Certification: CPB
Certification Full Name: Certified Professional Biller
Certification Provider: AAPC
Exam Code: CPB
Exam Name: Certified Professional Biller
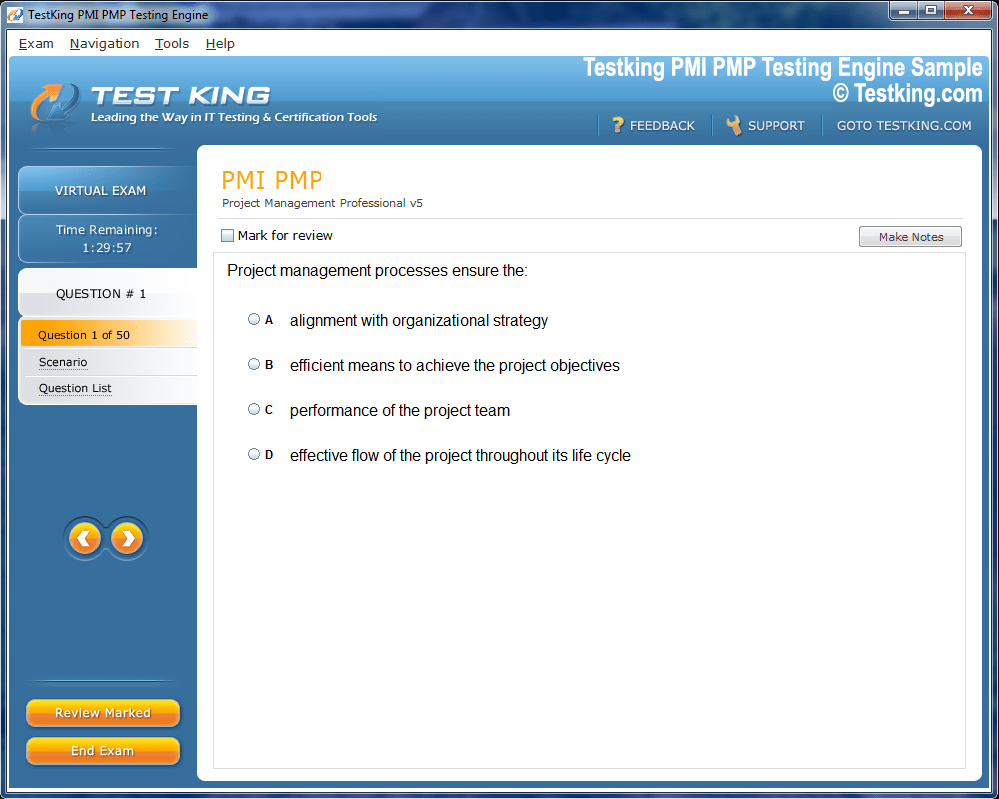
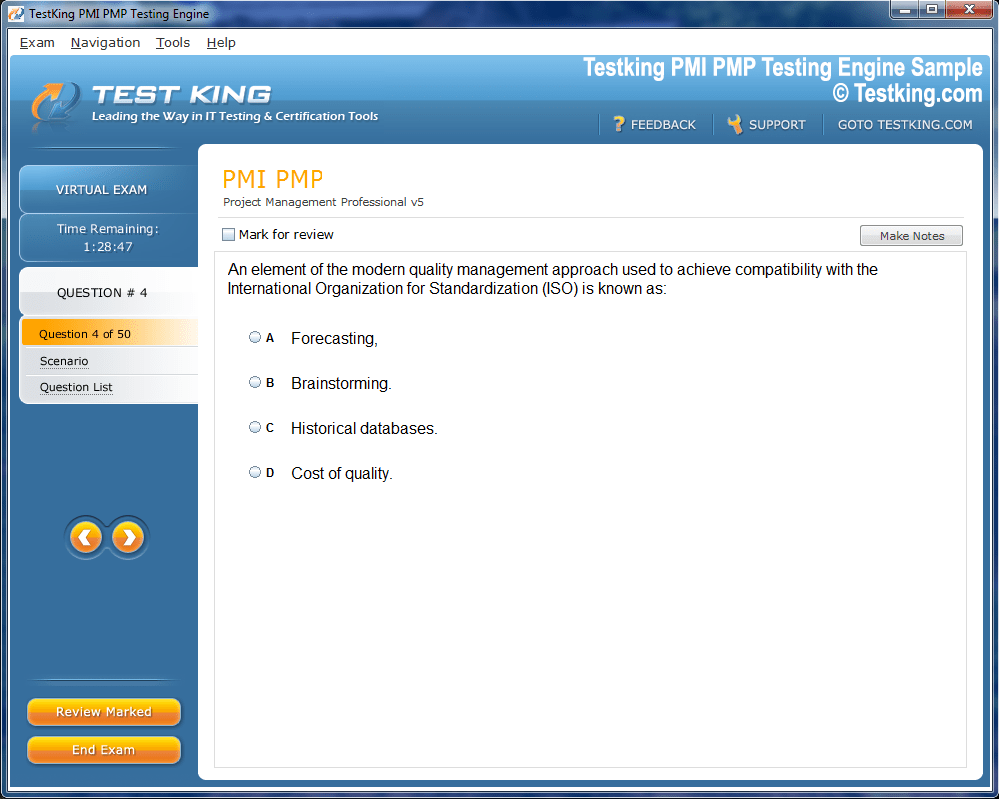
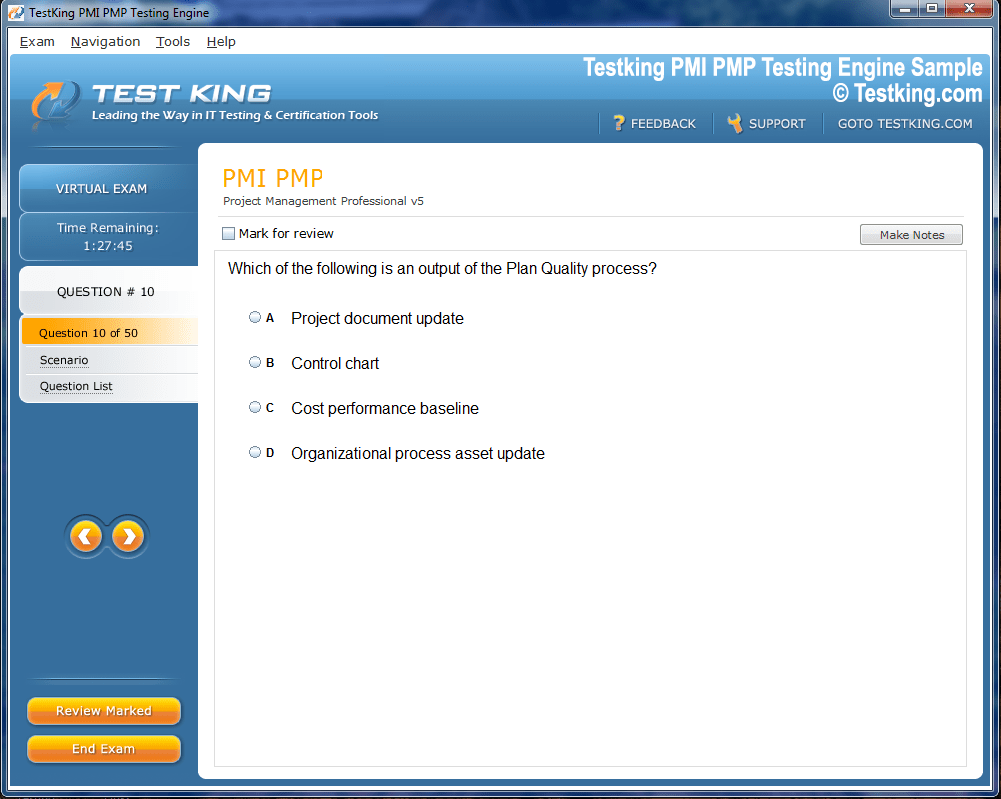
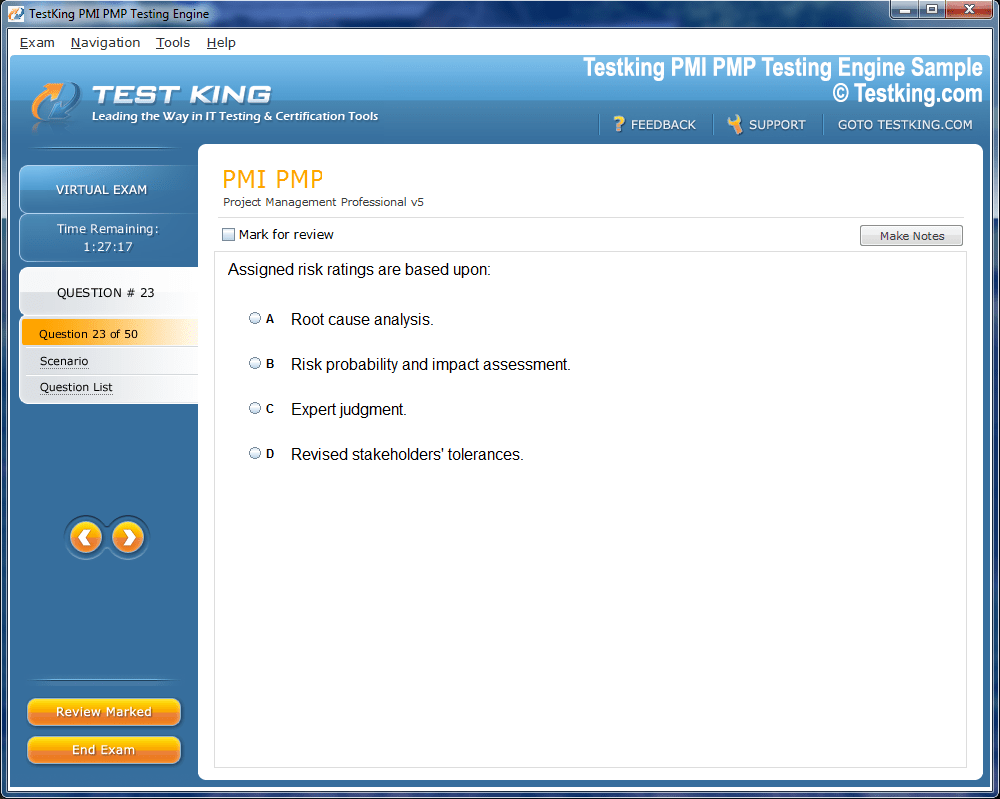
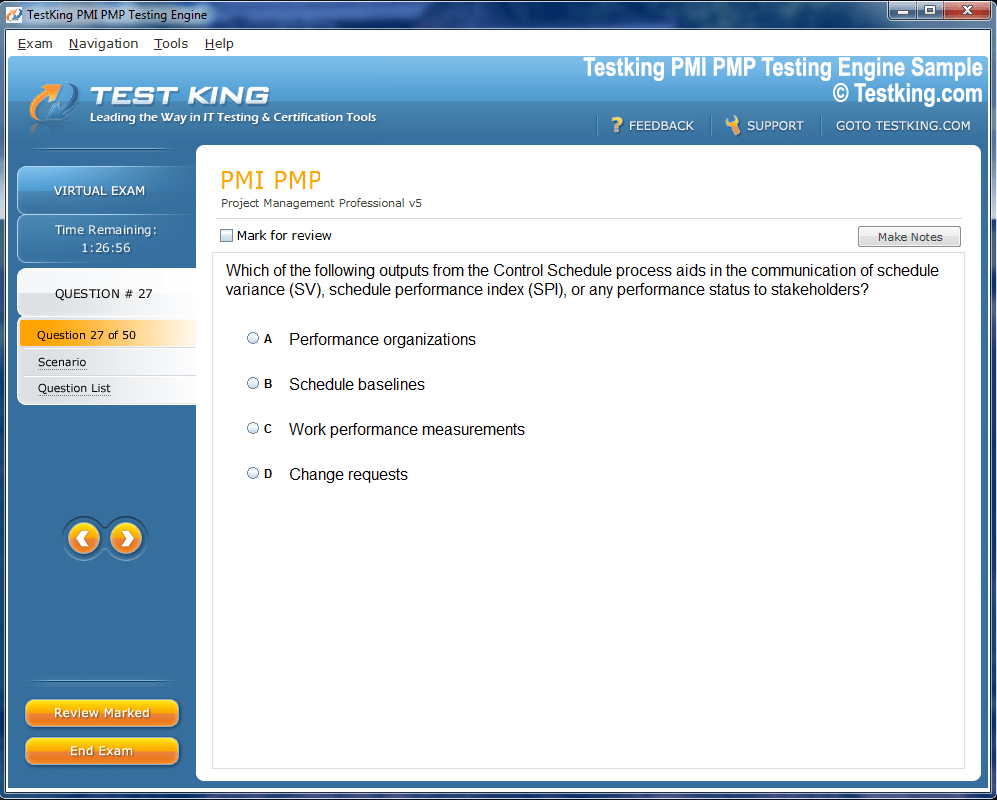
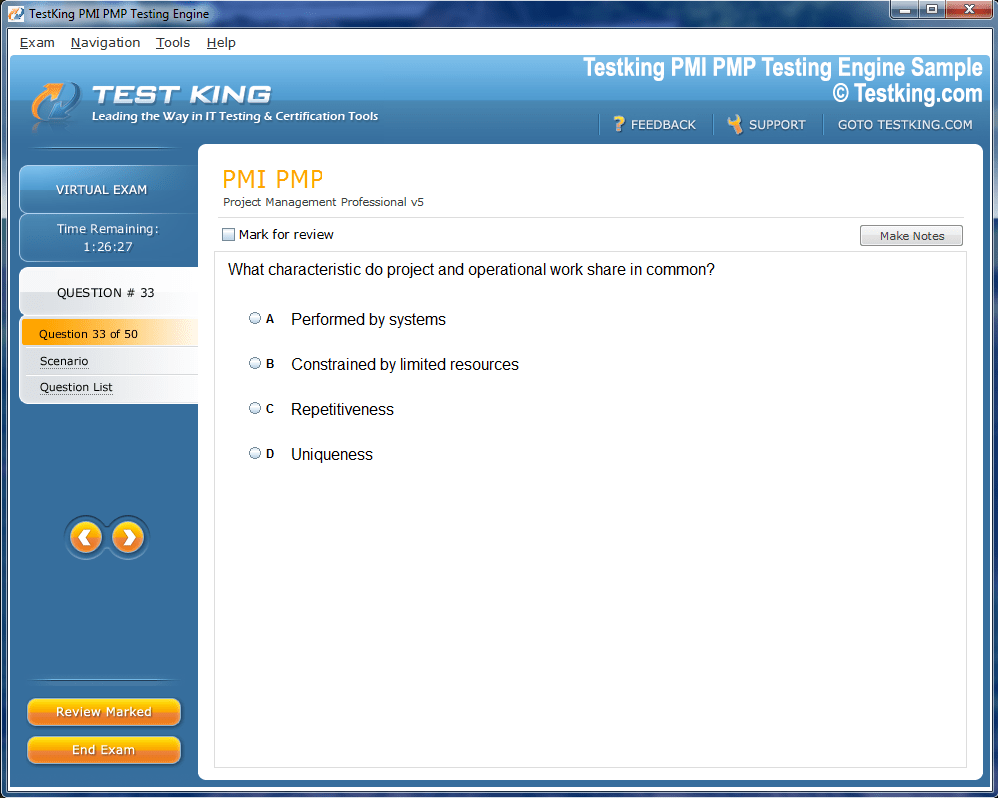
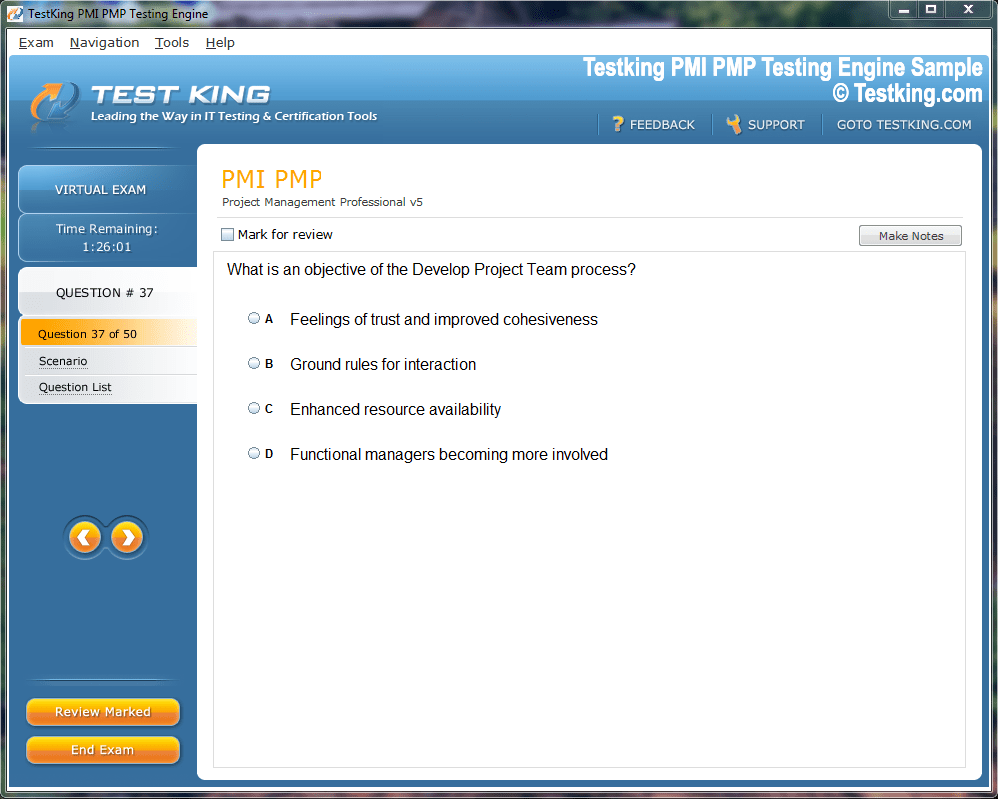
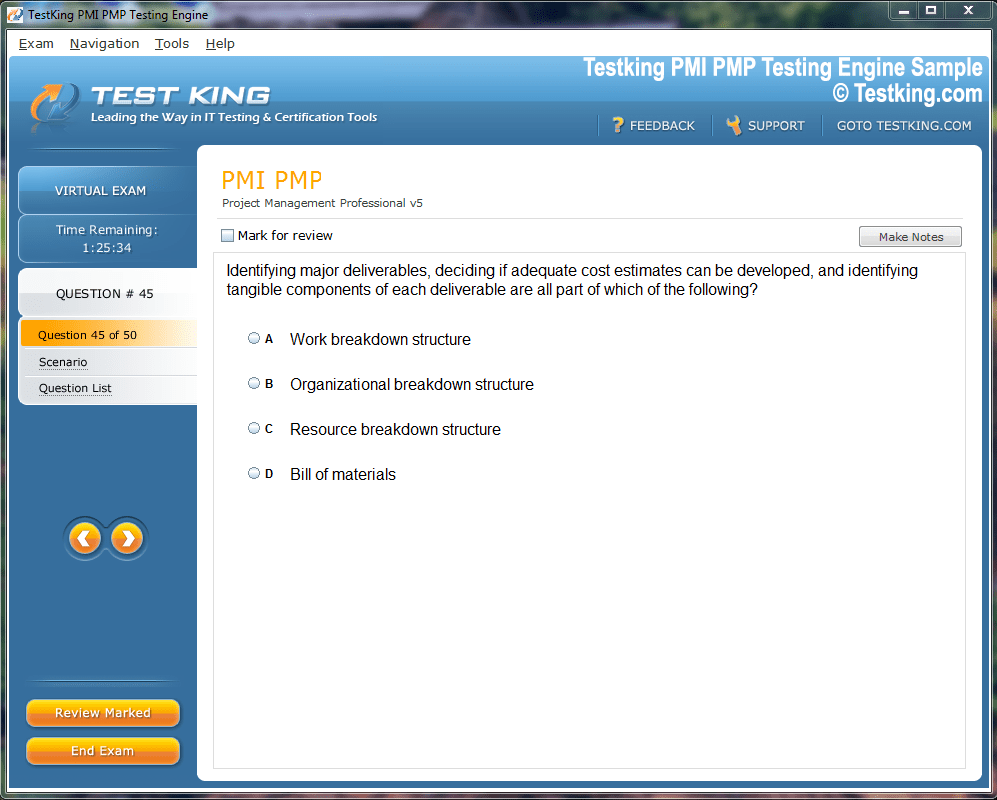
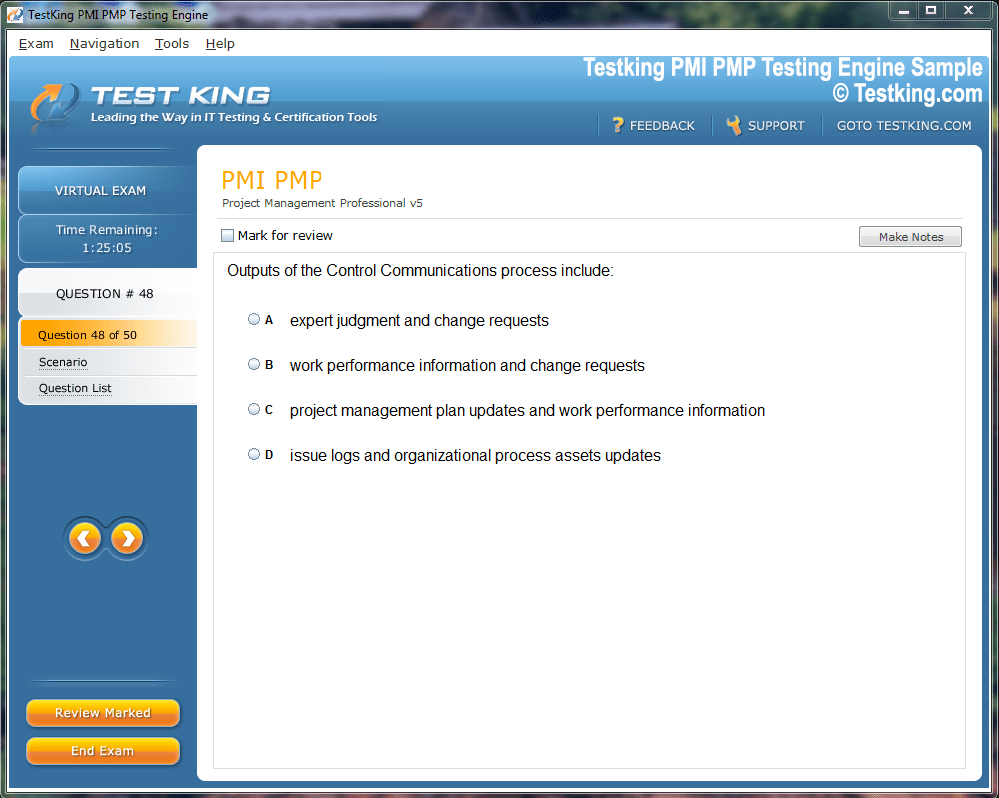
Product Screenshots

nop-1e =1
Unlocking Your Career in Medical Billing: An Introduction to CPB Certification Exam
The healthcare industry is a complex ecosystem, and its financial health relies on a crucial yet often overlooked profession: medical billing. For every patient visit, diagnosis, and procedure, a detailed process must be followed to ensure healthcare providers are properly compensated for their services. This intricate process is the domain of the medical biller. For individuals looking to enter and excel in this field, establishing credibility and demonstrating a high level of expertise is paramount. This is where professional certification plays a pivotal role, with the Certified Professional Biller (CPB) credential standing out as a benchmark of excellence in the industry.
This series will serve as your comprehensive guide to the world of the CPB certification. We will explore everything from the fundamental concepts of medical billing to the specific domains covered in the challenging CPB Exam. We will delve into effective study strategies, examine the career path of a certified professional, and discuss how to maintain and advance your career in this dynamic field. Whether you are just starting to consider a career in medical billing or are an experienced professional seeking to validate your skills, this guide will provide the insights you need to navigate your journey toward becoming a Certified Professional Biller.
What is the Certified Professional Biller (CPB) Certification?
The Certified Professional Biller (CPB) certification is a professional credential designed to validate an individual's skills and knowledge in all aspects of the medical billing process. It demonstrates proficiency in managing the entire revenue cycle, from patient registration to final payment resolution. This certification signifies that a professional has mastered the complexities of claim submission, payer policies, and the regulatory landscape that governs healthcare reimbursement. Holding this credential communicates to employers, colleagues, and providers that you possess a comprehensive understanding of the field and are committed to maintaining the highest professional standards.
Obtaining the CPB certification requires passing a rigorous examination, known as the CPB Exam. This test is carefully designed to assess a candidate's competency across a wide range of topics. These include various insurance models, billing regulations, claim lifecycle management, and compliance with federal laws like HIPAA. The certification is offered by a leading national organization for healthcare business professionals, which ensures that the standards for the credential remain high and are respected throughout the industry. Ultimately, the CPB certification is more than just a title; it is a testament to your expertise and a key that can unlock numerous career opportunities.
The Vital Role of a Medical Biller in Healthcare
A medical biller is the financial backbone of any healthcare practice, clinic, or hospital. Their primary function is to ensure that healthcare providers receive payment for the services they render to patients. This is far from a simple administrative task; it involves a deep understanding of complex coding systems, insurance plan requirements, and government regulations. The biller acts as a critical liaison between the healthcare provider, the patient, and the insurance company. They are responsible for creating accurate and clean claims, which are formal requests for payment submitted to payers like Medicare, Medicaid, or private insurance carriers.
The work of a medical biller directly impacts the financial stability and operational efficiency of a healthcare facility. Errors in the billing process can lead to delayed payments, claim denials, and significant revenue loss. A skilled biller meticulously reviews patient charts and translates medical services into billable charges. They ensure that all required information is present and correct before submitting a claim. Furthermore, they are responsible for tracking the status of submitted claims, appealing any denials, and posting payments once they are received. Their diligence and expertise ensure a steady revenue stream, allowing providers to focus on what they do best: delivering patient care.
Why CPB Certification Matters for Your Career
In a competitive job market, professional certification provides a distinct advantage. The CPB certification immediately elevates your professional standing by formally recognizing your skills. Employers often prioritize certified candidates because it reduces their risk and training costs. A CPB credential serves as third-party validation that you have the necessary knowledge to handle the complexities of medical billing effectively from day one. This can lead to more job interviews, better job offers, and a stronger position when negotiating your salary. The certification acts as a clear signal of your dedication to the profession.
Beyond securing employment, the CPB certification is a catalyst for career growth and increased earning potential. Statistics consistently show that certified professionals earn significantly more than their non-certified counterparts. This credential opens doors to advanced roles, such as billing department supervisor, revenue cycle manager, or compliance specialist. It also equips you with the confidence and knowledge to navigate the challenges of the industry, such as complex claim denials and changing payer rules. Investing in the CPB Exam and achieving certification is a direct investment in your long-term career success and financial well-being.
Understanding the Governing Body Behind the CPB Credential
The CPB certification is administered by a highly respected national organization dedicated to the professional development and certification of individuals in the business side of healthcare. This organization is renowned for setting the industry standard for both medical coding and billing credentials. Its mission is to advance the field by providing education, certification, and networking opportunities for its members. By establishing rigorous standards for its credentials, including the CPB, the organization ensures that certified professionals are well-prepared to meet the demands of the modern healthcare industry.
This governing body is responsible for developing and maintaining the curriculum and content for the CPB Exam. They conduct extensive research and work with subject matter experts to ensure the exam reflects current industry practices, regulations, and challenges. The organization also provides a wealth of resources for candidates preparing for the exam, including official study guides, practice tests, and training programs. Once certified, professionals are required to maintain their credential by completing continuing education units (CEUs), which ensures they stay current with the latest changes in medical billing, a field that is in constant evolution.
Key Differences Between Medical Billing and Coding
While the terms medical billing and medical coding are often used interchangeably, they represent two distinct yet interconnected functions within the healthcare revenue cycle. Medical coding is the process of translating healthcare diagnoses, procedures, medical services, and equipment into universal alphanumeric codes. Coders review clinical documentation from physicians and other providers and assign the appropriate codes from standardized systems like ICD-10-CM, CPT, and HCPCS Level II. The accuracy of these codes is crucial as they provide the foundation for the entire billing process, conveying the "why" and "what" of a patient encounter.
Medical billing, on the other hand, takes the codes created by the medical coder and uses them to create an insurance claim and bill the patient. The biller is responsible for the entire financial transaction process. They generate the claim, verify its accuracy, submit it to the insurance payer, and follow up to ensure it is processed and paid. If a claim is denied, the biller investigates the reason, makes necessary corrections, and manages the appeals process. While a coder's work is focused on translating clinical information into standardized codes, a biller's work is focused on using those codes to secure reimbursement.
Core Competencies of a Certified Professional Biller
The CPB certification validates a professional's competency in several key areas that are essential for success in medical billing. A primary competency is a thorough understanding of the entire revenue cycle management process. This includes everything from patient pre-registration and insurance verification to charge entry, claims submission, payment posting, and denial management. A CPB professional is expected to know how each step influences the next and how to optimize the process for maximum efficiency and reimbursement. This holistic view of the financial lifecycle of a patient account is a hallmark of a certified expert.
Another core competency tested in the CPB Exam is regulatory compliance. This involves a deep knowledge of major healthcare regulations, including the Health Insurance Portability and Accountability Act (HIPAA), the False Claims Act, and Stark Law. A CPB must understand how to handle protected health information (PHI) securely and ethically. They must also be proficient in the rules and guidelines set forth by various government and commercial payers, including Medicare, Medicaid, and private insurers. This knowledge is critical for submitting clean claims and avoiding costly compliance penalties for the healthcare provider.
Furthermore, a CPB must demonstrate expertise in claim submission and follow-up. This includes understanding the nuances of different claim forms, such as the CMS-1500 and UB-04, and knowing how to submit claims electronically. They must be skilled in interpreting explanation of benefits (EOB) and electronic remittance advice (ERA) documents to accurately post payments and identify issues. The ability to effectively investigate and appeal denied claims is a crucial skill. A CPB is trained to analyze denial reasons, gather supporting documentation, and construct compelling appeal letters to overturn incorrect payment decisions from insurance companies.
A Glimpse into the CPB Exam Format
The CPB Exam is designed to be a comprehensive assessment of a candidate's readiness to perform the duties of a professional medical biller. The test consists of multiple-choice questions that cover the full scope of the billing profession. The exam is typically administered in a timed environment, requiring candidates to manage their time effectively to answer all questions. The total number of questions is substantial, ensuring a thorough evaluation of the candidate's knowledge base. It is an open-book exam, but this should not be mistaken for an easy test; it requires knowing how to quickly find information in the approved reference materials.
The questions on the CPB Exam are not just about recalling facts. Many are case-based scenarios that require the test-taker to apply their knowledge to real-world situations. For example, a question might present a patient scenario with specific insurance details and a list of services, asking the candidate to determine the correct billing procedure or identify a compliance issue. This format tests critical thinking and problem-solving skills, which are essential for a biller. To pass, a candidate must achieve a minimum score, demonstrating a high level of proficiency across all tested domains.
Career Opportunities for CPB-Certified Professionals
Achieving CPB certification significantly broadens the scope of career opportunities available to a medical billing professional. Certified billers are in high demand across a variety of healthcare settings. One of the most common environments is a physician's office or a private medical practice, where they may handle all aspects of the revenue cycle for a small team of providers. In larger settings like hospitals or multi-specialty clinics, a CPB may work as part of a larger billing department, potentially specializing in a particular area such as inpatient billing, outpatient billing, or a specific medical specialty like cardiology or orthopedics.
Beyond direct provider settings, CPB-certified professionals can find rewarding careers in other parts of the healthcare industry. Many work for third-party medical billing companies that provide outsourced revenue cycle management services to multiple clients. Opportunities also exist within insurance companies, where a CPB's knowledge is valuable for roles in claims processing and provider relations. Government agencies that administer programs like Medicare and Medicaid also employ billing experts. With experience, a CPB can advance into leadership roles such as billing manager, revenue integrity analyst, or compliance officer, making it a career with a clear path for growth.
The Financial Rewards of Obtaining CPB Certification
One of the most tangible benefits of earning the CPB certification is the positive impact it has on earning potential. Professionals who hold this credential are seen as experts in their field, and this expertise commands a higher salary. Employers are willing to invest more in certified staff because they are more efficient, make fewer errors, and are better equipped to maximize revenue and minimize compliance risks. Data from industry salary surveys consistently shows a significant pay gap between certified and non-certified billers, with certified professionals earning a notable percentage more annually.
The financial return on investment for the CPB certification extends beyond the initial salary increase. The credential is a key to unlocking promotions and more senior positions, each coming with a corresponding pay raise. As a CPB gains experience and possibly pursues further specialized certifications, their value to an organization continues to grow, and so does their compensation. Moreover, the stability that comes with being a highly qualified and in-demand professional provides financial security. The cost associated with preparing for and taking the CPB Exam is an investment that can pay dividends for many years throughout one's career.
Your First Steps Towards Preparing for the CPB Exam
Embarking on the journey to become a Certified Professional Biller begins with a commitment to thorough preparation. The first step is to gain a clear and detailed understanding of the CPB Exam itself. This means obtaining the official exam blueprint from the certifying organization. This document is your roadmap, outlining all the specific knowledge domains, topics, and subtopics that will be covered on the test. Carefully review each section to assess your current knowledge and identify areas where you may have weaknesses. This initial self-assessment is crucial for developing an effective and targeted study plan.
Once you understand the scope of the exam, the next step is to gather your study resources. This includes acquiring the approved codebooks and any other reference materials permitted during the test. You should also consider investing in a dedicated CPB Exam study guide, which can provide a structured curriculum, explanations of complex topics, and valuable practice questions. Many aspiring CPBs also enroll in formal training courses offered by the certifying body or other reputable educational providers. Taking these initial steps with purpose and diligence will lay a strong foundation for your successful preparation and eventual success on the CPB Exam.
How to Strategically Approach Each Domain in Your CPB Exam Prep
To conquer the CPB Exam, you need a strategy that goes beyond simply reading a textbook. A domain-based approach is most effective. Start by using the exam blueprint to rank the domains from highest to lowest percentage. Allocate the majority of your study time to the heavily weighted areas like the revenue cycle and insurance types. For each domain, begin with a high-level review to grasp the main concepts. Then, dive deeper into the specifics, using your study guide and official resources. Create flashcards for key terms, regulations, and acronyms, as this will help with memorization.
Incorporate active learning techniques. Do not just read about the CMS-1500 form; find a sample form online and practice filling it out. Do not just read about HIPAA; think of real-world scenarios where a violation might occur. For regulations like Stark Law, focus on understanding the core principles rather than memorizing every word. As you complete your study of each domain, take a practice quiz or answer practice questions specific to that area. This will help solidify your knowledge and reveal any areas you need to revisit before moving on to the next section.
Common Pitfalls to Avoid in the CPB Exam
Many well-prepared candidates make common mistakes on the CPB Exam that can jeopardize their success. One of the biggest pitfalls is poor time management. With a large number of questions and a strict time limit, it is easy to get bogged down on a few difficult questions. Practice answering questions at a steady pace and learn to flag challenging ones to return to later if time permits. Do not leave any answers blank; make an educated guess if you are unsure, as there is typically no penalty for incorrect answers.
Another common error is misinterpreting the question. The exam questions can be wordy and complex, often presenting a detailed scenario. Read each question and all the possible answers carefully before making a selection. Look for keywords like "not" or "except" that can completely change the meaning of the question. Finally, avoid over-relying on the open-book format. While your books are a valuable resource, you will not have time to look up the answer to every question. The books should be used as a tool to confirm information or look up specific codes or guidelines, not as a primary source of knowledge.
Strategic Preparation for the CPB Exam: Study Resources and Techniques
Passing the rigorous CPB Exam is a significant achievement that requires more than just subject matter knowledge; it demands a strategic and disciplined approach to preparation. Simply reading through study materials is often not enough to ensure success. Candidates must develop a comprehensive study plan, utilize the right resources effectively, and master techniques for both learning the material and performing well on test day. The preparation phase is just as important as the knowledge itself, as it builds the confidence and skills needed to navigate the complexities of the exam under pressure.
This part of the series is dedicated to the art and science of preparing for the CPB Exam. We will move beyond the "what" of the exam blueprint and focus on the "how" of studying. We will explore how to create a personalized study schedule that fits your life, identify the most essential study materials, and leverage practice exams to their full potential. From effective note-taking strategies to managing exam-day anxiety, this guide will provide you with a toolkit of practical, actionable advice to optimize your preparation and maximize your chances of earning the title of Certified Professional Biller.
Creating a Personalized CPB Exam Study Schedule
The foundation of a successful preparation strategy is a well-structured and realistic study schedule. One size does not fit all; your schedule must be tailored to your personal circumstances, including your work hours, family commitments, and learning style. Begin by setting a target date for your CPB Exam. This will give you a clear deadline to work towards. Next, calculate the total number of weeks you have to prepare. A common recommendation is to dedicate at least three to four months to studying, but this can vary based on your prior experience in medical billing.
Once you have your timeframe, break down the CPB Exam blueprint into weekly goals. Assign specific domains or topics to each week, allocating more time to the areas that are either heavily weighted on the exam or are personal weak spots for you. Be specific in your daily planning. Instead of just writing "study," schedule specific tasks like "read chapter on Medicare," "complete 20 practice questions on compliance," or "review flashcards for billing terminology." This level of detail creates accountability and makes the process feel more manageable and less overwhelming. Remember to schedule short breaks and days off to prevent burnout.
Essential Study Materials for CPB Exam Success
Choosing the right study materials is critical for your preparation. Your primary resource should be the official CPB study guide provided by the certifying organization. This guide is specifically designed to align with the exam blueprint and covers all the necessary topics in the required depth. It often includes practice questions and case studies that mimic the format of the actual exam, making it an invaluable tool. Relying on this official resource ensures you are studying the most relevant and up-to-date information, directly from the source.
In addition to the study guide, you will need the current year's editions of the approved codebooks. Even though the CPB Exam is focused on billing, a fundamental understanding of CPT, ICD-10-CM, and HCPCS Level II codes is essential. The exam is open-book, so being familiar with the layout and conventions of these books is crucial for looking up information quickly. Consider purchasing practice exams from reputable sources. These are essential for simulating the test environment and assessing your readiness. Finally, create or purchase a set of flashcards for key terms, acronyms, and regulations to aid in memorization.
The Role of Practice Exams in Your Preparation
Practice exams are one of the most powerful tools in your CPB Exam preparation arsenal. Their primary benefit is to familiarize you with the format, style, and difficulty level of the questions you will encounter on the actual test. This helps to reduce anxiety and build confidence, as the exam format will feel familiar on test day. Taking a full-length, timed practice exam is the best way to simulate the real experience. It helps you build the mental stamina needed to stay focused for the duration of the test and highlights any issues with pacing or time management.
Beyond simulation, practice exams are an excellent diagnostic tool. After completing a practice test, do not just look at your score. Meticulously review every question you got wrong. For each incorrect answer, analyze why you chose it. Did you misunderstand the question? Did you have a gap in your knowledge? Or did you make a careless error? This analysis will reveal your specific weak areas, allowing you to go back to your study materials and reinforce those topics. This iterative process of testing, analyzing, and reviewing is a highly effective way to turn weaknesses into strengths and steadily improve your score.
Effective Note-Taking and Memorization Techniques
Passive reading is an inefficient way to learn and retain complex information. To truly master the material for the CPB Exam, you need to engage in active learning, and effective note-taking is a key part of this. As you read your study guide, summarize key concepts in your own words. This process forces your brain to process the information rather than just passively scanning it. Use methods like the Cornell Note-Taking System or create mind maps to visually connect different concepts. This is especially helpful for understanding the interconnected steps of the revenue cycle or the relationships between different regulations.
For memorization, rote repetition has its limits. Instead, use active recall techniques. Create flashcards with a term or question on one side and the definition or answer on the other. Regularly quiz yourself, and separate the cards into piles of "mastered" and "needs review." This method, known as spaced repetition, is scientifically proven to improve long-term retention. Use mnemonics or acronyms to remember lists or complex rules. For example, you can create a memorable phrase to recall the different parts of Medicare or the key components of a compliance plan.
Leveraging Study Groups and Online Communities
Studying for the CPB Exam can sometimes feel like a solitary journey, but it does not have to be. Joining a study group, whether in-person or virtual, can provide immense benefits. Explaining a complex topic like claim appeals or the Stark Law to a fellow student is a powerful way to solidify your own understanding. Other group members can also offer different perspectives and explain concepts in a way you may not have considered. A study group provides a structure for accountability and can help keep you motivated and on track with your study schedule.
If a local study group is not an option, there are numerous online forums and social media groups dedicated to individuals preparing for the CPB Exam. These communities are a valuable resource for asking questions, sharing study tips, and finding encouragement from peers who are going through the same process. You can learn about what study materials others have found helpful, discuss difficult practice questions, and get reassurance that your challenges are normal. This sense of community can be a powerful motivator and a source of practical advice throughout your preparation journey.
Time Management Strategies for Exam Day
Your performance on the CPB Exam depends not only on what you know but also on how well you manage your time during the test. Before the exam, you should calculate the average amount of time you can spend on each question. For example, if the exam has 150 questions and a 4-hour time limit (240 minutes), you have approximately 1.6 minutes per question. This is your baseline. During the test, do not let yourself get stuck on any single question for too long. If a question is proving to be very difficult, make your best educated guess, flag it, and move on.
The flagging feature is a critical tool. It allows you to quickly mark questions you are unsure about so you can easily return to them at the end if you have time remaining. It is a much better strategy to answer all the questions you are confident about first, securing those points, and then use your remaining time to tackle the more challenging ones. A final strategy is to do a quick review of your answers if you finish early. Use this time to check for any careless errors or to reconsider the questions you flagged.
Understanding the Approved Codebooks for the CPB Exam
The CPB Exam is an open-book exam, which means you are allowed to bring specific reference books into the testing center. It is absolutely essential that you know which books are approved for the specific year you are taking the exam and that you obtain these exact editions. The typically approved books are the CPT Professional Edition, ICD-10-CM, and HCPCS Level II Professional. Using an outdated or unapproved version could result in you not being allowed to use it during the exam.
Becoming proficient with your books before the exam is crucial. You should not be opening your CPT book for the first time on test day. Spend time during your studies tabbing and highlighting key sections. This will help you navigate the books quickly and efficiently under pressure. Practice looking up codes and guidelines so that the process becomes second nature. Remember, the books are a tool, not a crutch. Your primary knowledge should be in your head, with the books serving as a resource to confirm details or look up specific information you have not memorized.
How to Analyze and Learn from Practice Question Mistakes
Simply doing practice questions is not enough; the real learning comes from analyzing your mistakes. For every practice question you answer incorrectly, you should perform a small "autopsy." First, carefully read the question and the correct answer along with its rationale. The rationale is the most important part, as it explains the logic behind the correct choice. Understand not only why the right answer is right, but also why the other options, including the one you chose, are wrong. This deep level of analysis helps to correct misunderstandings and prevent you from making the same mistake again.
Keep a log or journal of your incorrect answers. Categorize them by the domain from the CPB Exam blueprint. Over time, this log will reveal patterns in your errors. You might discover that you consistently struggle with questions related to a specific payer, like Medicaid, or a particular regulation. This data-driven insight allows you to focus your remaining study time with surgical precision on the areas where you need the most improvement. This targeted approach is far more effective than simply re-reading the entire study guide over and over.
Mental and Physical Preparation Before the Test
The days leading up to your CPB Exam are a critical time for mental and physical preparation. Avoid the temptation to cram new information in the last 24 to 48 hours. This is often counterproductive and can increase anxiety and mental fatigue. Instead, use the last day for a light review of your notes, flashcards, or a quick summary of key concepts. Your primary goal should be to relax and build your confidence. Trust in the preparation you have done over the past several months.
Ensure you get a full night of sleep before the exam. A well-rested brain performs significantly better in terms of memory recall and critical thinking. On the morning of the exam, eat a nutritious breakfast and stay hydrated. Avoid excessive caffeine, which can increase nervousness. Plan your route to the testing center in advance and aim to arrive early to avoid any last-minute stress. Practice some simple relaxation techniques, like deep breathing, to calm your nerves before you walk in. A calm and confident mindset is a powerful asset.
Last-Minute Tips for the Day of Your CPB Exam
On the day of the CPB Exam, your focus should be on execution. Double-check that you have all your required materials: your approved identification, your authorization to test, and your approved codebooks. Make sure your books are free of any unapproved notes or materials. When you begin the test, take a moment to read the instructions carefully. As you work through the questions, maintain a steady pace. If you start to feel overwhelmed, take a few deep breaths to reset and refocus.
Trust your instincts. Your first answer is often the correct one, so avoid changing your answers unless you are absolutely certain you made an error. Pay close attention to the wording of each question, as small details can make a big difference. Remember to use the process of elimination to narrow down your choices on difficult multiple-choice questions. Even if you cannot identify the correct answer immediately, you can often eliminate one or two options that are clearly incorrect, which increases your odds of guessing correctly. Walk in prepared, stay calm, and be confident in your abilities.
The Life of a Certified Professional Biller: Responsibilities and Career Path
Earning the CPB certification by passing the CPB Exam is a monumental step in a professional's journey, but it is not the final destination. It is the beginning of a dynamic and rewarding career. The credential opens the door to a world of opportunities and responsibilities that are central to the financial health of the healthcare industry. Life after certification involves applying the vast knowledge gained during your studies to real-world challenges, navigating complex billing scenarios, and continuously adapting to an ever-evolving regulatory landscape. It is a career that demands precision, persistence, and a commitment to lifelong learning.
This part of our series will shift focus from preparing for the exam to embracing the career that follows. We will explore the day-to-day realities of working as a Certified Professional Biller, from the core responsibilities you will manage to the diverse environments you might work in. We will also map out the potential career paths and advancement opportunities that become accessible with the CPB credential. Understanding what to expect after you are certified will help you leverage your new qualification to build a successful and fulfilling long-term career in medical billing.
A Day in the Life of a Certified Professional Biller
The daily routine of a Certified Professional Biller can be both structured and unpredictable. The day often begins by reviewing the previous day's charges to ensure they have been captured correctly and coded accurately. This involves a meticulous check for any missing information or potential errors before the claims are compiled and submitted. A significant portion of the morning might be spent on electronic claim submission, where batches of claims are sent to various insurance payers. The biller must then verify that each batch was successfully received by the payers through confirmation reports.
The afternoon is frequently dedicated to follow-up activities. This includes analyzing incoming correspondence from insurance companies, primarily in the form of Explanation of Benefits (EOBs) and Electronic Remittance Advice (ERAs). The CPB will post payments received, make contractual adjustments to patient accounts, and identify any claims that have been denied or underpaid. The rest of the day may involve investigating these problem claims, contacting insurance company representatives to inquire about claim status, and initiating the appeals process for unfairly denied services. Sprinkled throughout the day are tasks like answering patient billing questions and generating financial reports for management.
Key Responsibilities in a Medical Billing Role
A Certified Professional Biller is entrusted with a wide range of critical responsibilities that directly impact a provider's revenue. A primary duty is ensuring the submission of "clean claims," which are claims that are accurate and complete on the first submission. This requires a sharp eye for detail and a thorough understanding of each payer's specific requirements. This includes verifying patient demographic and insurance information, confirming that medical codes are correct and support medical necessity, and ensuring all necessary fields on the claim form are properly filled out.
Another key responsibility is the management of the accounts receivable (A/R). This involves diligently tracking all submitted claims and actively pursuing payment on any that become overdue. A CPB must be skilled in identifying the root cause of claim denials, whether it is a simple data entry error, a lack of pre-authorization, or a dispute over medical necessity. They are then responsible for correcting the issue and resubmitting the claim or filing a formal appeal. Furthermore, a CPB has the responsibility to maintain strict compliance with all healthcare regulations, including HIPAA, to protect patient privacy and prevent fraud and abuse.
Work Environments: From Hospitals to Private Practices
The CPB certification qualifies professionals to work in a diverse array of settings within the healthcare industry. Many CPBs are employed in small to medium-sized physician practices, where they might be the sole person responsible for the entire revenue cycle. This type of role offers a broad range of experience and a high degree of autonomy. In contrast, working in a large hospital or health system presents a different experience. Here, a CPB is typically part of a large business office and may specialize in a specific area, such as inpatient facility billing, emergency department professional fees, or follow-up for a particular insurance carrier.
Beyond direct patient care facilities, there are many other environments where a CPB can thrive. Third-party billing companies, which handle billing and collections for multiple medical practices, are major employers of certified billers. Insurance companies also hire CPBs for roles in claims examination and processing, where their knowledge of billing practices is invaluable for identifying incorrect claims. Additionally, consulting firms, healthcare technology companies, and even educational institutions have roles for experienced and certified billing professionals, offering a variety of career paths outside the traditional provider setting.
The Importance of Soft Skills for a CPB Professional
While technical knowledge of billing rules and regulations is essential, success as a Certified Professional Biller also hinges on a strong set of soft skills. Communication is paramount. A CPB must be able to communicate clearly and professionally with a wide range of people, including physicians, office staff, patients, and insurance company representatives. They often need to explain complex billing issues to patients in a way that is easy to understand and compassionate. They must also be able to articulate their case effectively when speaking with insurance adjusters to appeal a denied claim.
Problem-solving and critical thinking are also crucial. Medical billing is rarely straightforward, and a CPB is constantly faced with puzzles to solve, such as why a claim was denied or how to interpret a new payer policy. They need an analytical mindset to investigate issues, identify patterns, and develop effective solutions. Strong organizational skills and attention to detail are non-negotiable, as even a small error can lead to a costly denial. Finally, a CPB must be persistent and resilient, as the process of securing payment can often be long and challenging.
Advanced Certifications to Pursue After Your CPB
The CPB certification is a fantastic foundation, but for those with ambitious career goals, it can be the first of several credentials. After gaining experience, you may want to pursue an advanced certification to demonstrate a higher level of expertise in a specialized area. For example, if you find yourself drawn to the compliance side of healthcare, you could pursue a certification as a Certified Professional Compliance Officer (CPCO). This credential validates your knowledge in developing and managing a healthcare compliance program.
If you enjoy the analytical and investigative aspects of the job, a certification as a Certified Professional Medical Auditor (CPMA) could be an excellent next step. This would qualify you to perform audits of medical records and claims to ensure they are compliant and accurately reflect the services provided. These advanced certifications signal to employers that you are a dedicated expert in your chosen specialty. They are often a prerequisite for senior-level management and executive positions within the revenue cycle and compliance departments.
Conclusion
Auditing is a critical function for ensuring the integrity and financial health of a healthcare practice, and a CPB plays an important role in this process. While a formal audit is often conducted by a certified auditor, the CPB is involved in both internal and external audits. Internal audits are proactive reviews of claims and billing processes, conducted to identify and correct problems before they lead to external scrutiny. A CPB might assist in these audits by pulling requested data, reviewing claims for accuracy, and helping to identify patterns of errors.
External audits are conducted by outside entities, such as Medicare, Medicaid, or a commercial insurance company. These can be stressful, as they can result in demands for repayment and even penalties if significant errors are found. A CPB is crucial during an external audit. They are responsible for gathering and organizing the requested documentation, responding to inquiries from the auditor, and helping to formulate a response to any negative findings. A strong knowledge of billing and compliance is essential to successfully navigate these audits.
Effective communication is a thread that runs through every aspect of a successful CPB's career. Building a professional and respectful relationship with the provider representatives at the insurance companies you deal with most frequently can be incredibly beneficial. When you have a good working relationship, it can be easier to get answers to complex questions, resolve issues, and even get help navigating the payer's internal bureaucracy. Always be polite, professional, and well-prepared when you contact a payer.
Equally important is building strong communication channels with the clinical providers and administrative staff within your own organization. A CPB must be able to educate physicians and other clinicians on the importance of clear and thorough documentation and explain how their documentation directly impacts reimbursement. They must also work collaboratively with front desk staff to improve processes like insurance verification and data collection. A CPB who is an effective communicator acts as a vital link, connecting the clinical and financial sides of the practice to ensure a smooth and successful revenue cycle.
Your career after passing the CPB Exam should be guided by a long-term strategy. Think about where you want to be in five, ten, and fifteen years. Do you aspire to be a billing manager, a compliance officer, a consultant, or perhaps even run your own billing company? Once you have a goal in mind, you can start taking intentional steps to get there. Seek out projects and responsibilities in your current role that will help you develop the skills you need for your desired future role.
Continuously invest in your education, pursuing additional certifications or even a formal degree if it aligns with your goals. Find a mentor, an experienced professional who can provide guidance and support. Stay active in your professional association and build a strong network. The CPB certification is a powerful tool, but it is your strategic vision, your commitment to learning, and your professional drive that will ultimately shape the trajectory of your career. Use it as a foundation to build a future as a respected and successful leader in the business of healthcare.
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How often do you update the questions?
Testking strives to provide you with the latest questions in every exam pool. Therefore, updates in our exams/questions will depend on the changes provided by original vendors. We update our products as soon as we know of the change introduced, and have it confirmed by our team of experts.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.


