This ensures they remain current with emerging regulations, updated coding standards, and evolving reimbursement models. Certification renewal typically involves completing a designated number of continuing education units over a specified period, demonstrating both a commitment to professional development and an adherence to the highest standards of practice. By continuously expanding their knowledge base, CPBs reinforce their value to healthcare organizations and ensure that they remain adept at managing the ever-changing landscape of medical billing.
The role of a Certified Professional Biller is multifaceted and highly specialized, encompassing technical, analytical, and interpersonal skills. They operate as linchpins in the financial operations of healthcare organizations, translating complex clinical information into accurate claims, navigating insurance systems, and ensuring compliance with regulatory standards. Their work safeguards revenue, enhances operational efficiency, and supports the overarching mission of healthcare institutions: delivering quality care to patients while maintaining fiscal integrity. The CPB designation embodies a commitment to excellence, meticulousness, and professional stewardship, reflecting the vital contributions these individuals make to the stability and sustainability of the healthcare industry.
The Structure and Scope of the Certified Professional Biller Exam
The Certified Professional Biller (CPB) exam serves as a comprehensive assessment of knowledge, skills, and analytical acuity in the domain of medical billing. Designed to validate proficiency across a wide spectrum of healthcare finance functions, the exam evaluates a candidate’s capacity to navigate complex regulatory environments, apply coding principles accurately, and manage the revenue cycle with precision. Its scope extends beyond rote memorization of coding rules, encompassing practical judgment, ethical considerations, and the ability to reconcile discrepancies between clinical documentation and insurer requirements.
The CPB exam’s architecture reflects the multifaceted responsibilities of a professional biller. Candidates encounter questions that span medical terminology, anatomy, and coding systems, including CPT, HCPCS, and ICD-10-CM. These coding frameworks form the backbone of the billing process, translating clinical procedures into universally recognized numeric or alphanumeric identifiers. Proficiency in these systems enables the accurate submission of claims, mitigates the risk of denial, and ensures adherence to payer-specific guidelines. Candidates must also demonstrate an understanding of insurance plan structures, encompassing private commercial policies, Medicare, Medicaid, and managed care organizations. The examination tests their ability to distinguish between plan types, coordinate benefits, and apply payer-specific rules for reimbursement.
Claims processing and revenue cycle management constitute another essential component of the CPB exam. Candidates must be adept at reviewing clinical documentation, verifying patient information, and applying correct codes to generate claims. They also encounter scenarios involving claim denials, adjustments, and appeals, requiring a combination of analytical reasoning and procedural knowledge. This aspect of the exam emphasizes the practical application of billing principles, reflecting the real-world challenges faced by professionals in healthcare finance. Furthermore, candidates are assessed on their familiarity with electronic claim submission platforms, validation protocols, and remittance advice interpretation. Competence in these areas ensures that claim processing is efficient, accurate, and compliant with industry standards.
The examination also delves into reimbursement methodologies, requiring candidates to comprehend fee-for-service structures, Resource-Based Relative Value Scale (RBRVS) calculations, Prospective Payment Systems (PPS), and the nuances of Medicare, Medicaid, and commercial insurance reimbursement policies. A thorough grasp of these methodologies allows CPBs to anticipate potential payment discrepancies, optimize revenue streams, and advocate effectively for providers. Additionally, candidates are tested on regulatory compliance, including HIPAA requirements, anti-fraud provisions, and privacy safeguards. Understanding these regulations is vital, as failure to comply can result in legal penalties, financial loss, or reputational harm to healthcare organizations.
Preparation for the CPB exam necessitates a strategic and structured approach. Candidates benefit from reviewing the official exam content outline provided by the certifying body, which delineates the domains and competencies assessed. By using this outline as a blueprint, individuals can prioritize areas of study, allocate time effectively, and ensure comprehensive coverage of essential topics. Official study materials, including manuals, workbooks, and practice exams, provide detailed guidance and scenario-based exercises that mirror the format of the examination. These resources not only reinforce foundational knowledge but also cultivate problem-solving skills and analytical reasoning.
A critical aspect of exam preparation is mastery of medical billing concepts. Candidates must internalize the principles of claims adjudication, charge capture, collections, denials management, and appeals processes. Scenario-based practice, such as simulating claims submissions or analyzing remittance advice statements, allows candidates to apply theoretical knowledge in realistic contexts. Such exercises enhance critical thinking, decision-making, and the ability to identify errors or inconsistencies in documentation and claims. Familiarity with billing software, electronic health records, and coding tools further supports accurate and efficient claim management.
Medical terminology and anatomy are foundational to the CPB exam. Candidates must comprehend clinical language, abbreviations, and the basic structure and function of the human body to assign codes accurately. An understanding of medical procedures, diagnostic classifications, and treatment protocols enhances the accuracy of coding and billing, ensuring that claims reflect the services provided. This knowledge also supports effective communication with healthcare providers, auditors, and insurers, fostering a collaborative approach to financial and clinical operations.
Time management and test-taking strategies are pivotal to success on the CPB exam. With approximately 200 multiple-choice questions to be completed within a five-hour window, candidates must balance accuracy with efficiency. Practicing under timed conditions allows candidates to simulate the exam environment, develop pacing strategies, and identify areas that require additional review. Utilizing practice exams and sample questions helps reinforce understanding, build confidence, and reduce anxiety on the day of testing.
The CPB exam also emphasizes ethical decision-making and fraud prevention. Candidates are expected to recognize and address potential instances of billing impropriety, such as submitting claims for services not rendered or manipulating codes to maximize reimbursement. Knowledge of anti-fraud laws, compliance programs, and reporting protocols is essential, as these safeguards protect both the patient and the organization from financial and legal consequences. Ethical awareness ensures that CPBs uphold the integrity of the healthcare billing process and contribute to a culture of accountability.
Passing the CPB exam requires a combination of technical expertise, analytical skills, and professional judgment. A minimum score of 70% is typically required for certification, reflecting a candidate’s ability to navigate the complexities of medical billing accurately and efficiently. Achieving certification signals mastery of critical concepts, operational competence, and a commitment to ethical and professional standards. Certified Professional Billers are therefore recognized not only for their technical capabilities but also for their role in sustaining organizational integrity, optimizing revenue cycles, and supporting high-quality patient care.
Once certified, CPBs enter a dynamic professional environment that demands continuous learning and adaptability. Healthcare regulations, coding standards, and reimbursement methodologies evolve regularly, and staying current is essential for maintaining certification and ensuring effective practice. Continuing education, professional development programs, and industry workshops provide opportunities to expand knowledge, refine skills, and remain abreast of changes that impact billing operations. This ongoing commitment to learning reinforces the value of CPBs within healthcare organizations and supports long-term career growth.
The CPB exam, therefore, represents both a culmination of rigorous study and a gateway to a specialized and highly respected profession. Its structure, content, and evaluation methods are carefully designed to reflect the realities of healthcare finance, ensuring that certified individuals possess the knowledge, skill, and judgment necessary to excel in complex billing environments. Mastery of the exam not only facilitates professional recognition but also enhances organizational efficiency, regulatory compliance, and financial stability.
Ultimately, the Certified Professional Biller exam is a multifaceted instrument for assessing competence, fostering professionalism, and reinforcing ethical standards in healthcare finance. Its comprehensive scope ensures that certified individuals are well-equipped to manage the nuanced interactions between clinical documentation, payer systems, and regulatory requirements. By preparing strategically, studying diligently, and embracing continuous learning, candidates can achieve certification and contribute meaningfully to the operational and financial success of healthcare institutions.
Eligibility, Registration, and Preparation Strategies for the Certified Professional Biller Exam
The path to becoming a Certified Professional Biller involves a structured combination of eligibility verification, exam registration, and strategic preparation. These stages are designed to ensure that candidates possess the requisite knowledge, experience, and competencies to navigate the complexities of healthcare finance effectively. Understanding the eligibility criteria is the initial step, as it ensures that candidates are adequately prepared to engage with the technical and analytical demands of the CPB exam.
Eligibility for the CPB exam is primarily based on professional experience in medical billing or a closely related field. Although formal educational prerequisites may not be strictly mandated, a high school diploma or equivalent is generally recommended to establish foundational literacy and numeracy skills. Candidates must typically demonstrate at least two years of experience performing billing-related tasks, which may include claim preparation, reimbursement management, coding, or billing documentation. This practical exposure cultivates familiarity with common billing scenarios, insurance workflows, and revenue cycle processes, providing a real-world context for the concepts assessed on the exam. Experience can be acquired through employment, externships, apprenticeships, or structured training programs that involve direct engagement with billing systems and documentation practices.
Membership in the certifying body, the American Academy of Professional Coders, is optional but highly advantageous. Members gain access to resources that facilitate exam preparation, including study guides, practice exams, webinars, and networking opportunities. While membership does not directly affect eligibility, the insights and tools provided can enhance a candidate’s readiness and confidence in approaching the exam. Candidates are encouraged to review the official guidelines to confirm that they meet all eligibility requirements before initiating the registration process.
Registration for the CPB exam involves a series of organized steps that ensure candidates are formally enrolled and prepared for testing. The first step is establishing an account with the certifying organization, which serves as a gateway to the exam portal. Candidates then select the CPB exam within the certification section, verify that eligibility criteria are satisfied, and choose a suitable date and testing format. Options typically include in-person exam centers or online proctored assessments, offering flexibility to accommodate diverse schedules and geographic locations. Payment of the examination fee is required to complete registration, and candidates are advised to consult official sources for current fee structures and payment procedures.
Preparation for the CPB exam requires a methodical and comprehensive approach, combining theoretical study, practical exercises, and scenario-based practice. A review of the official exam content outline provides a roadmap for identifying critical areas of focus, including coding systems, medical terminology, anatomy, claims processing, reimbursement methodologies, and compliance standards. Organizing study sessions around these domains ensures balanced coverage and reduces the likelihood of gaps in knowledge. Candidates benefit from using official manuals, workbooks, and practice exams, which simulate the exam environment and reinforce comprehension of complex concepts.
Mastery of coding systems is central to successful exam performance. Candidates must be fluent in CPT, HCPCS, and ICD-10-CM codes, understanding not only the technical specifications but also their practical applications in claims adjudication and revenue cycle management. Proficiency in these systems enables accurate translation of clinical documentation into coded claims, minimizing errors, and facilitating efficient reimbursement. In addition, candidates must comprehend insurance plan structures, reimbursement methodologies, and payer-specific requirements to navigate the financial and procedural intricacies of healthcare billing effectively.
Scenario-based practice is a particularly effective preparation strategy, allowing candidates to apply knowledge in realistic contexts. Simulating claim submission, denial analysis, or remittance review exercises cultivates analytical thinking and problem-solving skills. Candidates can practice identifying discrepancies, reconciling errors, and determining appropriate courses of action in alignment with regulatory standards. This experiential approach reinforces theoretical knowledge and enhances the ability to make informed decisions under the constraints of real-world billing environments.
Developing a disciplined study schedule is essential to managing the breadth of exam content. Candidates should allocate sufficient time to each domain, incorporating review sessions, practice questions, and targeted exercises for areas of relative weakness. Balancing intensity with consistency promotes retention and reduces the risk of cognitive overload. Establishing milestones and self-assessment checkpoints enables candidates to monitor progress, adjust study strategies, and maintain focus throughout the preparation period.
Engagement with peer study groups or professional forums provides additional benefits. Interacting with fellow candidates or experienced practitioners fosters discussion, encourages exchange of strategies, and clarifies complex concepts. Collaborative learning also exposes candidates to diverse perspectives and practical insights, enhancing understanding of nuanced billing scenarios and regulatory interpretations. Online communities and discussion boards often serve as valuable platforms for resource sharing, problem-solving, and ongoing support.
Understanding regulatory compliance is another critical component of exam readiness. Candidates must be well-versed in HIPAA regulations, anti-fraud statutes, privacy safeguards, and ethical billing practices. Knowledge of compliance requirements ensures that claim submission, documentation, and reimbursement processes adhere to legal standards, mitigating the risk of penalties or audits. Ethical awareness is particularly important in navigating situations involving discrepancies, potential fraud, or patient billing concerns, reinforcing the professional responsibility inherent in the CPB role.
Effective utilization of practice exams strengthens both technical and strategic skills. These exams allow candidates to familiarize themselves with question formats, timing constraints, and exam logic. Performance analysis of practice tests helps identify recurring errors, knowledge gaps, and areas requiring additional review. By simulating the conditions of the actual examination, candidates can enhance confidence, reduce test anxiety, and refine time management strategies essential for completing the exam efficiently.
Medical terminology and anatomy form the foundational knowledge underpinning accurate coding and claims management. A thorough understanding of clinical language, abbreviations, and anatomical structures enables precise interpretation of physician notes, diagnostic reports, and procedural documentation. This comprehension ensures that claims are accurate, complete, and defensible, reflecting the services provided and aligning with insurer requirements. Integrating terminology and anatomy review into study routines reinforces technical proficiency and supports problem-solving during scenario-based exercises.
Technology proficiency is increasingly critical in the CPB preparation process. Modern billing environments rely on electronic health records, automated coding systems, and integrated claims management platforms. Familiarity with these technologies allows candidates to simulate realistic billing scenarios, practice electronic submissions, and develop strategies for monitoring claim status. Understanding system functionalities, validation protocols, and reporting tools enhances a candidate’s operational competence and reinforces readiness for both the exam and professional practice.
Time management and cognitive endurance are essential skills for navigating the CPB exam successfully. Candidates must balance accuracy with efficiency, addressing approximately 200 multiple-choice questions within a five-hour timeframe. Practicing under timed conditions cultivates pacing strategies, reduces decision fatigue, and enables candidates to allocate attention effectively across domains. Regular practice sessions incorporating simulation of exam conditions enhance familiarity, build endurance, and foster confidence.
Finally, adopting a holistic preparation approach that integrates knowledge acquisition, scenario practice, regulatory understanding, technology fluency, and time management strategies provides a strong foundation for exam success. Candidates who engage in structured, disciplined, and reflective study routines increase their likelihood of achieving certification. The CPB credential is both a culmination of rigorous preparation and a gateway to a profession that demands precision, analytical capability, and ethical responsibility, ensuring that healthcare organizations operate efficiently and maintain financial integrity.
Exam Content, Subjects, and Procedures in the Certified Professional Biller Certification
The Certified Professional Biller (CPB) certification encompasses a broad and multifaceted examination designed to assess a candidate’s mastery of medical billing, coding, compliance, and revenue cycle management. The exam’s content reflects the intricate responsibilities of CPBs, evaluating technical competence, analytical reasoning, and ethical decision-making within the context of healthcare finance. Mastery of these subjects ensures that certified individuals can manage claims accurately, optimize reimbursement, and maintain regulatory compliance, thereby safeguarding the financial and operational health of healthcare organizations.
A central component of the exam is healthcare regulations and compliance. Candidates are required to demonstrate a comprehensive understanding of HIPAA regulations, privacy and security rules, and the principles of fraud and abuse prevention. This knowledge ensures that claims processing, documentation, and interactions with insurers adhere to legal and ethical standards. CPBs must be able to identify potential noncompliance, mitigate risks, and contribute to institutional compliance programs, reinforcing the integrity of organizational operations. Ethical considerations are integral, encompassing the detection and reporting of fraudulent activities, accurate representation of clinical services, and adherence to privacy safeguards that protect patient information.
Medical billing concepts and processes form another core area of focus. Candidates are assessed on revenue cycle management, including pre-authorization procedures, claims processing, charge capture, billing and collections, denials management, refunds, and appeals. Each of these processes involves careful attention to detail and the application of standardized protocols. By mastering these areas, CPBs ensure the efficiency of billing workflows, minimize revenue leakage, and maintain the accuracy and timeliness of payments. They must also demonstrate the ability to reconcile discrepancies between documentation and payer requirements, applying critical thinking to resolve complex billing scenarios.
Coding systems are a significant focus of the CPB exam. Candidates must demonstrate proficiency in Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), and the International Classification of Diseases, 10th Edition, Clinical Modification (ICD-10-CM). Accurate application of these coding systems is essential for claim submission, reimbursement, and compliance. Candidates must understand coding conventions, guidelines, and modifiers to ensure that claims reflect the services rendered accurately. Proficiency in these systems allows CPBs to detect errors, correct documentation gaps, and ensure that reimbursement aligns with provider services, enhancing both financial stability and operational efficiency.
Reimbursement methodologies also feature prominently in the CPB exam. Candidates are evaluated on their understanding of fee-for-service models, Resource-Based Relative Value Scale (RBRVS), Prospective Payment Systems (PPS), and the reimbursement frameworks utilized by Medicare, Medicaid, and commercial insurers. Understanding these methodologies enables CPBs to anticipate payment variances, optimize claims for maximum reimbursement, and navigate complex payer requirements. This knowledge is critical in maintaining revenue integrity, avoiding underpayment, and ensuring that healthcare providers are fairly compensated for their services.
Documentation requirements are equally essential in the examination. Candidates must be able to interpret medical records, clinical notes, and procedural documentation to assign accurate codes and submit compliant claims. The CPB exam evaluates the ability to apply documentation standards to diverse services and procedures, ensuring consistency, accuracy, and alignment with regulatory mandates. This proficiency also supports the resolution of claim denials, the preparation of appeals, and the accurate communication of patient information in accordance with privacy regulations.
Insurance plans and payer knowledge constitute a critical segment of the exam. Candidates must understand the operations of Medicare, Medicaid, commercial insurance plans, and managed care organizations, including coordination of benefits and coverage verification. This knowledge allows CPBs to navigate payer-specific rules, resolve disputes efficiently, and ensure that claims are submitted in accordance with contractual requirements. Familiarity with payer structures also enables CPBs to provide accurate financial guidance to patients and providers, fostering transparency and efficiency in the revenue cycle.
Claim submission and processing are extensively tested in the CPB exam. Candidates must demonstrate proficiency in both electronic and paper claim submission, including claim edits, validation, and adjudication procedures. Understanding claim status, remittance advice, and reconciliation processes is essential for maintaining revenue flow and minimizing errors. CPBs must also be able to respond to claim denials, perform appeals, and apply adjustments when necessary, highlighting the practical application of technical knowledge in real-world scenarios.
Medical terminology and anatomy are foundational elements of the exam content. Candidates are expected to comprehend medical terms, abbreviations, and basic human anatomy to accurately assign codes and interpret clinical documentation. This knowledge supports precise communication with healthcare providers, facilitates accurate coding, and ensures that claims reflect the services delivered. It also enables CPBs to understand complex medical procedures, diagnoses, and treatments, providing the context necessary for effective revenue cycle management.
The CPB exam is designed to be both rigorous and comprehensive, integrating multiple domains of knowledge into a unified assessment. Its structure reflects the interconnected nature of healthcare finance, emphasizing the importance of technical skills, analytical reasoning, and ethical responsibility. Candidates must demonstrate the ability to synthesize information from clinical documentation, insurance guidelines, and regulatory requirements to generate accurate and compliant claims. The examination challenges individuals to apply their knowledge in a variety of scenarios, requiring careful judgment, attention to detail, and the ability to resolve complex problems efficiently.
Preparation strategies for the CPB exam involve a blend of formal study, practical exercises, and ongoing skill reinforcement. Utilizing official study materials, including workbooks, manuals, and practice exams, provides candidates with structured guidance and exposure to representative questions. Scenario-based practice allows for the application of coding, billing, and documentation knowledge in realistic contexts, reinforcing analytical and problem-solving abilities. Study schedules that balance content review, practice exercises, and timed simulations enhance retention and build confidence for exam day.
Continuing education and professional development also support success on the CPB exam. Webinars, workshops, and industry events provide opportunities to stay current with evolving coding standards, reimbursement methodologies, and regulatory changes. Engaging with peers in study groups or professional forums facilitates knowledge exchange, clarification of complex concepts, and exposure to diverse perspectives. Candidates who adopt a disciplined, multifaceted approach to preparation are better equipped to navigate the demands of the exam and demonstrate mastery of essential competencies.
The CPB exam ultimately serves as a benchmark of professional capability, ensuring that certified individuals possess the expertise necessary to perform at a high level in the field of medical billing. Its content, subjects, and procedures reflect the real-world responsibilities of CPBs, emphasizing accuracy, efficiency, compliance, and ethical decision-making. Success on the exam validates a candidate’s ability to contribute meaningfully to healthcare organizations, optimize revenue cycles, and uphold the integrity of billing and reimbursement processes.
By integrating technical knowledge, practical skills, and ethical awareness, CPB-certified professionals are uniquely positioned to manage the intricacies of healthcare finance. Their expertise ensures that claims are processed correctly, reimbursements are optimized, and regulatory requirements are consistently met. The examination’s comprehensive coverage provides both a rigorous challenge and a valuable credential, recognizing individuals who demonstrate proficiency, professionalism, and a commitment to excellence in the critical domain of medical billing.
Sustaining Certification and Advancing in the Career of a Certified Professional Biller
Achieving the Certified Professional Biller (CPB) credential is a milestone that signifies both professional mastery and a commitment to excellence in healthcare finance. However, earning certification represents only the beginning of a continuous journey of professional growth, skill refinement, and adherence to evolving standards. Certified Professional Billers are not merely technical specialists in medical billing, coding, and revenue cycle management; they are strategic contributors to organizational stability, ethical compliance, and operational efficiency. Maintaining certification requires dedication to ongoing education, systematic documentation, and proactive adaptation to the ever-changing landscape of healthcare administration. The sustained relevance and effectiveness of a CPB depend on integrating these elements into a holistic career development approach that balances technical proficiency, regulatory knowledge, and ethical responsibility.
The foundation of maintaining CPB certification is adherence to the renewal guidelines set by the certifying organization. CPBs must engage in continuous educational activities that strengthen their technical capabilities, enhance regulatory awareness, and reinforce ethical practice. These activities encompass a wide array of opportunities, including webinars, workshops, industry conferences, online courses, and other professional development programs designed to address updates in coding standards, reimbursement methodologies, compliance regulations, and emerging technologies. Accumulating a predetermined number of continuing education units (CEUs) within a defined timeframe is typically required to retain certification. This structured approach ensures that CPBs remain current with evolving industry requirements and possess the skills necessary to process claims accurately, manage revenue cycles efficiently, and maintain compliance with regulatory mandates.
An essential component of certification maintenance is meticulous documentation of all continuing education activities. CPBs are required to provide verifiable records of completed CEUs, such as certificates of attendance, course completion statements, or workshop acknowledgments. Most certifying bodies facilitate submission through online portals, streamlining tracking, verification, and recordkeeping. Maintaining accurate documentation demonstrates accountability, upholds professional integrity, and ensures compliance with certification standards. It also serves as evidence that the professional is actively engaged in enhancing knowledge and skills, which is crucial for both professional credibility and organizational trust. Alongside educational achievements, CPBs must remit any applicable renewal fees to maintain active certification status, reinforcing the commitment to ongoing professional stewardship.
Remaining informed about industry developments is critical for both maintaining certification and advancing a career in medical billing. The healthcare billing environment is characterized by rapid evolution, with frequent updates to coding conventions, payer policies, reimbursement models, and regulatory frameworks. CPBs must actively monitor these changes and integrate new knowledge into their practice to ensure accuracy, efficiency, and compliance. Engaging with professional associations, attending industry conferences, participating in specialized workshops, and networking with peers are effective strategies for staying abreast of trends, innovations, and best practices. This continuous engagement not only reinforces technical competence but also cultivates strategic insight, enabling CPBs to anticipate challenges and implement solutions proactively.
Technology has become a central component of professional growth for CPBs. Modern healthcare billing increasingly relies on electronic health record (EHR) systems, automated claims management platforms, and data analytics tools that facilitate accurate coding, efficient claim submission, and comprehensive revenue tracking. Proficiency in these technologies enhances operational effectiveness, supports data-driven decision-making, and enables CPBs to detect patterns, anomalies, or discrepancies in billing operations. By embracing technological tools, CPBs can adapt to evolving workflows, optimize processes, and contribute to strategic planning beyond traditional billing responsibilities. This technological fluency strengthens a professional’s ability to influence organizational performance and maintain a competitive edge in the field.
A deeper understanding of reimbursement methodologies and insurance frameworks further distinguishes experienced CPBs. Mastery of fee-for-service models, Resource-Based Relative Value Scale (RBRVS), Prospective Payment Systems (PPS), and payer-specific guidelines equips professionals to optimize revenue streams and navigate complex interactions with insurers. This expertise enables CPBs to identify underpayments, reconcile billing discrepancies, and advocate effectively for fair reimbursement. Knowledge of payer-specific rules also supports accurate patient billing, minimizes administrative delays, and protects both providers and patients from financial inconsistencies. Proficiency in these areas enhances the strategic value of CPBs within healthcare organizations and reinforces the sustainability of institutional financial operations.
Ethical responsibility remains a fundamental pillar of the CPB profession. Professionals are charged with ensuring accuracy, preventing fraud, detecting inconsistencies, and maintaining compliance with HIPAA and other regulatory mandates. Ethical vigilance extends to interactions with patients, healthcare providers, and insurers, fostering transparency, accountability, and trust. CPBs serve as stewards of integrity in healthcare finance, safeguarding the organization’s reputation and contributing to a culture of compliance and professionalism. Participation in continuing education and adherence to professional standards reinforce this ethical foundation, ensuring that CPBs remain reliable and credible contributors to the broader healthcare system.
Career advancement opportunities for CPBs are diverse, reflecting the multifaceted nature of the profession. Certified professionals can progress into roles such as revenue cycle managers, billing supervisors, compliance specialists, or healthcare administrators. These positions often require oversight of complex financial operations, policy development, and team leadership. Furthermore, specialization in areas such as payer-specific reimbursement, auditing protocols, or advanced coding practices opens avenues for consultancy, professional training, or education. CPBs who pursue these pathways leverage their expertise to mentor colleagues, optimize organizational performance, and influence broader operational strategies, demonstrating the expanded scope of influence that certification enables.
Professional networking and engagement with industry peers play a crucial role in both career development and knowledge enhancement. Participation in professional forums, online communities, association events, and industry conferences provides opportunities to share experiences, exchange insights, and remain informed about emerging trends. Networking also exposes CPBs to diverse perspectives, problem-solving approaches, and innovative practices, enriching both individual careers and organizational operations. Mentorship opportunities and collaborative projects further strengthen professional development, fostering both personal growth and the advancement of collective industry knowledge.
Strategic planning and disciplined career management are key to long-term success in the CPB profession. Certified professionals are encouraged to establish structured learning plans, track continuing education progress, and evaluate performance in practical billing scenarios. Regular self-assessment, reflection on industry changes, and proactive engagement with new methodologies and technologies reinforce expertise and adaptability. This approach ensures that CPBs remain at the forefront of healthcare finance, capable of addressing complex challenges with precision, foresight, and confidence. By integrating continuous learning, ethical practice, and technological proficiency into a cohesive career strategy, CPBs strengthen their professional value and sustain relevance in a dynamic industry.
The CPB credential thus functions as both a recognition of technical competence and a foundation for ongoing professional growth. Maintaining certification integrates educational engagement, meticulous documentation, ethical awareness, technological aptitude, and strategic planning, forming a comprehensive framework for career advancement. CPBs who commit to lifelong learning, peer engagement, and industry awareness not only preserve the validity of their certification but also enhance their ability to influence organizational efficiency, financial integrity, and compliance adherence. Their continued contributions ensure that healthcare organizations operate effectively, optimize revenue cycles, and deliver high-quality patient care.
Sustaining CPB certification is a dynamic, multifaceted process that extends well beyond initial achievement. Certified Professional Billers are entrusted with critical responsibilities that encompass accurate claims processing, regulatory compliance, revenue optimization, and ethical stewardship. By embracing ongoing education, documenting progress meticulously, leveraging technology, and engaging in professional networks, CPBs maintain the relevance, efficacy, and integrity of their role. These practices empower professionals to advance in their careers, transition into leadership positions, and shape the future of healthcare finance. Through this continuous commitment to excellence, CPBs reinforce their value, contribute meaningfully to organizational success, and uphold the mission of providing accurate, ethical, and efficient financial services in healthcare.
Conclusion
The Certified Professional Biller (CPB) credential represents more than a certification—it embodies expertise, professionalism, and a sustained commitment to excellence in the field of medical billing and healthcare finance. CPBs play a pivotal role in ensuring the integrity of revenue cycles, accuracy in claim submissions, and compliance with complex regulatory frameworks. Their responsibilities extend across multiple dimensions of healthcare administration, encompassing coding proficiency, reimbursement analysis, claims processing, documentation review, and adherence to HIPAA and other privacy regulations. By bridging clinical documentation with payer requirements, CPBs protect both providers and patients, mitigating errors, delays, and financial discrepancies.
Achieving CPB certification signifies mastery of these technical competencies, but maintaining the credential requires ongoing dedication. Continuous professional development through webinars, workshops, conferences, and online courses ensures that CPBs remain updated on evolving coding standards, reimbursement methodologies, and regulatory changes. Documentation of continuing education units (CEUs) reinforces accountability and professional credibility, while familiarity with emerging technologies, electronic health records, and automated claims systems enhances operational efficiency and analytical capability. Ethical responsibility remains central, with CPBs serving as stewards of integrity, vigilance, and transparency in all aspects of billing and financial management.
Beyond technical skill, the CPB certification offers substantial opportunities for career advancement. Certified professionals can progress into leadership roles such as revenue cycle managers, compliance specialists, billing supervisors, or healthcare administrators. Specialized knowledge in auditing, payer-specific reimbursement, or coding systems further enables CPBs to provide consultancy, mentor colleagues, and influence organizational strategy. Networking with peers, engaging in professional forums, and participating in industry events enrich both career trajectories and organizational practices, fostering innovation and best practices in healthcare finance.
Ultimately, the CPB credential represents a combination of knowledge, analytical capability, ethical commitment, and professional resilience. Certified Professional Billers are not only indispensable to the operational and financial success of healthcare institutions but also contribute to the delivery of high-quality patient care. Through continuous learning, proactive engagement, and strategic career planning, CPBs uphold the integrity of healthcare billing, maximize reimbursement efficiency, and maintain compliance, ensuring their ongoing relevance and impact within an ever-evolving healthcare environment.