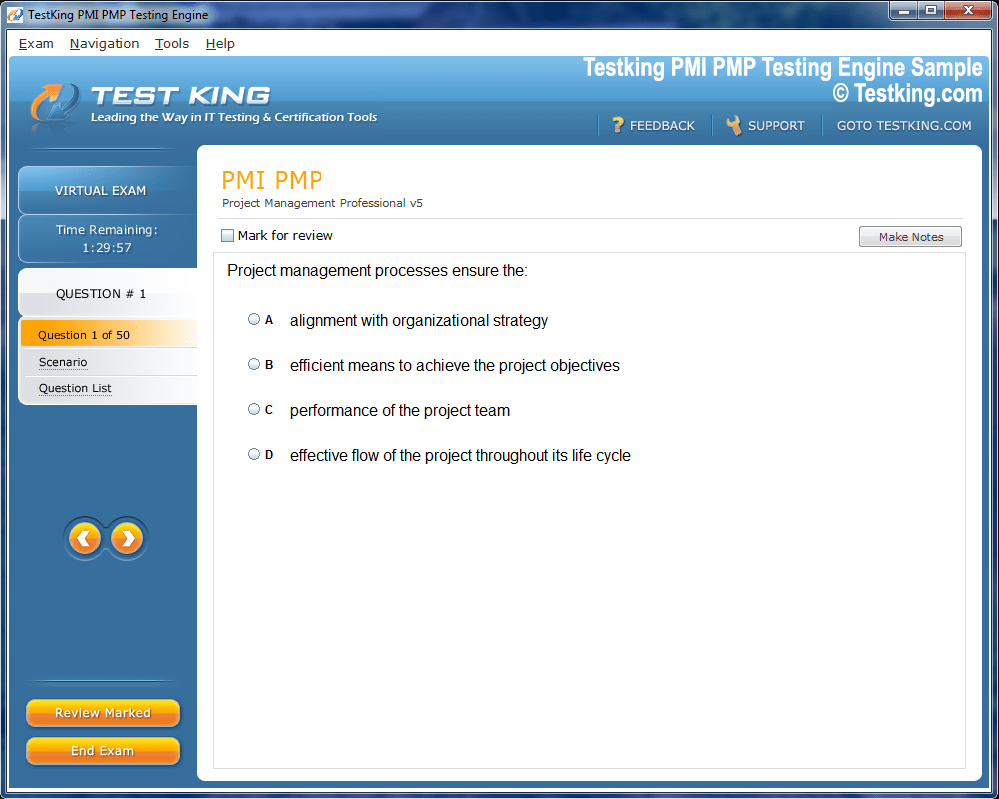
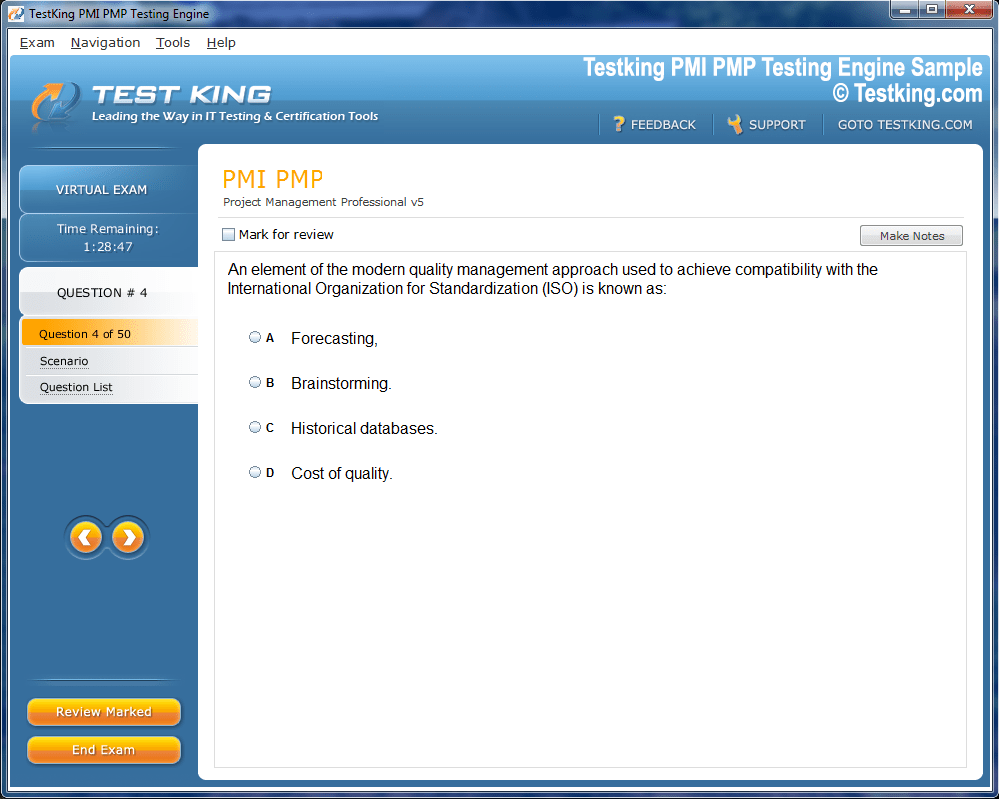
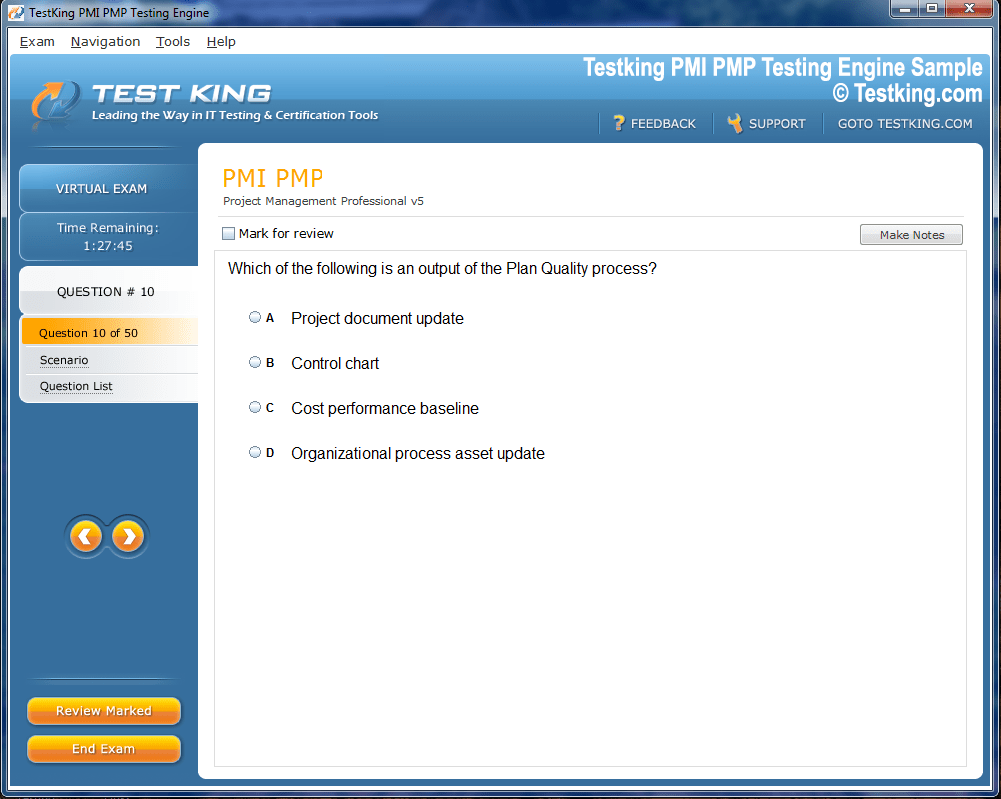
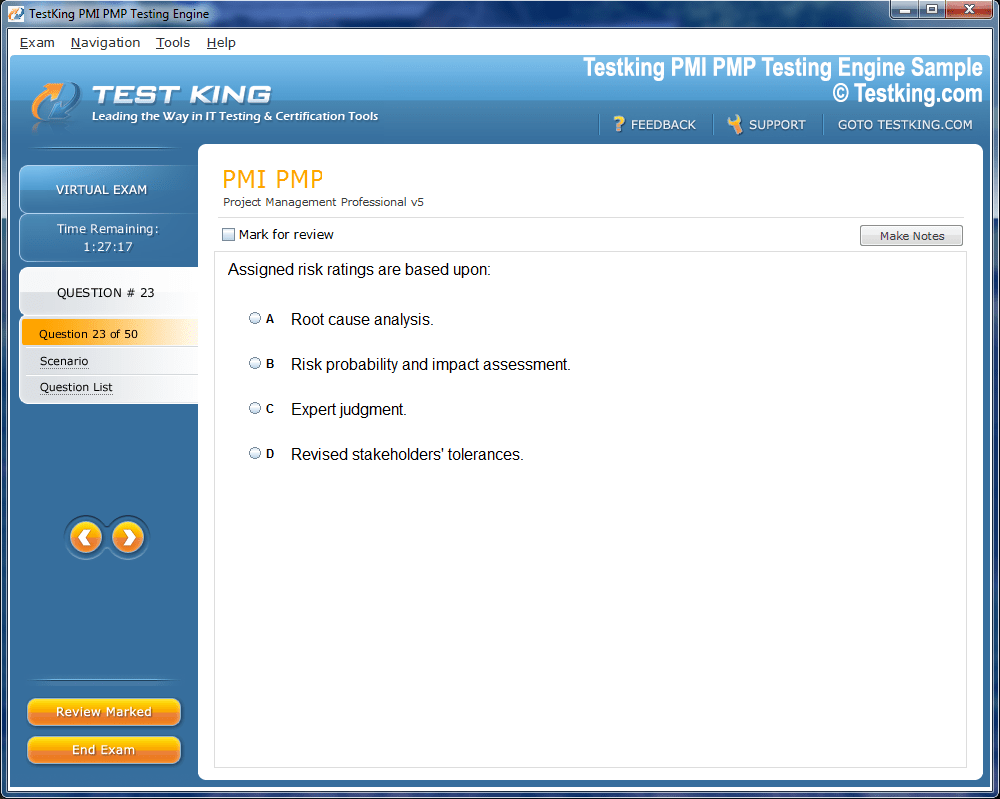
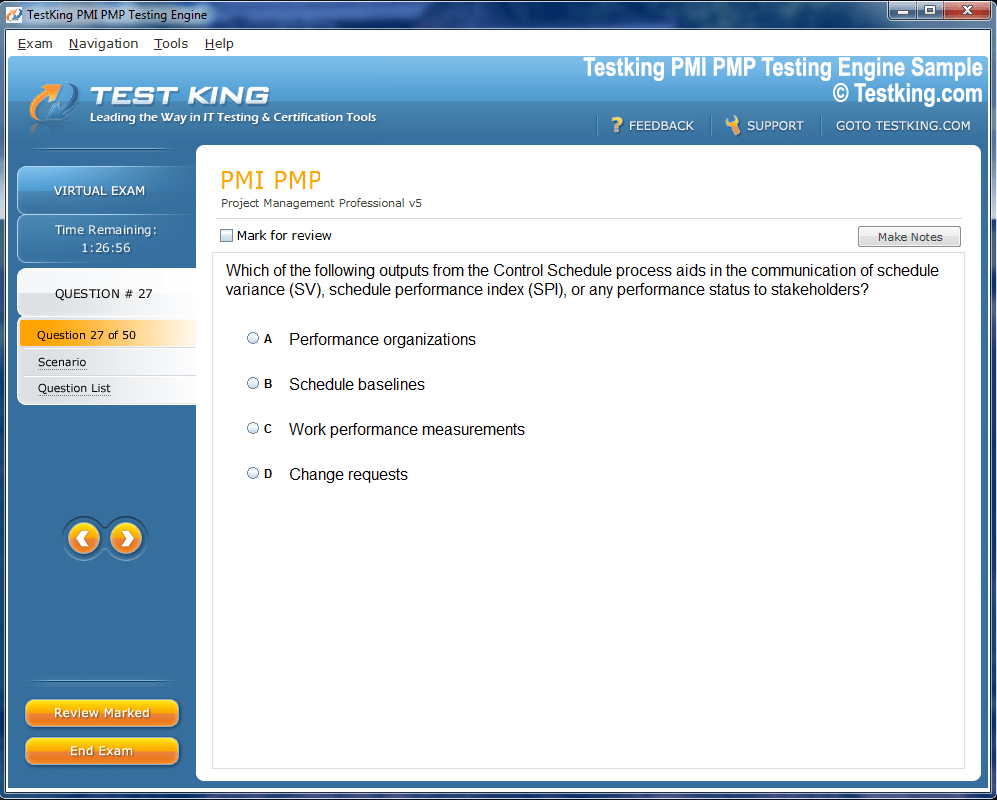
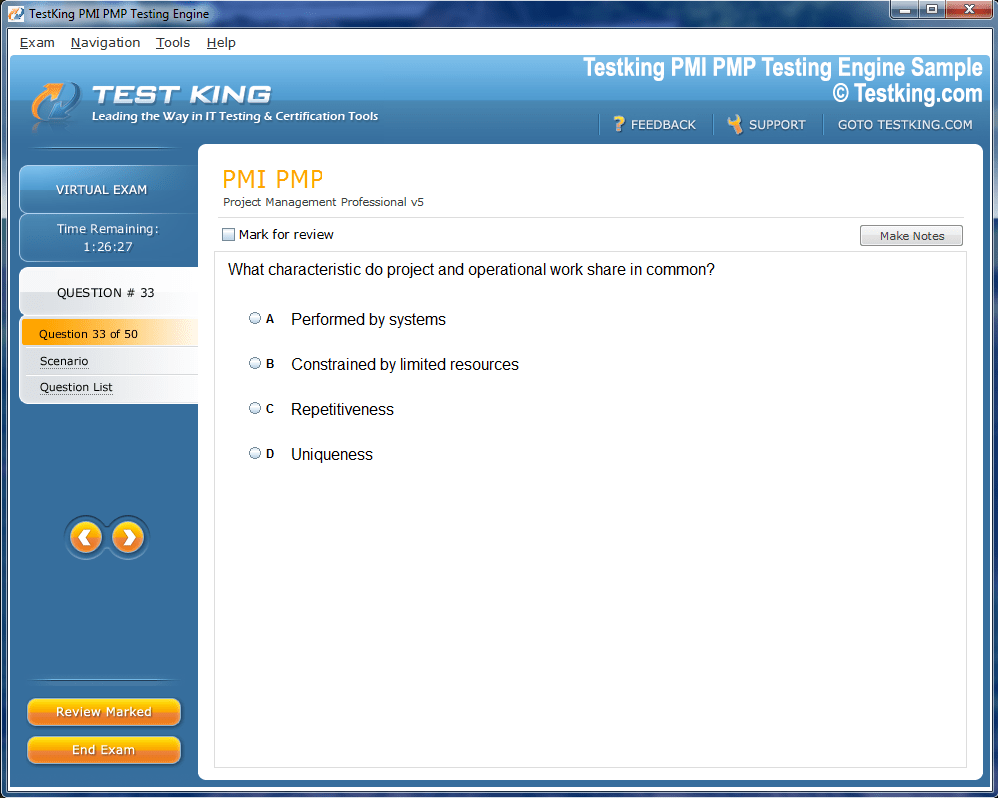
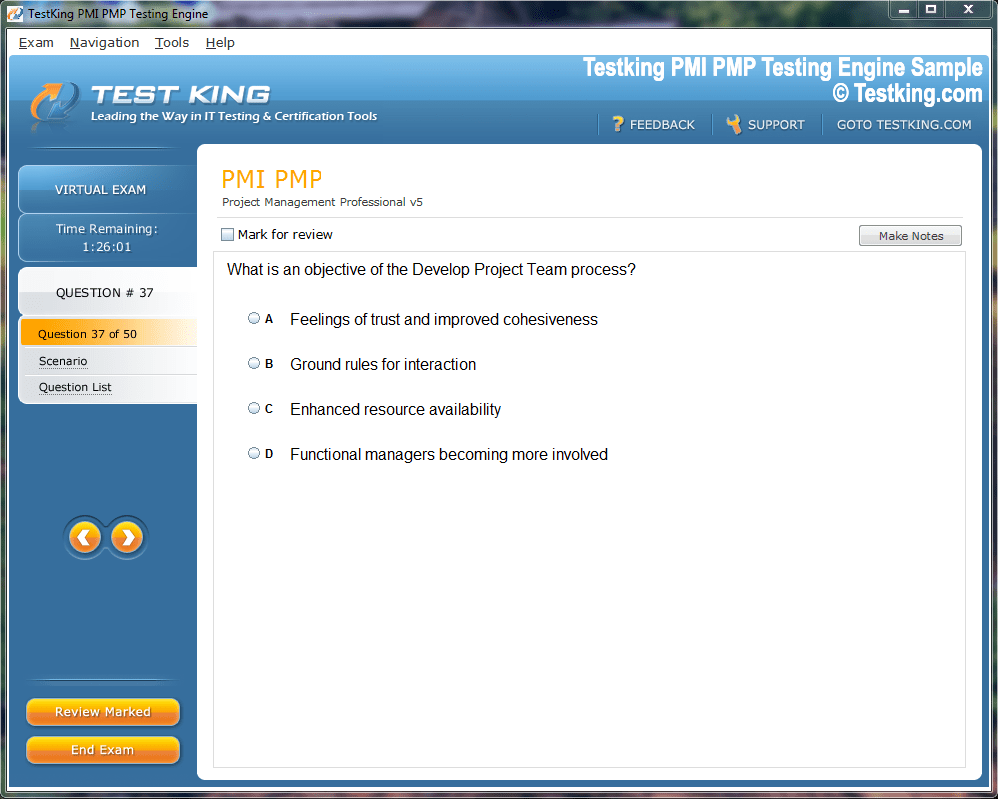
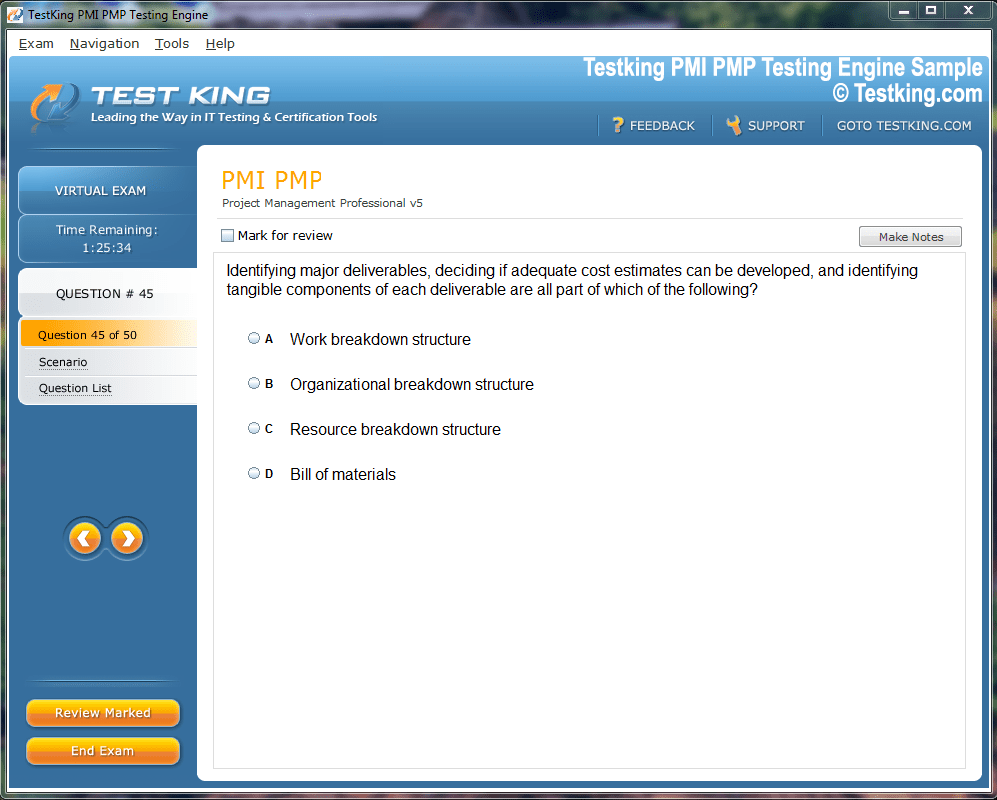
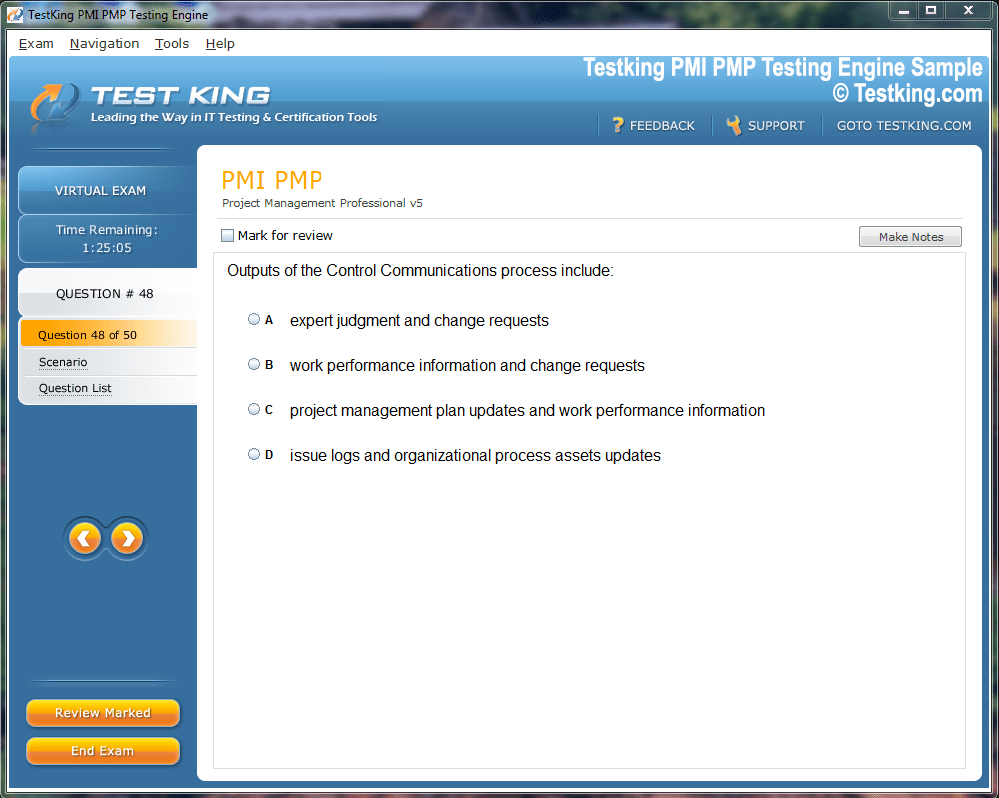
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our CIC testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Building Competent Infection Preventionists With CBIC CIC
For many infection preventionists, achieving Certification in Infection Control (CIC) represents more than a credential; it is a professional milestone that signifies both mastery of foundational concepts and a commitment to excellence in patient safety. Infection prevention as a discipline demands a complex amalgamation of epidemiology, clinical insight, and strategic program management. Consequently, professional certification functions as an emblem of competency, not only validating knowledge but also fostering confidence among early-career practitioners navigating the intricate healthcare landscape.
Organizations such as the Association for Professionals in Infection Control and Epidemiology have long advocated for certification as a critical element of professional development. Certification provides a standardized measure of aptitude that assures both employers and patients that an infection preventionist has met rigorous criteria for knowledge and practical capability. Within the healthcare ecosystem, CIC-certified professionals are often viewed as integral contributors to the cultivation of safety cultures, compliance with regulatory standards, and the implementation of evidence-based interventions.
Infection Prevention & Management Associates (IP&MA) exemplifies an organizational approach that prioritizes certification. Their work encompasses a spectrum of activities, including the creation of comprehensive infection prevention programs, the management of onsite operational structures, and educational initiatives tailored for both novice and experienced practitioners. IP&MA’s philosophy underscores the belief that early-career infection preventionists, often coming from public health or epidemiology backgrounds, require structured support to transition effectively into clinical settings where practical application of knowledge is paramount.
The journey toward CIC certification for a novice infection preventionist can be daunting. New professionals encounter diverse healthcare environments, each with unique operational, regulatory, and cultural characteristics. The ability to interpret surveillance data, implement intervention protocols, and assess outcomes requires not only theoretical understanding but also the cultivation of practical intuition. Certification serves as both a catalyst and a benchmark, providing early-career infection preventionists with a structured path to demonstrate their competency across these multifaceted domains.
Early-Career Development and Professional Expectations
Within organizations like IP&MA, recruitment strategies often emphasize the potential of early-career candidates with master's level education in public health or epidemiology. These individuals may possess considerable academic preparation but minimal exposure to direct clinical operations. Structured onboarding, therefore, becomes essential in bridging the gap between theoretical expertise and applied practice. Training programs designed for these professionals aim to instill core competencies in infection prevention while simultaneously nurturing the critical thinking and decision-making skills necessary for complex healthcare environments.
Leaders within IP&MA articulate a clear expectation: certification is integral to professional development. This expectation is not merely procedural but strategic, reflecting an understanding that structured certification pathways accelerate skill acquisition and promote career progression. For professionals from underrepresented or nontraditional backgrounds, obtaining CIC certification can serve as a potent equalizer, affirming their competence in ways that transcend prior experience or demographic factors. The credential offers a codified recognition of skill that aligns with industry standards and supports career mobility.
Infection preventionists encounter numerous challenges when entering the field. Clinical protocols evolve rapidly, technological platforms for surveillance and data analysis advance continuously, and healthcare institutions vary widely in organizational culture and policy emphasis. Certification functions as an anchor amidst this fluidity, enabling practitioners to navigate divergent contexts while maintaining consistency in practice standards. Moreover, the certification process itself reinforces professional rigor, compelling early-career infection preventionists to engage deeply with both foundational knowledge and contemporary best practices.
Structured Training and Knowledge Integration
IP&MA has developed an approach to early-career training that integrates multiple modalities of learning to optimize competency development. Novice infection preventionists undergo an initial three-month onboarding period designed to establish a foundational understanding of infection control practices. During this phase, practitioners learn to interpret epidemiologic data, recognize patterns indicative of potential outbreaks, and implement standardized preventive interventions. The onboarding process emphasizes practical application, ensuring that theoretical knowledge is immediately translatable into operational effectiveness.
Following the initial phase, practitioners progress through a structured series of modules designed to expand both breadth and depth of competence. These modules cover critical domains such as program development, risk assessment, outbreak investigation, and compliance with regulatory frameworks. Training is intentionally multimodal, incorporating self-directed learning through authoritative guidance documents, cohort-based lectures that foster collaborative engagement, and assessment quizzes that reinforce knowledge acquisition. Each participant is paired with an advanced-practice mentor as well as a near-peer mentor to facilitate experiential learning, model effective skill application, and validate competency through practical demonstration.
This blended methodology addresses the inherent variability of clinical environments by fostering both independent learning and collaborative problem-solving. Novice practitioners gain exposure to diverse operational scenarios while receiving structured support, which enhances both confidence and skill retention. Mentorship serves as a conduit for tacit knowledge transfer, allowing new infection preventionists to navigate the subtleties of organizational culture and workflow that are not readily captured in textbooks or formal curricula.
Certification Preparation and Competency Validation
Once foundational skills are established and competency validated, the training program transitions toward specific preparation for the CIC examination. This phase is characterized by self-paced, asynchronous learning, which accommodates the variable schedules and geographic distribution of practitioners across facilities. Training materials include recorded sessions aligned with the CIC content outline, study guides designed to identify areas of individual focus, and practice examinations aimed at reducing test anxiety and reinforcing knowledge retention.
The practice examination component is particularly significant, as it provides a simulated testing environment that enables practitioners to gauge readiness and adjust study strategies accordingly. For individuals who have delayed certification due to uncertainty or limited prior exposure, these resources mitigate apprehension and enhance performance outcomes. The integration of mentorship, hands-on practice, and self-guided study ensures that early-career infection preventionists are not only theoretically prepared but also equipped with the practical judgment necessary for real-world application of infection control principles.
Certification has implications beyond individual achievement; it enhances organizational capacity to deliver consistent, evidence-based interventions. CIC-certified practitioners bring standardized competencies to their teams, improving the reliability of infection prevention programs and contributing to safer patient environments. As infection prevention increasingly intersects with public health imperatives, epidemiologic surveillance, and policy compliance, certified professionals serve as pivotal agents in advancing institutional and community health objectives.
Organizational Impact and Workforce Advancement
IP&MA’s commitment to structured training and certification underscores a broader philosophy regarding workforce development. By embedding certification expectations within professional development pathways, organizations can cultivate a cadre of practitioners who are capable of assuming leadership roles, implementing sophisticated programs, and mentoring subsequent generations of infection preventionists. This investment in skill development translates into measurable improvements in program quality, operational efficiency, and patient safety outcomes.
A structured certification pathway also enhances retention and professional satisfaction. Early-career infection preventionists who receive comprehensive training and mentorship are more likely to engage fully with their roles and pursue continued professional growth. Certification provides tangible recognition of achievement, reinforcing commitment and fostering a sense of professional identity within a demanding field. For organizations, this translates into reduced turnover, increased institutional knowledge, and a more resilient workforce capable of adapting to emergent challenges in healthcare delivery.
The strategic integration of training, mentorship, and certification aligns with contemporary models of workforce development, which emphasize competency-based progression, evidence-informed practice, and continuous professional improvement. By adopting these principles, organizations like IP&MA not only support the growth of individual practitioners but also contribute to the evolution of infection prevention as a professional discipline.
Cultivating Expertise Across Diverse Backgrounds
A notable aspect of IP&MA’s approach is the deliberate inclusion of professionals from diverse educational and cultural backgrounds. Historically underrepresented groups entering the field benefit from structured pathways that validate competency and provide equitable opportunities for advancement. Certification serves as a unifying standard, ensuring that skill acquisition is recognized independently of prior institutional experience or demographic factors.
This focus on inclusivity has broader implications for the infection prevention workforce. Diversity enriches problem-solving capacity, encourages innovation in intervention strategies, and enhances the cultural competence of programs. By integrating certification within this framework, organizations affirm both the capability and the professional legitimacy of practitioners who may have faced systemic barriers in traditional career trajectories.
Mentorship plays a critical role in this context, facilitating both knowledge transfer and socialization into professional norms. Pairing novice infection preventionists with experienced practitioners allows for the transmission of nuanced skills, organizational insight, and strategic judgment that cannot be fully captured in formal curricula. Simultaneously, near-peer mentors provide relatable guidance and modeling, bridging the gap between theoretical understanding and practical application.
Structuring Training for Early-Career Infection Preventionists
The foundation of effective infection prevention practice lies not only in theoretical understanding but in the ability to apply knowledge consistently across diverse clinical environments. For early-career infection preventionists, structured training programs serve as the cornerstone of professional development, offering a scaffolded approach to acquiring competencies, navigating operational complexities, and ultimately achieving Certification in Infection Control (CIC). Organizations that emphasize comprehensive onboarding, integrated mentorship, and iterative skills reinforcement provide practitioners with the tools necessary to meet both immediate and long-term professional challenges.
Structured training programs begin with the recognition that novice infection preventionists often enter clinical practice with limited exposure to direct patient care environments. These practitioners may possess advanced degrees in public health, epidemiology, or related disciplines, yet the translation of academic knowledge into practical skill requires intentional guidance. An initial phase of onboarding, typically spanning three months, introduces foundational infection prevention concepts and protocols. Participants are exposed to core operational procedures, surveillance methodologies, and regulatory requirements, ensuring they acquire a functional understanding of the workplace context.
During this onboarding period, early-career practitioners learn to interpret epidemiologic data, monitor infection trends, and identify potential risks. Training emphasizes practical engagement, such as participating in focused quality improvement projects or conducting preliminary audits, which allows learners to internalize knowledge through direct application. This experiential approach not only fosters competency but also instills a sense of professional efficacy, crucial for practitioners adapting to multifaceted healthcare settings.
Multi-Modal Learning and Knowledge Reinforcement
Following the initial orientation, training programs typically expand to a series of modular learning experiences designed to cultivate comprehensive competency. Modules address critical domains including outbreak investigation, program design, risk assessment, compliance with national and local regulations, and interdisciplinary collaboration. A multi-modal learning framework integrates self-guided study, live cohort-based instruction, and ongoing evaluation, ensuring that practitioners absorb content through complementary avenues. Self-directed learning often involves authoritative guidelines, evidence-based protocols, and essential reference materials, allowing participants to develop autonomy and critical analysis skills.
Live cohort sessions serve as opportunities for interactive engagement, enabling participants to discuss case studies, simulate problem-solving scenarios, and collaborate on intervention planning. This format promotes dialogue and knowledge exchange, fostering the development of both technical expertise and professional judgment. Quizzes and knowledge assessments embedded throughout the modules function as reinforcement mechanisms, helping learners consolidate understanding while identifying areas requiring additional focus. These iterative assessments support a continuous feedback loop, enabling participants to refine their approach and internalize concepts more effectively.
Mentorship is a pivotal component of structured training programs. Novice infection preventionists are paired with advanced-practice mentors who provide both technical guidance and strategic insight. Mentors facilitate the application of theoretical knowledge to operational scenarios, model professional behaviors, and offer constructive feedback. In addition, near-peer mentors—practitioners slightly more advanced in their careers—provide relatable examples of skill application, reinforcing learning through demonstration. The combination of expert guidance and near-peer support ensures that early-career practitioners gain a holistic understanding of both procedural standards and workplace dynamics.
Bridging the Gap Between Knowledge and Practice
The transition from academic preparation to operational competence presents a critical challenge for early-career infection preventionists. Structured training programs address this gap by integrating hands-on experience with theoretical learning, enabling practitioners to apply concepts within authentic clinical contexts. Participants engage in activities such as conducting risk assessments, evaluating infection control compliance, and implementing preventive interventions under the guidance of mentors. These experiences reinforce the connection between knowledge and practical application, cultivating confidence in decision-making and situational analysis.
Operational immersion also exposes practitioners to variability across healthcare settings. Infection preventionists may rotate through multiple facilities, experiencing differences in organizational culture, workflow, and patient populations. Structured training ensures consistency in core practices while allowing for adaptive learning, preparing participants to apply standardized principles across heterogeneous environments. This approach not only strengthens individual competence but also enhances organizational resilience by promoting uniformity in infection prevention strategies across multiple sites.
Certification-Focused Preparation
As practitioners advance through training, preparation for the CIC examination becomes a central focus. This phase integrates self-paced, asynchronous learning with structured review materials aligned with the examination content outline. Recorded lectures, study guides, and targeted practice exercises enable participants to address knowledge gaps while accommodating their professional responsibilities. Practice examinations provide a simulated testing environment, helping to mitigate anxiety and build familiarity with exam structure and question types.
For early-career infection preventionists who may have deferred certification due to limited exposure or apprehension, these preparatory resources are critical. By allowing learners to assess their readiness and receive targeted feedback, structured preparation reinforces both knowledge acquisition and confidence. Certification preparation is not treated as a separate endeavor but as an extension of ongoing competency development, integrating seamlessly with experiential learning and mentorship support.
Mentorship as a Catalyst for Competency
Mentorship serves as a fulcrum for bridging the theoretical and practical dimensions of infection prevention. Advanced practitioners guide novices through the application of surveillance techniques, outbreak response protocols, and programmatic interventions. Near-peer mentors demonstrate the operationalization of knowledge in real-world scenarios, modeling effective communication, decision-making, and workflow integration. This layered mentorship structure ensures that early-career practitioners receive diverse perspectives, facilitating comprehensive skill development and professional socialization.
The benefits of mentorship extend beyond technical competency. Mentors provide emotional support, encouragement, and validation, fostering resilience and motivation among novice practitioners. By modeling professional comportment and strategic thinking, mentors cultivate both the cognitive and behavioral aspects of competence, enabling early-career infection preventionists to approach complex challenges with confidence and poise.
Expanding Training Beyond Organizational Boundaries
Organizations with well-developed training models often extend their programs to support practitioners outside their immediate workforce. This approach facilitates the dissemination of best practices, promotes consistency across institutions, and addresses gaps in training resources for underrepresented or geographically isolated infection preventionists. External participants engage in structured onboarding, modular learning, mentorship, and certification preparation, benefiting from the same rigorous framework employed internally.
Such expansion not only enhances workforce capability but also contributes to the broader professional ecosystem. Early-career practitioners from diverse backgrounds gain access to structured development opportunities, leveling the playing field for those entering the field without extensive institutional support. By sharing training models across organizations, experienced entities reinforce the standardization of infection prevention practices while fostering a collaborative professional community.
Evaluating Program Efficacy
The effectiveness of structured training programs is measured through both competency assessment and certification outcomes. Knowledge acquisition is evaluated through quizzes, module assessments, and practical exercises, while operational proficiency is validated through mentorship feedback and hands-on demonstrations. The ultimate indicator of success is performance on the CIC examination, which serves as an external benchmark for competency. High pass rates reflect the program’s ability to translate training into demonstrable expertise, confirming that participants are prepared to meet professional standards.
Regular program evaluation supports continuous improvement. By analyzing assessment data, participant feedback, and certification outcomes, training programs can adapt curricula, refine methodologies, and address evolving professional requirements. This iterative process ensures that training remains relevant, effective, and aligned with contemporary infection prevention challenges.
Building Confidence Through Practical Application
Practical application is essential for consolidating learning and reinforcing confidence. Novice infection preventionists engage in activities such as outbreak investigation simulations, risk assessment projects, and compliance audits. These exercises provide immediate feedback on decision-making, technical execution, and professional judgment, allowing learners to internalize best practices. Confidence gained through hands-on experience translates into enhanced performance in both routine and emergent scenarios, enabling early-career practitioners to navigate the complexities of infection prevention with agility and assurance.
Consistency in practice is another key outcome of structured training. Exposure to diverse facilities and patient populations, combined with mentorship guidance, equips practitioners to apply standardized infection prevention protocols while accommodating contextual variability. This balance of uniformity and adaptability is critical for effective infection control across multifaceted healthcare environments.
Mentorship and Long-Term Professional Growth
Mentorship contributes not only to immediate competency development but also to long-term professional growth. Early-career infection preventionists benefit from guidance on career pathways, skill enhancement, and leadership development. Mentors facilitate goal setting, strategic planning, and reflective practice, enabling practitioners to envision trajectories that encompass clinical proficiency, programmatic leadership, and eventual mentorship of future cohorts.
The relational dimension of mentorship also fosters professional identity formation. Novice practitioners internalize organizational values, ethical standards, and professional norms through sustained interaction with experienced mentors. This integration of technical expertise and professional comportment underpins the evolution of competent, resilient infection preventionists capable of contributing meaningfully to patient safety initiatives.
Standardizing Competency Across Diverse Backgrounds
Structured training programs are particularly effective in standardizing competency for practitioners from varied educational and experiential backgrounds. Novice infection preventionists may come from nursing, public health, epidemiology, or allied disciplines, each contributing unique perspectives but varying levels of exposure to clinical environments. Comprehensive onboarding, multimodal learning, mentorship, and certification preparation ensure that all participants achieve a consistent baseline of knowledge, skill, and professional judgment.
This standardization is crucial for fostering equitable opportunities within the profession. Certification serves as a unifying credential, validating competency across diverse backgrounds and reinforcing parity in career progression. By aligning training outcomes with industry standards, organizations facilitate both individual advancement and the collective strengthening of the infection prevention workforce.
Translating Training into Practical Competence
The transition from structured learning to practical competence is a pivotal stage in the development of early-career infection preventionists. While knowledge acquisition forms the foundation, the ability to operationalize concepts in diverse healthcare environments is essential for achieving both professional efficacy and Certification in Infection Control (CIC). Structured programs that integrate experiential learning, mentorship, and competency evaluation ensure that practitioners can navigate complex scenarios, interpret epidemiologic data, and implement evidence-based interventions with confidence.
Practical competence encompasses multiple dimensions. Surveillance skills are paramount, requiring practitioners to monitor infection trends, identify anomalies, and respond to potential outbreaks. Novice infection preventionists are trained to collect, analyze, and synthesize data from various clinical sources, translating numerical trends into actionable insights. This analytical foundation is complemented by the development of operational skills, including risk assessment, programmatic intervention design, and compliance evaluation. By bridging analytical acumen with practical application, structured training cultivates practitioners who are both data-literate and operationally effective.
Immersive Learning and Experiential Engagement
Immersive learning experiences are central to translating theoretical understanding into practical proficiency. Novice infection preventionists are engaged in activities such as conducting focused audits, participating in outbreak investigations, and evaluating adherence to infection control policies. These exercises offer real-time feedback, highlighting the consequences of decisions and reinforcing procedural knowledge. The experiential component of training allows practitioners to refine judgment, adapt protocols to context-specific scenarios, and develop a nuanced understanding of operational workflows across varied healthcare environments.
Exposure to multiple facility types enhances versatility and adaptability. Infection preventionists may rotate through acute care hospitals, long-term care facilities, outpatient clinics, and specialty centers, each presenting unique operational challenges and patient populations. Structured rotation programs ensure that practitioners internalize core principles while developing the flexibility to apply them in diverse settings. By standardizing foundational practices while encouraging context-sensitive adaptation, programs cultivate infection preventionists who maintain consistency in outcomes despite variability in environment and resources.
Mentorship as a Framework for Skill Development
Mentorship plays an indispensable role in reinforcing practical competence. Experienced practitioners provide guidance on the application of theoretical concepts, modeling strategic thinking, and professional comportment. Advanced mentors offer insight into the subtleties of operational decision-making, including prioritization, risk mitigation, and interdepartmental coordination. Near-peer mentors, in turn, demonstrate practical execution, offering relatable examples that facilitate comprehension and skill replication.
Mentorship is not limited to technical instruction; it also encompasses professional socialization, confidence-building, and the development of reflective practice. Novice infection preventionists learn to navigate workplace dynamics, communicate effectively with multidisciplinary teams, and integrate feedback constructively. This relational dimension of mentorship ensures that practitioners acquire both cognitive and behavioral competencies, which are critical for professional growth and long-term success.
Assessment-Driven Competency Validation
Assessment is a continuous thread woven through practical training, serving both formative and summative purposes. Formative assessments provide real-time feedback, highlighting areas for improvement and reinforcing learning. These include observation of procedural execution, evaluation of data interpretation accuracy, and review of program implementation plans. Summative assessments, often culminating in practical demonstrations or scenario-based evaluations, validate competency and readiness for certification.
Assessment-driven training ensures that novice infection preventionists achieve proficiency across multiple dimensions, including surveillance, risk management, program development, and compliance monitoring. Continuous evaluation also allows instructors to tailor learning trajectories, addressing gaps in knowledge or skills and promoting individualized professional growth. By embedding evaluation within practical experiences, programs ensure that practitioners are both competent and confident in their abilities.
Integrating Evidence-Based Practice
Early-career infection preventionists are trained to integrate evidence-based practice into operational decision-making. This involves evaluating current research, interpreting clinical guidelines, and applying validated interventions in a manner consistent with organizational policies. Practitioners are encouraged to critically appraise emerging literature, adapt protocols to the local context, and monitor outcomes to assess efficacy. Evidence-based practice training cultivates analytical rigor, ensuring that infection prevention initiatives are informed by the latest scientific understanding and are aligned with best practices in patient safety.
Integration of evidence-based strategies also reinforces the link between practical competence and certification. The CIC examination emphasizes knowledge of current guidelines, epidemiologic principles, and operational procedures, all of which are strengthened through experiential engagement and application of evidence-informed interventions. By bridging practice with theory, structured programs prepare early-career infection preventionists to meet certification requirements while enhancing operational impact.
Developing Operational Judgment
Operational judgment is a critical component of professional competence in infection prevention. Novice practitioners learn to evaluate competing priorities, allocate resources effectively, and respond to emergent situations with strategic clarity. Structured training exposes learners to scenario-based exercises, case studies, and real-time problem-solving challenges, fostering the ability to anticipate potential complications, assess risk, and implement effective mitigation strategies.
Operational judgment is closely tied to experiential learning. By engaging in simulations, outbreak investigations, and cross-facility rotations, practitioners gain exposure to complex scenarios that require adaptive reasoning. Mentorship further reinforces this skill set, with experienced mentors providing feedback, highlighting alternative approaches, and modeling decision-making processes. This combination of exposure, practice, and guided reflection ensures that early-career infection preventionists develop the cognitive agility necessary for both routine and emergent operational challenges.
Preparing for Certification Through Practice Integration
Certification preparation is seamlessly integrated into practical training to ensure alignment between learning experiences and examination expectations. Novice infection preventionists review recorded lectures, study guides, and practice exams that correspond directly to the competencies emphasized on the CIC examination. Asynchronous, self-paced learning accommodates diverse schedules while reinforcing knowledge retention and confidence.
Practice exams serve multiple purposes. They familiarize participants with the structure and format of the certification assessment, provide benchmarks for readiness, and alleviate anxiety associated with high-stakes testing. For practitioners who have delayed certification due to limited experience or perceived gaps in preparation, these resources provide targeted support, enabling incremental skill development and reinforcing practical application. By aligning experiential learning with certification objectives, structured programs ensure that practitioners are prepared to demonstrate both knowledge and competency on a standardized platform.
Addressing Variability in Practitioner Backgrounds
Structured training programs are particularly effective in standardizing competency among practitioners from heterogeneous backgrounds. Early-career infection preventionists may possess academic training in nursing, public health, microbiology, or epidemiology, yet may lack uniform exposure to operational environments. Programs that integrate practical exercises, mentorship, and assessment provide equitable pathways for achieving competence, ensuring that all participants reach the baseline proficiency required for certification and operational efficacy.
This approach also addresses systemic disparities in access to professional development. Novice infection preventionists entering the field from underrepresented backgrounds or resource-limited institutions benefit from structured, standardized training, which validates competency and supports career advancement. By providing consistent opportunities for skill acquisition and experiential learning, organizations cultivate a workforce that is both diverse and highly capable.
Mentorship and Reflective Practice
Reflective practice is a vital component of professional development in infection prevention. Novice practitioners are encouraged to evaluate their decisions, analyze outcomes, and identify opportunities for improvement. Mentors facilitate this process, guiding reflection on both successes and challenges, and modeling adaptive learning strategies. Through reflection, practitioners internalize lessons from practical experiences, enhance problem-solving capabilities, and refine operational judgment.
Mentorship complements reflective practice by providing a sounding board for discussion, clarification, and validation. The combination of reflection and mentorship fosters resilience, critical thinking, and professional maturity. Early-career infection preventionists emerge from structured programs not only competent in procedural skills but also capable of self-assessment and continuous improvement, traits that are essential for lifelong professional growth.
Translating Competence into Leadership Potential
Structured training programs cultivate the foundation for future leadership in infection prevention. By developing technical proficiency, operational judgment, and reflective skills, early-career practitioners are positioned to assume supervisory roles, lead quality improvement initiatives, and mentor subsequent cohorts. Leadership potential emerges through exposure to complex scenarios, guided decision-making, and structured opportunities for problem-solving. Certification further reinforces credibility, providing recognition of both skill and professional commitment.
Leadership development is reinforced by mentorship and experiential exposure. Advanced mentors model strategic thinking, interdepartmental collaboration, and organizational influence, demonstrating pathways for career progression. Near-peer mentors provide relatable examples of emerging leadership roles, illustrating how foundational competencies translate into supervisory responsibilities. By integrating leadership concepts into practical training, organizations ensure that the next generation of infection preventionists is prepared to guide teams, influence policy, and advance institutional safety objectives.
Continuous Professional Growth
Early-career training programs emphasize continuous professional growth beyond initial certification. Practitioners are encouraged to pursue ongoing education, engage with emerging research, and participate in professional networks. Structured mentorship and reflective practice cultivate an orientation toward lifelong learning, ensuring that infection preventionists remain adaptive, knowledgeable, and effective in dynamic healthcare environments.
Continuous growth also encompasses skill refinement in response to evolving challenges. Infection preventionists encounter novel pathogens, technological innovations, and shifting regulatory landscapes, necessitating agile learning and adaptive application of knowledge. Structured training programs, reinforced by mentorship and competency assessment, equip practitioners with the cognitive flexibility and professional discipline to navigate these changes successfully.
Mentorship Dynamics in Infection Prevention Training
Mentorship serves as a foundational pillar in the development of early-career infection preventionists, facilitating the transition from theoretical knowledge to applied expertise. Structured programs integrate layered mentorship approaches, pairing novice practitioners with advanced-practice mentors and near-peer guides to foster skill acquisition, professional socialization, and confidence building. This dual-level mentoring strategy ensures that learners receive both technical insight and practical modeling of behaviors, communication strategies, and organizational navigation essential to operational success.
Advanced mentors provide guidance in the design, implementation, and evaluation of infection prevention programs. They offer strategic perspectives on risk assessment, outbreak response, and quality improvement initiatives, helping novices interpret complex data, prioritize interventions, and make evidence-based decisions. By observing mentor-driven workflows, early-career practitioners internalize best practices, understand the rationale behind decisions, and develop analytical frameworks applicable across diverse healthcare environments.
Near-peer mentors supplement this guidance by offering relatable demonstrations of procedural skills and situational problem-solving. These mentors, who are slightly more experienced in practice, act as approachable role models, bridging the gap between novice understanding and expert proficiency. Their proximity in experience allows for candid discussions, modeling of iterative learning, and validation of competency in real-world applications. This combination of mentorship levels accelerates skill development, enhances retention, and fosters professional confidence.
Integrating Mentorship with Structured Learning
Mentorship is not an isolated component but is interwoven into the broader structure of training programs. Novice practitioners engage in experiential exercises, including surveillance data analysis, outbreak simulations, and compliance audits, with mentors providing real-time feedback. This integration ensures that theoretical knowledge is reinforced through practical application, while mentorship facilitates reflection on performance, promotes critical thinking, and instills adaptive decision-making capabilities.
Structured feedback loops between mentors and mentees are crucial. Regular evaluation sessions allow mentors to assess progress, identify knowledge gaps, and guide learners through corrective strategies. Reflection exercises, encouraged by mentors, reinforce learning by prompting practitioners to analyze outcomes, consider alternative approaches, and internalize lessons for future application. The synergy between mentorship and structured learning ensures that competency development is comprehensive, iterative, and aligned with professional standards.
Certification as a Measure of Mentorship Success
Certification functions as a tangible outcome reflecting the efficacy of mentorship and structured training. Achieving Certification in Infection Control (CIC) validates not only knowledge acquisition but also the ability to apply skills effectively in diverse operational contexts. Programs that integrate mentorship into their preparation processes have consistently demonstrated high pass rates, underscoring the role of guided support in achieving competency benchmarks.
For novice infection preventionists, mentorship enhances preparedness by clarifying complex concepts, modeling professional behaviors, and reinforcing critical decision-making processes. The combination of hands-on experience, reflective practice, and mentor guidance equips practitioners with the skills required to succeed in high-stakes certification assessments. Consequently, mentorship functions as both a developmental tool and a strategic mechanism to ensure measurable professional achievement.
Long-Term Professional Development
Structured mentorship extends beyond initial training and certification, laying the groundwork for long-term professional growth. Early-career infection preventionists cultivate analytical thinking, operational judgment, and reflective practices that serve as the foundation for continuous learning. Mentors guide practitioners in identifying career goals, pursuing advanced educational opportunities, and exploring leadership trajectories within infection prevention programs.
Reflective practice, reinforced by mentorship, is central to sustaining professional growth. Practitioners learn to evaluate their decision-making, assess the impact of interventions, and identify opportunities for improvement. This iterative process encourages adaptive learning, allowing infection preventionists to respond effectively to evolving challenges, including emerging pathogens, novel regulatory requirements, and technological advancements in surveillance and program management.
Expanding Professional Capacity Through Mentorship
Mentorship programs contribute to workforce capacity and resilience. By developing confident, competent practitioners, organizations enhance their ability to maintain consistent, high-quality infection prevention programs. Mentorship also prepares practitioners to assume supervisory or leadership roles, creating a cycle of knowledge transfer and skill propagation within the organization. Experienced infection preventionists, having benefited from structured mentoring, are better equipped to guide the next generation, reinforcing organizational standards and sustaining operational excellence.
This cascading model of mentorship ensures the long-term sustainability of the infection prevention workforce. As early-career practitioners advance into leadership positions, they replicate and adapt mentorship strategies, embedding a culture of continuous development and professional support. Organizations benefit from both immediate skill enhancement and the cultivation of a resilient, self-perpetuating professional ecosystem.
Structured Learning and Competency Verification
In conjunction with mentorship, competency verification is essential for validating skill acquisition. Structured programs employ multiple assessment modalities, including practical demonstrations, scenario-based exercises, quizzes, and formal evaluations. These assessments measure proficiency across operational domains, including surveillance, outbreak investigation, risk mitigation, and compliance adherence. Verification ensures that novice infection preventionists not only acquire theoretical knowledge but can also apply it effectively within clinical and organizational contexts.
Regular competency evaluation provides opportunities for corrective guidance and individualized development. Mentors play a central role in this process, observing performance, offering feedback, and facilitating targeted learning interventions. By continuously monitoring progress and addressing gaps, structured programs maintain rigorous standards and reinforce the alignment between practical skill, mentorship guidance, and certification readiness.
Integrating Evidence-Based Practice in Professional Development
Evidence-based practice is a cornerstone of effective infection prevention and a central focus of mentorship and structured training. Practitioners are encouraged to critically appraise emerging research, interpret clinical guidelines, and apply validated interventions within their operational environments. Mentors guide the integration of evidence into daily practice, fostering analytical rigor and reinforcing adherence to industry standards.
Practitioners who engage with evidence-based approaches develop the capacity to evaluate intervention effectiveness, adapt strategies to local context, and contribute to institutional quality improvement initiatives. This emphasis on research literacy, combined with practical mentorship, ensures that early-career infection preventionists are prepared to navigate evolving healthcare landscapes, address novel challenges, and implement interventions with measurable impact.
Supporting Diverse Professional Pathways
Mentorship and structured training programs recognize the value of diversity in the infection prevention workforce. Practitioners may enter the field from nursing, public health, microbiology, epidemiology, or other allied disciplines, each bringing unique perspectives and experiences. Structured mentorship provides tailored guidance to bridge gaps in operational exposure, ensuring equitable competency development across heterogeneous professional backgrounds.
By supporting diverse entry pathways, organizations foster inclusive professional environments that enhance problem-solving capacity, creativity, and innovation in infection prevention strategies. Certification serves as a unifying measure of competence, validating skills acquired through varied professional journeys and reinforcing opportunities for career advancement.
Continuous Feedback and Iterative Improvement
Feedback is a central component of mentorship-driven training. Mentors provide ongoing evaluation of performance, guiding practitioners through complex tasks, suggesting refinements, and reinforcing successful practices. This iterative feedback loop encourages continuous improvement, promotes self-reflection, and enhances adaptability.
Regularly scheduled feedback sessions also facilitate the early identification of knowledge gaps or skill deficiencies, allowing for targeted interventions. Mentors support the implementation of corrective strategies, monitor progress, and adjust learning trajectories to ensure that practitioners meet both operational and certification standards. Continuous feedback reinforces learning, fosters accountability, and contributes to long-term professional competence.
Professional Confidence and Workforce Resilience
Mentorship cultivates professional confidence, which is critical for early-career infection preventionists facing complex clinical and operational challenges. Practitioners develop assurance in their analytical, procedural, and decision-making abilities through guided practice, feedback, and repeated application. Confidence enhances performance, encourages proactive engagement in problem-solving, and supports the cultivation of professional autonomy.
Workforce resilience is also strengthened through mentorship. By providing guidance, modeling adaptive strategies, and supporting reflective practice, mentors equip practitioners to navigate stress, ambiguity, and high-stakes decision-making. Resilient infection preventionists are better prepared to sustain consistent quality in their work, maintain adherence to protocols under pressure, and contribute positively to institutional safety culture.
Building a Collaborative Professional Culture
Mentorship fosters a culture of collaboration and continuous learning within infection prevention teams. Experienced practitioners model effective communication, interdisciplinary coordination, and evidence-based decision-making, setting standards for professional conduct. Novice practitioners, in turn, contribute fresh perspectives, engage in reflective discussions, and support peer learning.
This collaborative culture strengthens organizational capacity by promoting shared accountability, knowledge exchange, and coordinated intervention strategies. The integration of mentorship into training programs ensures that infection preventionists operate as cohesive units, capable of responding efficiently to emergent challenges and sustaining programmatic excellence across multiple care settings.
Certification Outcomes and Workforce Competency
Certification in infection control serves as a tangible benchmark for the competency and readiness of early-career infection preventionists. The structured integration of mentorship, experiential learning, and targeted preparation ensures that practitioners are well-positioned to meet the rigorous standards assessed by the Certification in Infection Control (CIC) examination. High first-attempt pass rates among participants underscore the effectiveness of comprehensive training programs, reflecting the synergy between knowledge acquisition, practical application, and structured guidance.
Certification outcomes are indicative not only of individual proficiency but also of organizational commitment to workforce development. Practitioners who successfully attain certification demonstrate mastery of epidemiologic principles, outbreak response strategies, and program management protocols, all essential for sustaining safe and effective healthcare environments. The credential serves as a validation of both theoretical understanding and operational execution, providing a measure of assurance to supervisors, interdisciplinary teams, and patients alike.
Expanding Structured Training Beyond Organizational Boundaries
Structured infection prevention training programs have proven effective not only within a single organization but also when extended to external participants. Early-career practitioners from diverse healthcare facilities benefit from exposure to standardized learning frameworks, evidence-based protocols, and mentorship strategies. Expanding training to external participants enhances professional networks, promotes consistency in practice, and strengthens workforce competency across institutional and geographic boundaries.
Training expansion includes modular onboarding, mentorship pairing, experiential exercises, and certification preparation. Novice practitioners from other organizations gain access to structured guidance, hands-on learning opportunities, and assessment feedback, leveling the professional development landscape for individuals who may otherwise encounter limited resources or support. This dissemination of best practices fosters a collaborative professional environment and contributes to the broader advancement of infection prevention standards.
Longitudinal Program Evaluation
The evaluation of long-term outcomes is critical for assessing the impact of structured training programs on workforce competency and certification success. Longitudinal studies track participant progress, certification achievement, and professional retention over multiple years, providing a comprehensive view of program efficacy. Metrics such as CIC first-attempt pass rates, demonstrated operational competence, and continued engagement in infection prevention roles offer objective indicators of both individual and organizational benefit.
Regular program evaluation enables continuous refinement of curricula, training methodologies, and mentorship approaches. Feedback loops incorporating participant experiences, mentor observations, and assessment outcomes facilitate targeted improvements, ensuring that training remains responsive to evolving professional requirements and healthcare challenges. This iterative approach strengthens the alignment between training objectives, certification benchmarks, and real-world operational needs.
Supporting Early-Career Infection Preventionists
Structured programs are particularly valuable for early-career practitioners entering the field from diverse educational or professional backgrounds. Novices often possess advanced academic knowledge but limited exposure to direct clinical practice, necessitating intentional support to develop applied competencies. Training frameworks integrate experiential engagement, multi-modal learning, and mentorship to bridge the gap between theory and practice, enabling early-career infection preventionists to acquire essential skills, confidence, and professional acumen.
Mentorship supports individualized development by tailoring guidance to the unique needs and prior experiences of each practitioner. Advanced mentors provide strategic oversight, modeling programmatic thinking and operational execution, while near-peer mentors facilitate skill demonstration, problem-solving, and contextual adaptation. This layered support system ensures equitable access to professional development opportunities and reinforces competency across a heterogeneous workforce.
Certification Preparation and Exam Readiness
The alignment of training programs with CIC examination objectives is central to practitioner success. Asynchronous learning modules, recorded lectures, study guides, and practice examinations provide targeted preparation for the content and format of the certification assessment. Practice exams simulate real-world testing conditions, mitigating anxiety and enabling practitioners to identify areas requiring additional focus.
Certification readiness is further enhanced by integrating experiential learning with theoretical review. Hands-on engagement in surveillance, outbreak management, and compliance monitoring reinforces knowledge retention while providing context for exam content. Mentorship ensures that practitioners can apply knowledge critically and accurately, strengthening both operational competence and examination performance.
Building Professional Confidence
Professional confidence emerges as a key outcome of structured training programs. Early-career infection preventionists gain assurance in their ability to interpret data, implement interventions, and navigate organizational workflows. Confidence is reinforced through repeated application of skills, feedback from mentors, and successful engagement in complex scenarios. Practitioners who possess both competence and confidence are more likely to take initiative, engage collaboratively, and contribute meaningfully to infection prevention initiatives within their organizations.
Confidence also supports certification success. Practitioners who approach the CIC examination with self-assurance and familiarity with applied concepts are more likely to achieve first-attempt success, further validating the effectiveness of structured training and mentorship frameworks.
Workforce Retention and Career Advancement
Structured training and certification preparation contribute to workforce retention by fostering engagement, professional identity, and career trajectory development. Early-career practitioners who receive comprehensive support are more likely to remain in the field, advance into leadership positions, and participate in mentoring subsequent cohorts. Retention of trained infection preventionists ensures continuity in programmatic quality, institutional knowledge, and patient safety initiatives.
Career advancement is facilitated by both competency validation and certification recognition. CIC-certified practitioners gain credibility, enhanced visibility within organizations, and access to leadership opportunities. Structured training programs that integrate mentorship and certification preparation support this trajectory, creating pathways for early-career practitioners to evolve into influential contributors to infection prevention practice and policy.
Enhancing Organizational Capacity
The presence of certified, competent infection preventionists enhances organizational capacity to deliver safe, evidence-based care. Structured training programs cultivate practitioners who are adept in surveillance, risk assessment, outbreak response, and program management, ensuring that institutional infection prevention initiatives are consistent, effective, and adaptive. Organizations benefit from a workforce that can implement standardized protocols, address emergent challenges, and provide mentorship to less-experienced staff.
High-functioning infection prevention teams also contribute to regulatory compliance, quality improvement, and patient safety outcomes. The integration of structured training, mentorship, and certification ensures that practitioners are equipped to meet both internal organizational goals and external standards, reinforcing operational excellence and institutional resilience.
Mentorship as a Long-Term Investment
Mentorship within structured programs represents a long-term investment in both individual practitioners and organizational outcomes. Experienced mentors cultivate skill, confidence, and professional judgment in early-career infection preventionists while reinforcing a culture of continuous learning. As mentees progress into leadership roles, they perpetuate this cycle by mentoring subsequent practitioners, ensuring knowledge transfer, and sustaining organizational expertise.
The cumulative effect of mentorship over time enhances workforce sustainability. Organizations with layered mentorship structures develop resilient teams capable of adapting to emerging challenges, maintaining program quality, and fostering collaborative professional environments. Mentorship extends beyond immediate training outcomes, embedding professional standards and culture into the fabric of organizational practice.
Expanding Professional Networks
Participation in structured training programs fosters the development of professional networks, connecting early-career infection preventionists with mentors, peers, and practitioners from diverse organizations. These networks facilitate knowledge exchange, collaborative problem-solving, and the dissemination of best practices. Networking also supports career development, offering insights into emerging trends, opportunities for professional growth, and access to continuing education resources.
Robust professional networks contribute to workforce resilience by enabling rapid dissemination of information, coordinated responses to emerging threats, and peer support during complex operational scenarios. Structured training programs that integrate networking opportunities amplify the impact of mentorship and experiential learning, enhancing both individual and organizational capacity.
Measuring Program Impact
Program impact is measured through multiple dimensions, including certification achievement, competency validation, professional retention, and operational outcomes. High CIC pass rates reflect successful knowledge integration, practical application, and effective mentorship. Competency assessments, performance evaluations, and feedback loops provide additional metrics to gauge skill acquisition and professional development.
Longitudinal tracking of program participants enables organizations to evaluate sustained performance, career progression, and contributions to infection prevention initiatives. Continuous assessment informs program refinement, curriculum adaptation, and mentorship strategies, ensuring that training remains responsive to evolving healthcare landscapes and professional needs.
Sustaining Excellence in Infection Prevention
Structured training programs, mentorship, and certification preparation collectively sustain excellence in infection prevention practice. Early-career practitioners acquire the knowledge, skills, and professional confidence necessary to implement evidence-based interventions, navigate complex clinical environments, and contribute meaningfully to patient safety. Organizations benefit from a resilient, competent workforce capable of maintaining high standards of care and responding adaptively to emerging challenges.
Sustained excellence is reinforced through iterative program evaluation, continuous professional development, and mentorship cycles. Practitioners remain engaged, informed, and proficient, while organizations maintain operational readiness, program consistency, and regulatory compliance. The integration of these elements ensures that infection prevention practice evolves in parallel with the demands of modern healthcare systems.
Conclusion
Infection prevention is a dynamic and critical discipline within healthcare, requiring a workforce that is both knowledgeable and operationally competent. Structured training programs, combined with layered mentorship and targeted certification preparation, provide early-career infection preventionists with the tools to bridge theoretical knowledge and practical application. These programs cultivate analytical skills, operational judgment, and evidence-based decision-making, while fostering professional confidence and resilience. Certification in infection control serves as a tangible benchmark of competency, validating expertise and supporting career advancement. By expanding training beyond organizational boundaries, integrating reflective practice, and emphasizing experiential learning, these programs strengthen workforce capacity, standardize practices across diverse settings, and enhance patient safety. Long-term investment in mentorship and professional development ensures sustainability, creating a cycle of continuous learning, leadership cultivation, and knowledge transfer. Ultimately, this comprehensive approach prepares infection preventionists to meet evolving healthcare challenges with skill, confidence, and strategic acumen.