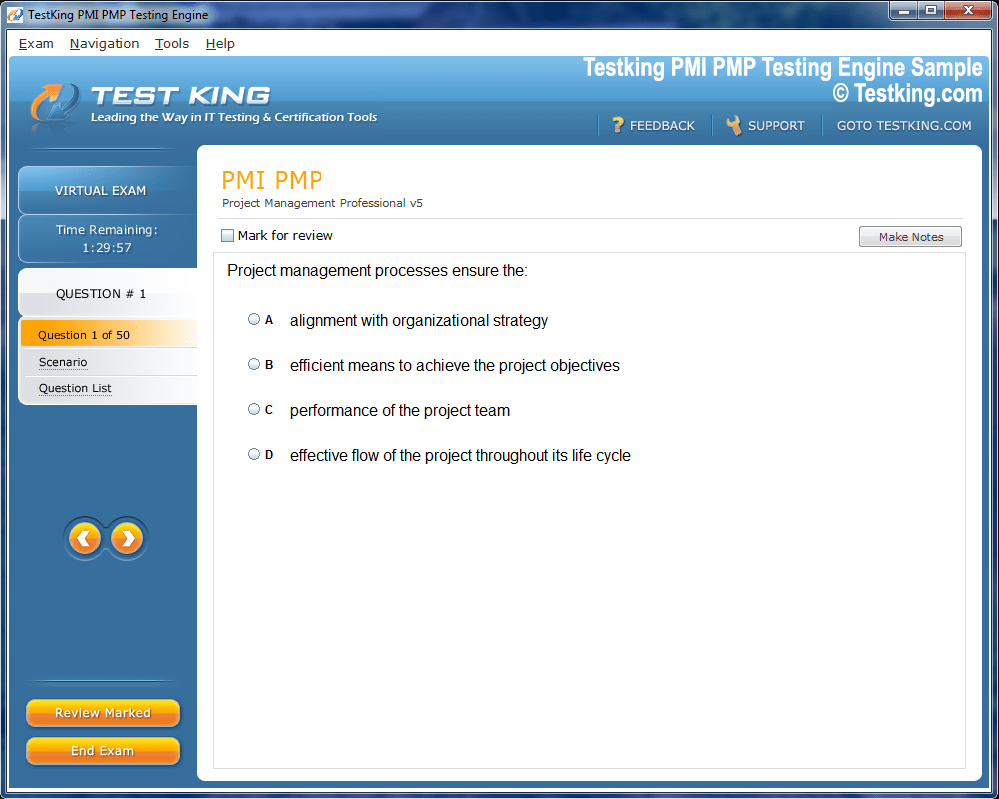
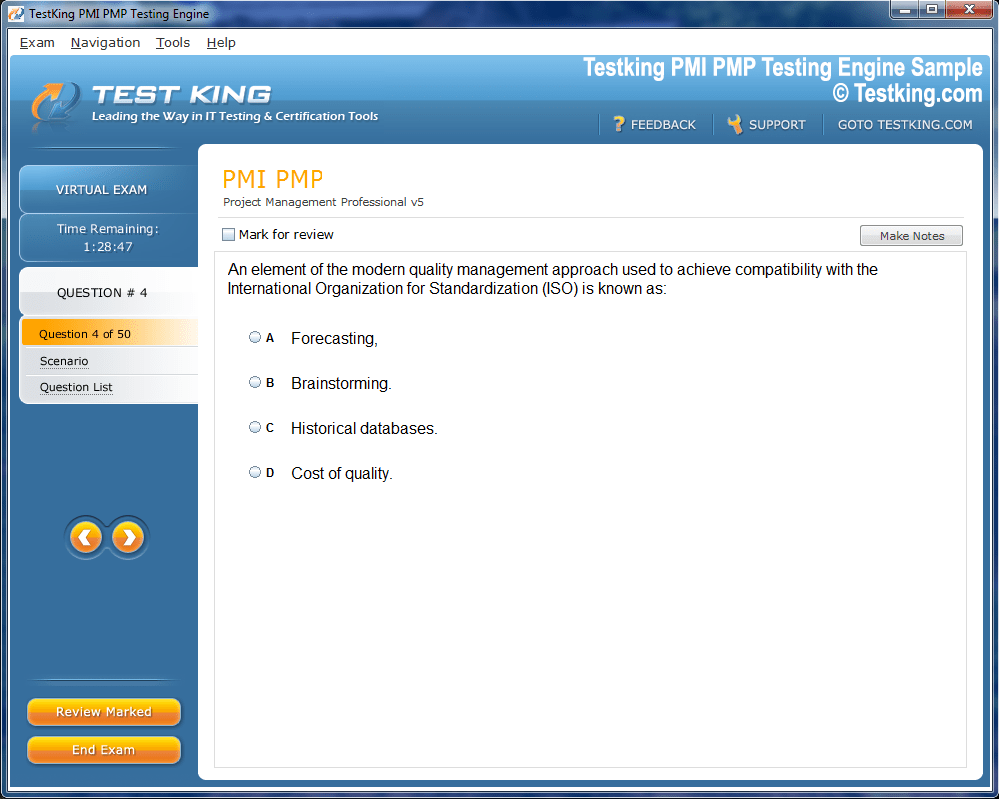
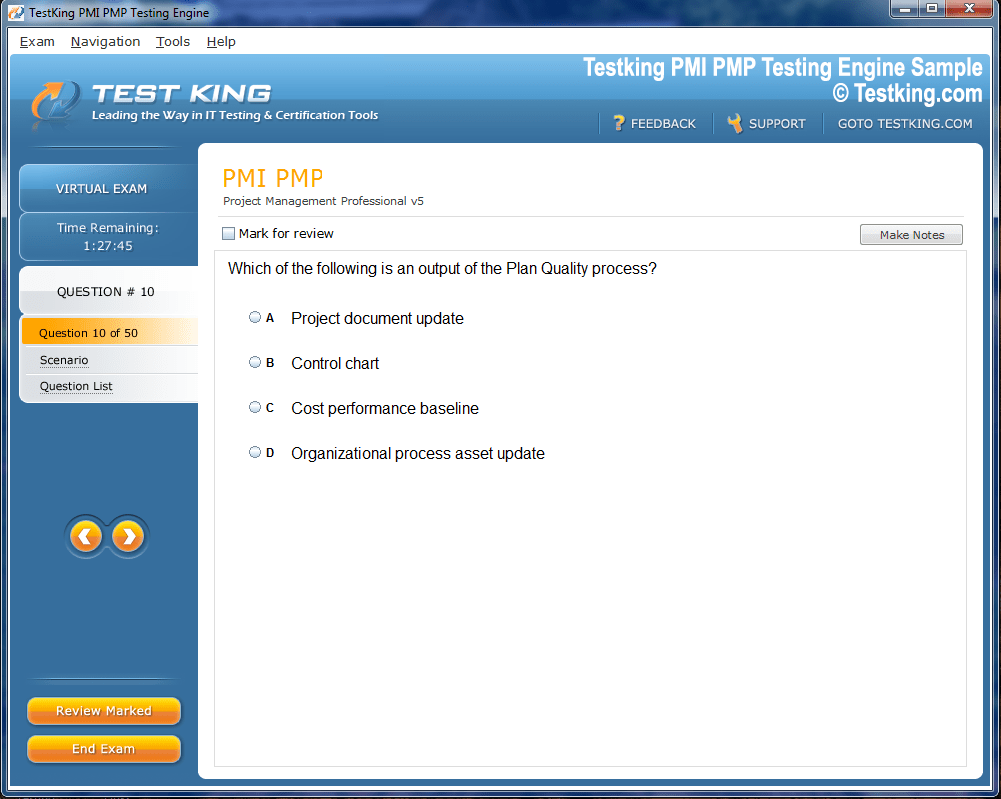
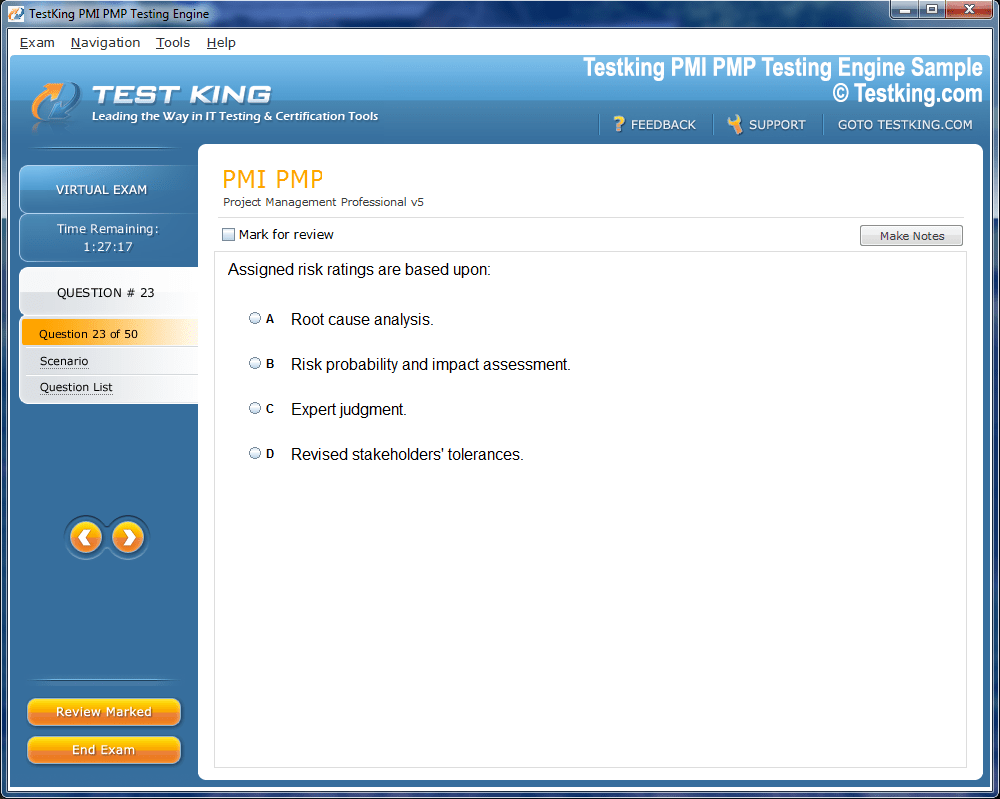
Product Screenshots
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our AHM-510 testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.
Top AHIP Exams
Comprehensive Guide to AHIP AHM-510 Exam Preparation
The AHIP AHM-510 Exam is one of the most reputable and rigorous assessments in the healthcare insurance field, designed to evaluate an individual’s deep understanding of Medicare’s intricate structure and the multifaceted regulations that govern it. For professionals seeking to strengthen their expertise, mastering this exam represents both an intellectual and professional milestone. It reflects a commitment to excellence and compliance within an ever-evolving healthcare system where precision, comprehension, and ethical practice are paramount.
The healthcare landscape is constantly transforming, driven by policy reforms, demographic changes, and technological advancements. Within this dynamic environment, Medicare remains a foundational component of the American healthcare system, serving millions of beneficiaries across the nation. The AHM-510 Exam, created and administered by America’s Health Insurance Plans (AHIP), focuses on cultivating an advanced level of proficiency among individuals who work directly or indirectly with Medicare policies and programs. This exam is not merely a test of memory or rote learning; it measures how well candidates can interpret complex regulations, evaluate compliance requirements, and apply theoretical knowledge to real-world healthcare scenarios.
The Nature and Structure of the Exam
To approach the AHM-510 Exam effectively, it is crucial to understand its structural design. This examination employs a multiple-choice format that typically consists of 60 to 70 carefully curated questions. These questions are methodically constructed to cover a wide spectrum of subjects within Medicare administration, policy analysis, and compliance management. The duration of the test is two hours, providing candidates with sufficient time to read, analyze, and respond thoughtfully to each question.
A passing score of 70% signifies that the participant has achieved a competent grasp of the essential subject matter. While the number might appear moderate, the difficulty lies in the breadth and depth of the content. Medicare, as a federal health insurance program, is regulated by an extensive set of statutes, guidelines, and procedural mandates, which candidates must understand in both conceptual and applied contexts.
The examination’s complexity ensures that those who succeed are genuinely prepared to handle professional responsibilities in Medicare-related roles. Whether in policy compliance, claims administration, managed care operations, or consulting, individuals with this certification demonstrate the analytical capabilities and judgment necessary for decision-making within healthcare systems.
The Significance of AHIP and Its Educational Mission
America’s Health Insurance Plans (AHIP) serves as an influential voice within the U.S. healthcare industry. Its mission centers on promoting affordable, equitable, and sustainable health coverage while ensuring that industry professionals uphold the highest standards of knowledge and competence. Through its certification programs, including the AHM-510, AHIP empowers healthcare administrators, insurers, and policymakers to navigate the intricacies of government programs with confidence and precision.
The AHM-510 Exam stands as a testament to AHIP’s commitment to professional development and educational excellence. By setting a consistent benchmark of proficiency, AHIP helps ensure that individuals responsible for managing Medicare-related operations possess a thorough understanding of compliance obligations, ethical standards, and strategic implementation of federal guidelines.
The certification not only enhances credibility but also instills a sense of responsibility. Those who earn this credential become part of a community that influences public health outcomes and ensures that Medicare beneficiaries receive the protection and quality service they deserve.
Key Areas of Focus within the Exam
The AHM-510 Exam explores a variety of advanced topics that extend beyond basic Medicare literacy. Candidates are expected to understand the history, structure, and operational framework of the Medicare program, along with the legal and ethical dimensions of its administration. Major areas include Medicare Parts A, B, C, and D, each with its distinct coverage parameters and eligibility requirements.
Medicare Part A deals with hospital insurance, encompassing inpatient hospital care, skilled nursing facility services, hospice care, and certain home healthcare services. Part B covers medical insurance for outpatient services, preventive care, and durable medical equipment. Part C, also known as Medicare Advantage, allows beneficiaries to receive Medicare benefits through private health plans approved by Medicare. Part D provides prescription drug coverage, a critical component for millions of beneficiaries managing chronic conditions.
Beyond these foundational aspects, the AHM-510 Exam also delves into the nuanced territory of Medicare compliance. This includes understanding the regulations established by the Centers for Medicare & Medicaid Services (CMS), the protocols for reporting and documentation, and the ethical considerations that govern healthcare practices. Candidates must be familiar with the mechanisms of fraud prevention, auditing, and the maintenance of transparency within organizational operations.
The exam’s emphasis on compliance underscores the gravity of accuracy and accountability in healthcare management. Inaccurate reporting or a lapse in regulatory adherence can lead to significant legal repercussions and financial penalties. Therefore, professionals who pass the AHM-510 demonstrate not only intellectual mastery but also an ethical commitment to the integrity of the healthcare system.
The Role of Policy Knowledge and Analytical Skill
Passing the AHM-510 Exam requires more than memorizing statutes or understanding administrative terms. It demands the ability to analyze, interpret, and synthesize information from multiple sources. Healthcare professionals must evaluate policy implications, anticipate the impact of regulatory changes, and apply conceptual frameworks to practical decision-making.
For instance, a question may require candidates to identify the correct response not through recall alone but through reasoning that incorporates Medicare policy principles and compliance logic. This analytical orientation mirrors the daily responsibilities of healthcare managers who must interpret policy updates, assess operational risks, and ensure alignment between organizational objectives and legal requirements.
Policy literacy, therefore, becomes a vital component of exam preparation. Candidates benefit from studying legislative histories, such as the Social Security Amendments of 1965, which established Medicare, and subsequent reforms like the Balanced Budget Act and the Medicare Prescription Drug, Improvement, and Modernization Act. Understanding these foundational shifts allows candidates to contextualize current Medicare operations within a broader historical and legislative framework.
Analytical skills are further tested through scenario-based questions, which simulate real-world challenges. These situations often involve ethical dilemmas, resource allocation decisions, or interpretations of regulatory guidance. The ability to think critically and respond with clarity is essential for success.
Developing an Effective Study Approach
Preparation for the AHM-510 Exam should begin with an organized and methodical study plan. Candidates must first obtain the official exam blueprint from AHIP, which outlines all the competencies and objectives covered in the test. Reviewing this document provides a roadmap for targeted learning, ensuring that study efforts are distributed evenly across the relevant domains.
A structured study schedule helps maintain consistency. Allocating specific time blocks to each major topic—such as Medicare structure, compliance, policy interpretation, and ethical considerations—enables gradual mastery without overwhelming the learner. Setting achievable milestones enhances motivation and allows for progress tracking.
Incorporating official AHIP study materials into one’s preparation is highly advisable. These resources, developed by subject matter experts, align closely with the exam’s objectives. Textbooks, online learning modules, and practice assessments collectively provide a comprehensive understanding of both theory and application.
Practice exams are particularly valuable tools. They not only familiarize candidates with the exam format but also build mental endurance for the two-hour test duration. By reviewing incorrect answers and revisiting the related material, candidates can identify patterns of misunderstanding and refine their approach.
Another powerful method involves collaborative learning. Engaging with study groups or discussion forums allows participants to share insights and clarify complex topics. The diversity of perspectives can illuminate nuances that might otherwise be overlooked. Interaction with peers also fosters accountability, helping maintain momentum throughout the preparation journey.
The Psychological Dimension of Exam Readiness
Mental and emotional preparation plays an equally significant role in achieving success. Exam anxiety can hinder concentration and memory retention, even for well-prepared candidates. Developing a calm and confident mindset is therefore essential.
Techniques such as mindfulness meditation, deep breathing, and visualization can mitigate pre-exam stress. Establishing a regular routine that balances study with rest and recreation prevents burnout and sustains cognitive performance.
Adequate sleep is especially vital, as it enhances focus, problem-solving capacity, and recall. Nutritional balance also contributes to cognitive stability. Foods rich in omega-3 fatty acids, antioxidants, and proteins support brain health and sustained concentration.
On exam day, candidates should ensure they are physically and mentally prepared. Arriving early allows time to acclimate to the environment, reducing last-minute tension. Reading questions carefully, managing time judiciously, and maintaining steady composure throughout the test are key behavioral elements that contribute to success.
The Broader Impact of the AHM-510 Credential
Achieving certification through the AHM-510 Exam carries implications beyond personal accomplishment. It enhances professional credibility and signals a high level of competence to employers, colleagues, and stakeholders within the healthcare sector.
Individuals who earn this credential become more adept at navigating the regulatory frameworks that influence healthcare financing and delivery. Their expertise contributes to the integrity and efficiency of organizational operations. By ensuring compliance with Medicare guidelines, they help prevent violations and safeguard the financial and ethical health of their institutions.
Moreover, certified professionals often serve as mentors or policy advisors, guiding teams through complex administrative processes and promoting best practices in Medicare management. Their insight can influence strategic planning, auditing procedures, and quality improvement initiatives.
From a career perspective, this credential opens pathways to higher-level roles, including compliance officer, healthcare consultant, and policy analyst. In an era where healthcare accountability is closely scrutinized, organizations increasingly value individuals who demonstrate both regulatory proficiency and principled judgment.
Sustaining Knowledge and Professional Growth
Certification is not the endpoint of learning but rather a foundation for continual development. The healthcare field evolves rapidly, with frequent legislative modifications and technological innovations influencing how Medicare programs are administered. Staying informed about these changes is a professional responsibility.
Reading regulatory updates, attending training sessions, and participating in industry conferences help maintain relevance and deepen expertise. Continuous learning ensures that certified professionals remain equipped to adapt to shifts in policy, technology, and public health priorities.
Professional growth also involves reflection and application. By examining case studies, reviewing performance outcomes, and engaging in peer discussions, individuals can integrate theoretical insights with practical experience. This iterative process reinforces understanding and enhances problem-solving capabilities.
Building a Strong Foundation for the AHIP AHM-510 Exam
Preparing for the AHIP AHM-510 Exam requires a deliberate, structured approach that combines theoretical understanding with practical application. The exam assesses proficiency in Medicare regulations, compliance, and advanced policy comprehension—subjects that demand a disciplined study regimen and intellectual persistence. Establishing a solid foundation ensures not only that candidates can navigate the complexities of the material but also that they cultivate a durable grasp of the principles that underpin Medicare’s operation and governance.
The AHM-510 Exam tests a candidate’s capacity to synthesize diverse concepts, from eligibility rules and benefit structures to policy frameworks and ethical considerations. Building that knowledge base involves more than just reading—it requires deep immersion, analytical thinking, and consistent reinforcement. Success in this exam is as much about the mindset as it is about the material, reflecting a candidate’s ability to think critically about healthcare delivery systems and the administrative mechanisms that sustain them.
Structuring a Comprehensive Study Plan
A well-crafted study plan is the cornerstone of effective preparation. Without structure, even the most motivated candidate may find themselves overwhelmed by the breadth of topics covered in the AHM-510 Exam. A systematic plan brings order to complexity, ensuring that every essential subject receives adequate attention.
The first step in creating such a plan is to outline the key topics using the official AHIP exam blueprint. This document provides the framework upon which to build the entire preparation strategy. By identifying the core competencies, candidates can allocate time proportionally to each domain, focusing on weaker areas without neglecting foundational ones.
Daily and weekly study goals should be realistic, measurable, and adaptable. For instance, dedicating specific hours to Medicare structure during one week and shifting to compliance and policy analysis the next allows for gradual, cumulative learning. Consistency is critical; studying in shorter, focused intervals often yields better retention than infrequent, prolonged sessions.
Incorporating scheduled review periods throughout the study plan is essential. Revisiting previously covered material consolidates memory and strengthens comprehension. Regular self-assessment through quizzes or mock tests ensures continuous feedback, helping learners recognize gaps and adjust their strategy accordingly.
A well-balanced plan also considers the cognitive rhythm of the individual. Some people absorb information more efficiently in the morning, while others prefer late-night study sessions. Understanding one’s natural learning patterns helps optimize efficiency and retention.
Mastering the Medicare Framework
The AHM-510 Exam requires a thorough understanding of Medicare’s organizational structure and its interlocking components. Medicare is not a monolithic system but a complex amalgamation of parts designed to serve different healthcare needs for eligible individuals.
Part A, known as Hospital Insurance, primarily covers inpatient hospital care, skilled nursing facility services, hospice care, and limited home health services. It is typically funded through payroll taxes, and most beneficiaries qualify for premium-free coverage after sufficient work history.
Part B, or Medical Insurance, focuses on outpatient care, physician services, preventive screenings, and certain types of medical equipment. Unlike Part A, this component generally requires a monthly premium. Understanding the nuances of coverage, exclusions, and billing processes for Part B is crucial for those managing claims or compliance.
Part C, commonly referred to as Medicare Advantage, integrates Parts A and B and often includes prescription drug coverage. Administered through private health plans approved by Medicare, Part C offers flexibility but requires adherence to federal standards. Candidates must grasp how these private entities interact with the federal framework and the regulatory obligations that govern them.
Part D, introduced through the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, provides beneficiaries with prescription drug coverage. It operates through private plans that contract with Medicare, and understanding the subsidy structure, formulary rules, and cost-sharing requirements is vital for exam success.
The Importance of Policy Interpretation
Policy interpretation lies at the heart of Medicare administration. The AHM-510 Exam evaluates not just factual recall but the ability to interpret and apply policy in real-world contexts. This skill is critical because healthcare laws and guidelines often require nuanced understanding to implement effectively.
Medicare policies evolve through legislative action, regulatory updates, and administrative interpretations by federal agencies. Candidates should familiarize themselves with how these processes occur and how to interpret the implications of policy changes. A deep understanding of legislative intent—why a policy was created or amended—enables more accurate decision-making in professional practice.
For example, understanding the reasoning behind changes in reimbursement structures or eligibility criteria helps professionals anticipate operational impacts and adjust processes accordingly. Interpreting policy also involves identifying potential conflicts, ethical considerations, and compliance risks. This interpretive skill distinguishes those who simply know the rules from those who can apply them strategically.
Studying historical policy shifts can also strengthen comprehension. The establishment of Medicare in 1965 under the Social Security Amendments, the subsequent expansion of benefits, and the introduction of Medicare Advantage and Part D all illustrate how evolving social and economic needs shape public health programs. Recognizing these transformations helps candidates contextualize current regulations and anticipate future reforms.
Utilizing Official Study Materials
AHIP’s official study materials are indispensable tools for anyone preparing for the AHM-510 Exam. These resources, developed by experts and regularly updated to reflect current regulations, ensure alignment with the exam’s content structure. Textbooks, digital learning platforms, and interactive modules offer comprehensive coverage of key topics and allow candidates to engage with the material at multiple levels of depth.
Using these materials effectively requires active learning strategies. Passive reading rarely leads to mastery; instead, candidates should summarize concepts in their own words, create outlines, and apply the information through case studies or hypothetical scenarios. By transforming theoretical knowledge into applied understanding, candidates enhance their ability to recall and utilize information under exam conditions.
Practice assessments provided by AHIP serve a dual purpose. They familiarize candidates with the exam format and help measure readiness. After completing each practice test, reviewing incorrect responses is essential. Rather than memorizing the right answer, the goal should be to understand the underlying reasoning. This reflective process strengthens analytical thinking and reduces the likelihood of similar errors in the actual exam.
Supplementing official materials with credible academic texts or peer-reviewed articles can further deepen comprehension. However, it is crucial that any supplementary reading aligns with the current Medicare framework and does not introduce outdated or conflicting information.
Leveraging Collaborative Learning
Collaboration can greatly enhance exam preparation. Engaging with peers in study groups or online forums fosters intellectual exchange and mutual motivation. Discussing challenging topics helps clarify misconceptions, and teaching others reinforces one’s own understanding.
In a study group, members can divide topics, conduct research, and present summaries to the group, thereby covering more material efficiently. Constructive debate over policy interpretation encourages critical thinking, while hearing alternative perspectives broadens conceptual understanding.
Digital platforms have made collaborative learning more accessible than ever. Candidates can participate in virtual study sessions, share notes, and discuss exam-related insights in professional forums. This digital interaction builds a sense of community and accountability, both of which can sustain motivation throughout the preparation process.
However, collaboration must remain focused and disciplined. Discussions should be centered on verified content and relevant exam objectives. Engaging in speculative conversations or relying on unverified resources can lead to confusion or misinformation. Setting clear goals and maintaining structure within the group ensures productive collaboration.
Developing Critical Thinking and Application Skills
The AHM-510 Exam rewards analytical reasoning over rote memorization. Many questions present complex scenarios that require synthesis of information from multiple domains. Developing critical thinking skills is therefore essential for success.
Candidates should practice analyzing case-based questions where multiple regulations may apply simultaneously. For instance, a scenario might involve assessing eligibility under specific Medicare Parts, identifying compliance obligations, or resolving a coverage dispute. Approaching such questions methodically—by isolating relevant variables and applying the appropriate regulatory framework—enhances accuracy.
Engaging in reflective exercises can further sharpen reasoning abilities. After studying a policy or regulation, candidates should ask themselves how it applies in different contexts or how a change in one parameter might alter the outcome. This habit transforms abstract knowledge into flexible, applicable insight.
Time management during the exam also benefits from analytical discipline. Some questions may appear deceptively simple but contain subtle distinctions that require careful evaluation. Developing the ability to discern key details quickly can prevent misinterpretation and improve overall performance.
Maintaining Focus and Motivation
Long-term exam preparation can be mentally demanding. Maintaining focus requires a blend of discipline, balance, and intrinsic motivation. Setting specific goals—such as mastering one section of Medicare policy each week—helps sustain momentum.
Creating a study environment conducive to concentration is equally important. Minimizing distractions, maintaining an organized workspace, and adhering to a consistent routine foster mental clarity. Some individuals benefit from environmental cues such as background instrumental music or study-specific scents, which help trigger concentration through associative memory.
Motivation can wane over time, especially when facing dense or complex material. To counter this, candidates should periodically reflect on their purpose for pursuing the AHM-510 certification. Recognizing the professional opportunities and personal growth that accompany mastery can rekindle determination.
Balancing study with relaxation prevents burnout. Short breaks, exercise, and leisure activities rejuvenate the mind and improve long-term productivity. Developing resilience—the ability to persist despite difficulty—is perhaps the most valuable mental asset in preparing for this exam.
Integrating Ethical Awareness into Preparation
Understanding the ethical dimensions of Medicare administration is a vital part of preparation for the AHM-510 Exam. Ethical practice ensures that decisions made within healthcare organizations uphold fairness, transparency, and respect for patient rights.
Candidates should study ethical principles such as beneficence, nonmaleficence, autonomy, and justice as they relate to Medicare operations. These principles guide behavior in situations involving resource allocation, conflict of interest, or reporting accuracy.
Exam questions may present ethical dilemmas embedded within policy or compliance contexts. For instance, a scenario might involve balancing cost management with patient access to necessary care. Responding appropriately requires both regulatory knowledge and ethical reasoning.
Cultivating ethical awareness also means recognizing the broader social implications of healthcare policies. Understanding how regulatory decisions affect vulnerable populations reinforces a sense of responsibility that extends beyond administrative efficiency.
Deep Exploration of Medicare Compliance for the AHIP AHM-510 Exam
One of the most intricate and consequential aspects of the AHIP AHM-510 Exam is the domain of Medicare compliance. This area delves into the precise rules, reporting protocols, and ethical obligations that ensure Medicare operates within lawful and transparent boundaries. Compliance is the cornerstone of credibility for healthcare organizations and professionals alike. Those preparing for this examination must not only grasp regulations theoretically but also understand their operational implications across diverse healthcare environments.
Medicare compliance represents a convergence of law, ethics, and administrative precision. It involves systematic oversight to prevent fraud, waste, and abuse, while safeguarding patient rights and ensuring proper reimbursement for services rendered. Candidates sitting for the AHM-510 must therefore comprehend compliance both as a regulatory mandate and as a moral duty that underpins public trust in healthcare systems.
The exam tests familiarity with the Centers for Medicare & Medicaid Services (CMS) guidelines, auditing mechanisms, enforcement strategies, and the frameworks that define corporate integrity. Candidates must analyze case scenarios, interpret compliance breaches, and determine appropriate corrective actions—all while adhering to federal statutes. The ability to internalize this balance between procedural correctness and ethical discernment is what distinguishes a merely competent test-taker from a genuinely proficient healthcare professional.
Understanding the Framework of Medicare Compliance
Compliance in the Medicare context refers to adherence to federal and state laws, CMS rules, and organizational policies that regulate program administration. Its primary goal is to ensure that beneficiaries receive entitled services without deception, misrepresentation, or financial exploitation. Compliance extends beyond clerical accuracy; it embodies the principle of accountability at every administrative and operational level.
The framework of Medicare compliance operates through multiple layers. At the highest level, federal legislation defines broad standards, including provisions from the Social Security Act, the False Claims Act, and the Anti-Kickback Statute. These laws serve as the backbone of regulatory enforcement. CMS, as the overseeing agency, interprets and enforces these laws through rules, manuals, and operational guidance.
Within healthcare organizations, compliance programs translate these federal requirements into actionable policies and procedures. A robust compliance program typically includes written standards of conduct, training for employees, auditing systems, mechanisms for reporting misconduct, and disciplinary protocols. The design of these programs reflects CMS’s guidance on “effective compliance,” a term that emphasizes proactive prevention rather than reactive correction.
Candidates must understand the essential elements of these programs, such as risk assessment, monitoring, and corrective action plans. The AHM-510 Exam frequently evaluates comprehension of how these components work in harmony to create a culture of compliance that sustains integrity and mitigates risk.
The Role of Oversight and Enforcement
Oversight is the backbone of Medicare compliance. CMS and the Office of Inspector General (OIG) collaborate to identify irregularities, investigate potential fraud, and enforce accountability. Their oversight mechanisms function as both deterrent and safeguard, ensuring the Medicare system operates efficiently and ethically.
The OIG has extensive authority to audit, subpoena, and sanction entities that violate Medicare regulations. Familiarity with OIG’s enforcement role is essential for candidates, as exam scenarios often incorporate cases involving billing errors, improper payments, or deliberate fraud. Understanding enforcement procedures—including administrative penalties, exclusion from federal programs, and civil monetary fines—is vital.
Equally significant is recognizing that enforcement is not solely punitive. It is educational and preventive. Organizations that discover compliance breaches and report them voluntarily can mitigate penalties, provided they demonstrate good faith and effective corrective measures. This principle reinforces the value of transparency within the compliance culture.
Fraud, Waste, and Abuse Prevention
Preventing fraud, waste, and abuse is a central theme in both Medicare operations and the AHM-510 Exam. Fraud entails intentional deception or misrepresentation to gain unauthorized benefits, such as falsifying billing records or submitting claims for services not rendered. Waste involves inefficient or unnecessary use of resources, often resulting from negligence or poor management. Abuse encompasses practices that, while not fraudulent, are inconsistent with sound fiscal or medical standards.
To prevent these issues, healthcare organizations implement auditing systems and training initiatives that reinforce ethical behavior. Employees are encouraged to recognize red flags, such as duplicate billing, inflated service codes, or improper patient inducements.
The AHM-510 Exam may include questions that require identification of potential fraud indicators or analysis of appropriate responses when suspicious patterns emerge. Understanding the procedural sequence—detect, investigate, report, and remediate—is essential. Candidates should also know how whistleblower protections under the False Claims Act encourage transparency and accountability within organizations.
Documentation and Record-Keeping
Meticulous documentation forms the backbone of compliance integrity. Accurate records demonstrate that services were provided appropriately, billed correctly, and supported by clinical evidence. Errors in documentation can trigger audits, financial penalties, or even legal action.
Candidates must understand the standards governing medical record maintenance, including retention periods, accessibility, and confidentiality. CMS guidelines require that documentation substantiate medical necessity, a concept central to Medicare reimbursement. Medical necessity ensures that services provided to beneficiaries are reasonable, essential, and consistent with accepted medical practices.
Record-keeping also intersects with privacy regulations, particularly the Health Insurance Portability and Accountability Act (HIPAA). Candidates must be able to differentiate between compliance requirements related to billing accuracy and those concerning patient privacy. The AHM-510 Exam frequently tests awareness of how these domains interrelate and overlap within daily operations.
The Importance of Internal Audits
Internal audits serve as proactive instruments of compliance assurance. They provide an opportunity for organizations to evaluate the effectiveness of their compliance programs before external scrutiny occurs. A well-structured audit examines documentation accuracy, billing procedures, staff adherence to protocols, and the timeliness of corrective actions.
Candidates should understand that audits are not solely diagnostic but educational. They help identify systemic weaknesses, refine training programs, and reinforce accountability at every level. When irregularities are detected, corrective actions—such as re-training, policy revisions, or reimbursement adjustments—are implemented to prevent recurrence.
The exam may include case studies requiring candidates to identify appropriate responses to audit findings. Recognizing the importance of confidentiality, data accuracy, and prompt reporting within the audit process reflects a mature understanding of compliance governance.
Ethics and Decision-Making in Compliance
Compliance is not purely procedural; it is fundamentally ethical. Decision-making in this realm often involves moral discernment where legal obligations intersect with human welfare. Ethical dilemmas can arise when cost efficiency conflicts with patient access or when organizational loyalty challenges personal integrity.
The AHM-510 Exam assesses a candidate’s ability to evaluate such dilemmas through established ethical principles—autonomy, beneficence, nonmaleficence, and justice. For instance, when faced with a situation involving ambiguous billing practices, a compliant response requires prioritizing transparency over convenience. Ethical decision-making fosters trust among patients, regulators, and employees alike.
Cultivating ethical awareness involves continuous reflection. Professionals should question whether their actions align with both the letter and the spirit of Medicare regulations. The exam’s focus on ethics ensures that certified individuals not only follow rules but also embody integrity in their professional conduct.
Training and Education as Compliance Tools
Effective compliance is sustained through continuous education. Employees at every organizational level must understand their responsibilities and the consequences of non-compliance. Training programs should be tailored to the specific roles of staff, addressing both general awareness and specialized regulatory knowledge.
The AHM-510 Exam emphasizes this element of compliance management, testing the candidate’s grasp of how training supports organizational resilience. Training should not be limited to initial onboarding but should occur regularly to address regulatory updates and evolving risk areas.
Monitoring the effectiveness of training programs through feedback and performance metrics ensures continuous improvement. Candidates must be aware that an informed workforce constitutes the first line of defense against inadvertent errors and deliberate violations.
Reporting Mechanisms and Whistleblower Protections
Encouraging open communication is a defining characteristic of effective compliance systems. Organizations must establish safe and confidential channels for reporting potential violations. Anonymous hotlines, secure digital portals, and designated compliance officers serve this purpose.
The False Claims Act provides protections for whistleblowers who disclose fraudulent activities. Understanding the scope of these protections is essential for AHM-510 candidates, as it underscores the ethical obligation to report wrongdoing without fear of retaliation.
A well-functioning reporting system not only prevents misconduct but also demonstrates organizational commitment to ethical governance. When employees trust the reporting process, they are more likely to participate in maintaining compliance integrity.
Risk Assessment and Mitigation
Risk assessment forms a strategic component of compliance management. Organizations must continually identify areas susceptible to violations, such as billing processes, vendor relationships, or data handling. Once risks are recognized, they are prioritized according to likelihood and potential impact.
Mitigation strategies may involve revising policies, strengthening oversight, or introducing technological safeguards. For example, automated claims monitoring systems can detect anomalies before they escalate into systemic problems. Candidates should understand how such systems function within broader compliance architecture.
The AHM-510 Exam evaluates understanding of how risk assessment supports prevention. Candidates may be required to interpret risk data, recommend mitigation measures, or determine the adequacy of a compliance response. Recognizing that risk management is dynamic—requiring constant adaptation to new regulations and technologies—is vital for long-term competence.
Organizational Culture and Leadership in Compliance
Leadership plays a decisive role in shaping compliance culture. A top-down commitment to ethical conduct inspires confidence and accountability throughout the organization. Senior executives must model integrity and allocate sufficient resources for compliance programs.
Candidates should appreciate that culture cannot be mandated; it must be cultivated. Transparent communication, recognition of ethical behavior, and consistent enforcement of rules foster an environment where compliance becomes a shared value rather than a burdensome requirement.
The AHM-510 Exam may assess understanding of leadership responsibilities, including how tone-at-the-top influences employee behavior and how governance structures integrate compliance oversight into daily operations.
Adapting to Regulatory Change
Healthcare regulations are never static. The Medicare system evolves through legislative reforms, CMS updates, and judicial interpretations. Staying informed about these developments is a continuous responsibility for healthcare professionals.
Candidates must understand how regulatory change impacts compliance protocols. For instance, adjustments to payment methodologies or eligibility rules may necessitate updates to documentation standards, billing systems, and staff training. The ability to adapt swiftly and accurately distinguishes effective professionals in this field.
Exam questions often evaluate this adaptability through hypothetical policy shifts that require analytical response. Demonstrating comprehension of how to align operations with new regulations exemplifies both foresight and competence.
Advanced Understanding of Medicare Policy and Legislative Evolution
The AHIP AHM-510 Exam challenges candidates to engage deeply with the intricate policies and legislative developments that shape Medicare’s structure. To excel in this section of the exam, it is essential to cultivate a comprehensive understanding of how laws, administrative actions, and regulatory changes have influenced Medicare’s evolution since its inception. The system reflects the continuous balancing of social priorities, fiscal responsibility, and healthcare equity, demanding an analytical perspective that blends historical awareness with forward-thinking interpretation.
Understanding policy and legislative evolution in Medicare is not simply about memorizing dates or statutes. It involves perceiving the philosophical and economic forces behind every reform, recognizing the motivations that drive policy shifts, and interpreting how those transformations affect beneficiaries, providers, and administrators. The AHM-510 Exam tests the candidate’s ability to contextualize these changes and apply this understanding to complex regulatory scenarios.
Medicare’s policy landscape is an intricate mosaic of federal statutes, agency regulations, and judicial interpretations. It reflects a dialogue between lawmakers, healthcare professionals, and the public—each shaping how healthcare is financed, delivered, and monitored. Candidates preparing for this exam must approach the subject with both intellectual rigor and a sense of moral awareness, recognizing that each regulation has profound implications for human welfare.
The Genesis of Medicare and Its Foundational Principles
The establishment of Medicare in 1965 marked one of the most transformative moments in American social policy. Enacted under Title XVIII of the Social Security Act, it sought to provide health insurance to older adults who, due to age and declining employment participation, were often excluded from private coverage. Its guiding principle was equity—ensuring that age would not become a barrier to essential healthcare access.
In its earliest form, Medicare consisted of two primary components: Hospital Insurance (Part A) and Medical Insurance (Part B). These programs were structured around a partnership between federal funding and private healthcare delivery, embodying a uniquely American blend of public oversight and private participation.
Candidates must recognize that the ideological foundation of Medicare was built upon solidarity and social responsibility. The system reflected the belief that collective contributions through payroll taxes could sustain a safety net for the elderly. Understanding this principle is essential because much of Medicare’s subsequent evolution has revolved around reconciling fiscal sustainability with expanding demand.
Legislative Expansions and Reforms
Medicare’s journey since 1965 has been characterized by continuous legislative refinement. Several key acts have reshaped its design, coverage scope, and operational mechanisms. Each reform introduced new challenges and responsibilities for healthcare administrators—subjects that often appear in the AHM-510 Exam.
One of the earliest major reforms, the Social Security Amendments of 1972, expanded Medicare eligibility to include individuals under 65 with certain disabilities and those with End-Stage Renal Disease (ESRD). This change demonstrated Medicare’s adaptability and its evolving definition of vulnerability within the healthcare landscape.
The Balanced Budget Act of 1997 represented another pivotal moment. It introduced the Medicare+Choice program, later renamed Medicare Advantage (Part C). This reform emphasized managed care as a strategy for controlling costs while offering beneficiaries more flexible options. Candidates must understand how the Act reshaped the relationship between Medicare, private insurers, and healthcare providers.
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) marked the birth of Part D, extending coverage to prescription drugs—a monumental expansion addressing one of the most pressing gaps in elderly healthcare. This act also encouraged the use of private plans to administer benefits, reinforcing the market-oriented dimension of Medicare.
Each legislative milestone reflects the perpetual tension between accessibility, affordability, and sustainability. For candidates, recognizing how these reforms interact with modern policies provides valuable insight into Medicare’s strategic direction and its regulatory complexities.
The Administrative Role of CMS
The Centers for Medicare & Medicaid Services (CMS) serves as the principal administrative body overseeing Medicare operations. Understanding its role is vital for AHM-510 candidates, as CMS regulations shape nearly every aspect of Medicare compliance, reimbursement, and service delivery.
CMS interprets federal legislation, issues operational guidance, and enforces compliance standards. It maintains the Medicare Benefit Policy Manual, Claims Processing Manual, and Program Integrity Manual—key resources for understanding procedural and policy application.
Beyond administration, CMS also drives innovation through initiatives such as the Medicare Shared Savings Program and value-based payment models. These programs reflect a shift from volume-based to outcome-based healthcare delivery. Candidates must appreciate how such policies influence organizational behavior, financial incentives, and patient care quality.
The AHM-510 Exam often includes questions that test comprehension of CMS’s multifaceted responsibilities. Understanding how the agency balances regulatory enforcement with policy innovation demonstrates both technical and strategic knowledge.
The Economic Dimensions of Medicare Policy
Medicare’s evolution cannot be separated from economic realities. Its sustainability depends on effective cost management, equitable distribution of resources, and continuous adaptation to demographic trends. Candidates preparing for the AHM-510 Exam must be able to analyze how economic factors shape policy decisions and program design.
Funding for Medicare primarily derives from payroll taxes, premiums, and general federal revenue. However, with an aging population and rising healthcare costs, maintaining fiscal balance has become increasingly challenging. Reforms such as the implementation of prospective payment systems and bundled payments emerged as responses to these pressures, promoting efficiency while preserving quality.
Understanding cost-control mechanisms—such as Diagnosis-Related Groups (DRGs) and the Resource-Based Relative Value Scale (RBRVS)—is crucial for exam success. These systems regulate reimbursement by linking payment levels to standardized measures of resource utilization and clinical complexity.
Economic prudence also intersects with ethics. Policymakers must navigate the delicate balance between containing costs and ensuring that essential services remain accessible to all beneficiaries. Recognizing this interplay underscores the sophistication required to interpret Medicare policy effectively.
The Role of Quality and Accountability in Policy Design
Modern Medicare policy emphasizes quality, transparency, and accountability as measures of success. Candidates must understand how these principles are embedded within policy frameworks and performance evaluation models.
Programs such as the Hospital Readmissions Reduction Program (HRRP) and the Merit-based Incentive Payment System (MIPS) tie reimbursement to quality metrics, promoting improved patient outcomes and discouraging inefficiency. The concept of “value-based care” epitomizes this evolution—prioritizing outcomes over volume.
For AHM-510 examinees, recognizing how quality-based payment models alter operational strategies within healthcare organizations is crucial. They must analyze how data reporting, patient satisfaction, and clinical outcomes influence policy compliance and financial performance.
Policy accountability also extends to transparency in communication. CMS mandates public reporting of certain provider performance data, reinforcing the importance of integrity and patient empowerment. Understanding the rationale behind these policies demonstrates comprehensive mastery of the subject.
The Influence of Demographics and Social Trends
Medicare policy is profoundly shaped by demographic and social trends. As the population ages, the number of beneficiaries increases, straining financial and administrative resources. The exam may test understanding of how demographic projections influence long-term Medicare planning.
Beyond aging, changing patterns in chronic disease prevalence, technology adoption, and socioeconomic disparities also drive policy adaptation. The shift toward preventive care—exemplified by expanded coverage for screenings and wellness visits—reflects a proactive response to evolving healthcare needs.
Candidates should also recognize the influence of social movements on Medicare policy, such as advocacy for disability rights or the emphasis on health equity. Understanding how societal values shape policy development provides a nuanced perspective that distinguishes advanced learners from superficial readers.
Regulatory Harmonization and Interagency Coordination
The administration of Medicare involves coordination across multiple agencies and policy frameworks. The Department of Health and Human Services (HHS), CMS, the Office of Inspector General (OIG), and the Government Accountability Office (GAO) each play distinct yet interconnected roles.
Candidates must understand how these agencies collaborate to enforce compliance, evaluate program integrity, and manage fraud prevention initiatives. For example, CMS sets operational standards, while OIG enforces legal accountability through investigations and sanctions. The GAO, meanwhile, conducts audits to ensure fiscal responsibility and transparency in program administration.
Such interagency collaboration exemplifies a system of checks and balances, designed to protect public funds and uphold ethical governance. Recognizing how these institutions interact helps candidates appreciate the complexity of Medicare’s regulatory environment.
The Policy Cycle: From Proposal to Implementation
Understanding how a Medicare policy evolves from conception to execution is fundamental for AHM-510 success. The policy cycle typically involves five stages: problem identification, formulation, legislative approval, implementation, and evaluation.
Candidates should analyze how stakeholders—lawmakers, healthcare providers, advocacy groups, and beneficiaries—participate in each stage. For instance, policy formulation often involves consultation with experts and analysis of cost-effectiveness studies. Once legislation is enacted, CMS translates it into operational rules and disseminates guidance to providers.
The final stage, evaluation, determines whether the policy achieves its intended outcomes. Data collection, analysis, and stakeholder feedback play crucial roles in refining or amending existing rules. A comprehensive understanding of this cycle enables candidates to grasp how Medicare remains both adaptable and accountable.
Judicial and Administrative Interpretations
Medicare policy is not static; it is constantly redefined through judicial and administrative interpretation. Court decisions, administrative appeals, and CMS rulings often clarify ambiguities or set precedents that shape future policy.
Candidates preparing for the AHM-510 Exam should understand how judicial review functions within the Medicare system. For example, disputes over coverage determinations, payment denials, or provider sanctions may escalate to administrative law judges or federal courts. Familiarity with these procedural pathways enhances comprehension of the system’s legal framework.
Administrative interpretations, such as CMS memoranda or program transmittals, serve as practical guides for implementation. Candidates should recognize their authority and the necessity of staying current with updates.
Strategic Mastery of Medicare Compliance and Regulatory Oversight
The landscape of Medicare compliance demands precision, foresight, and an in-depth understanding of regulatory structures. For candidates pursuing success in the AHIP AHM-510 Exam, the ability to interpret and apply compliance requirements within healthcare organizations represents one of the most intellectually rigorous and ethically charged components of preparation. Mastery of this domain requires not only memorization of statutes but also the cultivation of analytical reasoning that connects policy principles to real-world administrative behavior.
Medicare compliance functions as a protective framework that sustains the integrity of the entire program. Its regulations ensure that public funds are spent responsibly, that beneficiaries receive legitimate services, and that providers uphold professional and legal standards. Understanding how this framework operates—and how it evolves in response to new threats and innovations—is indispensable for advanced-level examinees.
Compliance within Medicare is guided by statutes, agency regulations, and ethical mandates that intersect across numerous operational levels. It serves as both a deterrent to misconduct and a proactive mechanism for ensuring transparency and fairness. Candidates preparing for the AHM-510 Exam must appreciate this dual nature, recognizing that compliance is as much about culture and accountability as it is about technical enforcement.
The Foundations of Medicare Compliance
Compliance begins with adherence to the Social Security Act, the foundational legislation that established Medicare and outlined the authority of the federal government to oversee its operation. This act grants power to the Department of Health and Human Services (HHS) and the Centers for Medicare & Medicaid Services (CMS) to implement detailed regulations governing provider conduct, billing practices, and beneficiary protection.
Understanding these origins provides essential context for interpreting the modern compliance environment. Over the decades, new layers of legislation—such as the False Claims Act, the Anti-Kickback Statute, and the Stark Law—have fortified the framework against fraud, waste, and abuse. Each statute represents a unique yet interconnected effort to maintain ethical and fiscal integrity within the healthcare system.
Candidates must understand not only what these laws prohibit but also how they are enforced and interpreted. The compliance landscape operates as a continuum where legal mandates interact with administrative policies, forming a dynamic system that adapts to emerging challenges.
The Role of the Office of Inspector General
Within this vast regulatory network, the Office of Inspector General (OIG) occupies a crucial position. Tasked with preventing fraud, promoting efficiency, and safeguarding program integrity, the OIG acts as both a watchdog and a policy advisor. It issues compliance program guidance documents that outline best practices for healthcare organizations seeking to align their operations with federal expectations.
These guidance documents are central to understanding compliance at a practical level. They provide frameworks for developing internal controls, conducting risk assessments, and implementing reporting systems. For the AHM-510 Exam, familiarity with OIG guidance demonstrates advanced comprehension of how compliance principles translate into operational strategies.
The OIG’s enforcement capabilities extend beyond advisory functions. Through audits, investigations, and administrative sanctions, it ensures that organizations adhere to ethical and legal standards. Understanding the scope of OIG authority, including its coordination with other federal agencies, reinforces a candidate’s command of the regulatory ecosystem.
Building Effective Compliance Programs
An effective compliance program is the cornerstone of ethical healthcare administration. Candidates must understand the seven key elements traditionally recommended by the OIG: written policies and procedures, compliance leadership, training and education, effective communication, monitoring and auditing, disciplinary standards, and corrective action.
These components serve as an integrated structure designed to detect and prevent misconduct. A robust compliance program not only fulfills legal obligations but also fosters a culture of accountability and continuous improvement. The AHM-510 Exam may assess understanding of how these elements interact, how they are implemented, and how they contribute to risk mitigation.
Building such a program requires more than administrative precision. It demands an understanding of organizational psychology, leadership ethics, and operational risk. Candidates should be able to analyze how internal governance models affect compliance behavior and how leadership commitment can transform regulatory adherence into a shared organizational value.
Enforcement and Penalties
The enforcement of Medicare compliance is multifaceted, involving administrative actions, civil penalties, and, in severe cases, criminal prosecution. The False Claims Act, for instance, imposes liability on individuals or organizations that knowingly submit false claims for payment. Penalties can include substantial fines and exclusion from federal healthcare programs.
The Anti-Kickback Statute prohibits financial arrangements that could influence patient referrals or the use of particular services. Violations can result in criminal charges, emphasizing the gravity of maintaining ethical integrity. The Stark Law, meanwhile, restricts physician self-referral for designated health services covered by Medicare, reinforcing the separation between clinical judgment and financial incentives.
Candidates must grasp how these laws function collectively to protect program integrity. Understanding the nuances of enforcement—such as intent, materiality, and administrative discretion—distinguishes a candidate who memorizes from one who truly comprehends.
The Role of Audits and Program Integrity
Auditing represents one of the most critical mechanisms for maintaining Medicare compliance. Both internal and external audits ensure that claims are accurate, documentation is complete, and services meet coverage requirements. CMS conducts various audit programs, including Recovery Audit Contractor (RAC) reviews, Medicare Administrative Contractor (MAC) oversight, and Zone Program Integrity Contractor (ZPIC) investigations.
Candidates should be familiar with the purpose and scope of each type of audit. For example, RACs focus on identifying improper payments through data analysis and claim review, while MACs handle daily claim processing and provider education. ZPICs target potential fraud through investigative methodologies.
Auditing not only serves as a corrective tool but also as a preventive one. Regular internal audits help organizations identify vulnerabilities before they escalate into compliance violations. Understanding how these processes interrelate is vital for developing comprehensive risk management strategies.
Data Integrity and Technological Oversight
In the era of digital transformation, data integrity has become a central pillar of Medicare compliance. Electronic health records, billing systems, and data exchanges all require strict adherence to security and accuracy standards. CMS regulations emphasize confidentiality, data validity, and system integrity as essential components of program accountability.
Candidates must comprehend how technology influences compliance dynamics. For instance, data analytics now play a pivotal role in detecting fraudulent billing patterns or unusual utilization trends. Artificial intelligence and predictive modeling assist regulators in identifying anomalies before they result in systemic abuse.
However, these technological advancements also introduce new vulnerabilities. Data breaches, unauthorized access, and inaccurate coding can compromise both financial and ethical obligations. An advanced understanding of these risks, combined with strategies to mitigate them, reflects the level of sophistication expected in the AHM-510 Exam.
Ethical Imperatives in Compliance Management
Compliance is not merely a legal obligation—it is a moral contract between the healthcare system and society. Candidates must appreciate that ethical decision-making underlies every regulatory standard. While laws prescribe the minimum acceptable behavior, ethics guide actions beyond compliance, fostering integrity even in ambiguous circumstances.
Healthcare administrators must navigate dilemmas involving confidentiality, resource allocation, and equitable treatment. The AHM-510 Exam may test the candidate’s ability to apply ethical reasoning to complex compliance scenarios. Recognizing that compliance transcends bureaucracy and reflects humanity’s moral compass distinguishes exceptional candidates from ordinary ones.
Creating an ethical culture requires leadership that models integrity, communication that promotes transparency, and systems that reward honesty. Ethical compliance is sustainable only when it becomes part of the organization’s collective conscience, not merely an external imposition.
The Evolution of Regulatory Oversight
Regulatory oversight within Medicare is dynamic, continuously adapting to social, economic, and technological changes. Over the years, CMS has refined its compliance strategy to balance enforcement with education, shifting from punitive control to collaborative improvement.
Initiatives such as the Compliance Program Effectiveness Framework and the Provider Compliance Group illustrate this evolution. These efforts emphasize proactive engagement with providers, focusing on guidance and training rather than mere punishment. Candidates should understand how this shift aligns with modern governance theories that prioritize partnership over policing.
The regulatory environment also responds to macro-level developments, such as economic recessions, demographic shifts, or public health emergencies. For example, during crises, CMS may issue temporary waivers or flexibilities to ensure continuity of care. Recognizing how such adaptations occur and their legal basis enhances analytical depth for exam success.
Comprehensive Strategies for Exam Readiness and Cognitive Mastery
Success in the AHIP AHM-510 Exam hinges not only on knowledge acquisition but also on the cultivation of strategic study habits, cognitive resilience, and practical application skills. The exam assesses both comprehension of complex Medicare policies and the ability to apply them in multifaceted scenarios, making preparation a rigorous intellectual endeavor.
Preparation begins with a deliberate approach to time management. Candidates often encounter an expansive breadth of topics, from Medicare program intricacies to regulatory compliance and ethical frameworks. Structuring study time around a comprehensive blueprint ensures that all areas are addressed systematically. Allocating dedicated periods for policy review, practice exercises, and reflective synthesis helps internalize material and fosters confidence in tackling challenging questions.
Equally important is the incorporation of active learning strategies. Passive reading is insufficient for mastering advanced concepts; candidates should engage with the material through summarization, paraphrasing, and application exercises. This process transforms information into usable knowledge and strengthens cognitive retention. Concept mapping, scenario analysis, and question prediction exercises are particularly effective for bridging theory and practice.
Cognitive Strategies for Retention and Recall
Understanding Medicare policies, compliance frameworks, and ethical principles requires more than rote memorization. Candidates must employ cognitive strategies that enhance comprehension and recall. Spaced repetition, where material is reviewed at increasing intervals, combats memory decay and reinforces long-term retention. Interleaving—alternating between topics—encourages flexible thinking and facilitates the integration of concepts across different domains.
Elaboration techniques are also critical. By connecting new information to existing knowledge, candidates deepen understanding and create mental scaffolding for complex concepts. For example, linking legislative history to current reimbursement policies or associating compliance mechanisms with real-world auditing scenarios promotes both retention and practical application.
Visualization strategies aid in conceptual clarity. Diagramming Medicare structures, workflow processes, or regulatory hierarchies allows candidates to perceive systemic relationships and interdependencies. This spatial representation of knowledge enables faster recall and more accurate application during scenario-based questions on the AHM-510 Exam.
Practice with Simulated Scenarios
Simulated scenarios are essential for bridging theoretical knowledge and practical application. The AHM-510 Exam frequently presents case studies requiring the integration of multiple concepts, including eligibility determinations, policy interpretation, and ethical decision-making. Practicing with such scenarios develops analytical reasoning and decision-making agility.
Candidates should approach each scenario systematically. Identifying relevant regulations, assessing risk factors, evaluating ethical implications, and determining appropriate corrective actions are steps that mirror real-world problem-solving. Reflecting on reasoning after each exercise strengthens cognitive pathways and reduces the likelihood of errors under timed conditions.
Practice should also encompass question formats and timing. Multiple-choice questions can include nuanced distractors designed to test comprehension rather than simple recall. Engaging with sample questions repeatedly familiarizes candidates with these subtleties and hones time management skills, ensuring that each answer is considered with both accuracy and efficiency.
Enhancing Analytical Thinking
Analytical thinking is central to navigating the complexities of Medicare administration. The AHM-510 Exam emphasizes the capacity to synthesize information, identify regulatory intersections, and interpret policy implications. Candidates must develop a mindset that balances precision with contextual understanding.
One approach involves deconstructing complex questions into constituent components. For example, a scenario involving Part C enrollment may include eligibility verification, compliance obligations, reimbursement calculations, and ethical considerations. Breaking down the scenario allows for systematic application of knowledge while ensuring that all relevant aspects are addressed.
Critical reasoning exercises further enhance analytical capacity. Evaluating policy changes, assessing potential outcomes of compliance decisions, and comparing alternative interpretations cultivates the intellectual flexibility required to succeed on advanced examinations. These skills translate into professional competency, preparing candidates for real-world decision-making beyond the scope of the exam.
Integrating Ethical and Regulatory Considerations
Ethical reasoning is inseparable from regulatory comprehension in Medicare administration. Candidates must be prepared to apply both legal mandates and ethical principles when analyzing scenarios. Questions may involve conflicts between operational efficiency and patient welfare, or between cost containment and equitable access.
Applying ethical frameworks—such as beneficence, nonmaleficence, autonomy, and justice—enables candidates to make principled decisions even when regulations are ambiguous. The AHM-510 Exam evaluates the ability to balance these considerations alongside compliance requirements, highlighting the integrated nature of knowledge and ethical judgment.
Reflective exercises enhance ethical acumen. Candidates should regularly review case studies that present moral dilemmas, exploring the reasoning behind decisions and evaluating potential alternative approaches. This reflective practice strengthens moral discernment and supports consistent, principled responses under exam conditions.
Optimizing Exam-Day Performance
Exam-day preparation extends beyond mastery of content to include physical, psychological, and logistical readiness. Ensuring adequate rest, nutrition, and hydration supports cognitive function and concentration. Establishing a pre-exam routine—including review of key concepts, meditation, or light mental exercises—can reduce anxiety and enhance focus.
Time management during the exam is equally critical. Candidates should allocate time according to question complexity, ensuring that challenging items receive sufficient attention without sacrificing completion of the entire test. Strategic reading, highlighting keywords, and eliminating distractors methodically increase accuracy and efficiency.
Maintaining composure is essential. The exam may present unfamiliar scenarios or deceptively complex questions. Candidates should approach each question with calm analytical reasoning, applying learned strategies systematically rather than reacting impulsively. Confidence in preparation mitigates stress and enhances cognitive performance.
Continuous Review and Adaptive Learning
Even during the final stages of preparation, adaptive learning strategies remain valuable. Reviewing weak areas, analyzing incorrect practice responses, and updating study strategies based on performance metrics reinforces mastery. Candidates should embrace iterative refinement, using each study session to deepen understanding and correct misconceptions.
Adaptive learning also involves prioritization. Focusing on high-yield topics, emergent policy updates, and areas of personal difficulty ensures that preparation time is used efficiently. Combining targeted review with comprehensive synthesis promotes both breadth and depth of understanding.
Integrating Technology and Learning Tools
Digital tools can enhance preparation by providing interactive learning experiences and data-driven feedback. Practice question banks, online simulations, and digital note-taking systems allow candidates to engage dynamically with content. Tracking progress, analyzing patterns in responses, and revisiting challenging concepts create a personalized learning ecosystem.
Simulation tools can replicate exam conditions, reinforcing time management and scenario analysis skills. Digital flashcards, spaced repetition apps, and concept mapping software provide supplementary reinforcement that complements traditional study methods. Candidates who integrate technology strategically often achieve superior retention and application capabilities.
Cognitive Resilience and Stress Management
Preparing for an advanced exam such as the AHM-510 requires sustained mental effort. Cognitive resilience—the ability to maintain focus, adapt to challenges, and recover from setbacks—is critical. Stress management techniques, such as mindfulness, deep-breathing exercises, and scheduled breaks, support mental endurance and prevent burnout.
Developing resilience also involves cultivating a growth mindset. Viewing errors as opportunities for learning rather than failures encourages persistence and self-improvement. This perspective reinforces intellectual flexibility, allowing candidates to approach complex exam questions with curiosity and analytical clarity.
Applying Knowledge to Professional Practice
Although the AHM-510 Exam evaluates academic proficiency, the skills developed through preparation are immediately transferable to professional practice. Candidates trained in regulatory interpretation, ethical reasoning, and policy analysis become more effective healthcare administrators. They can implement compliance strategies, manage risk, and make informed decisions that balance operational demands with patient-centered care.
Practical application exercises, such as mock audits, case studies, or policy reviews, strengthen this professional competence. Candidates who approach exam preparation as a form of experiential learning gain a dual benefit: they enhance exam readiness while simultaneously elevating their professional capabilities.
Conclusion
Mastering the AHIP AHM-510 Exam requires a comprehensive understanding of Medicare policies, compliance frameworks, regulatory structures, and ethical principles. This exam evaluates not only factual knowledge but also the ability to apply complex concepts in practical, real-world scenarios. Through diligent preparation, candidates develop the analytical skills, ethical awareness, and procedural expertise necessary to navigate the multifaceted healthcare environment effectively.
A deep understanding of Medicare program components—Parts A, B, C, and D—forms the foundation for exam success. Candidates must be proficient in eligibility requirements, coverage options, enrollment procedures, and reimbursement structures. Alongside this, an advanced comprehension of legislative evolution, including key reforms and regulatory updates, allows candidates to contextualize current policies and anticipate their implications for healthcare administration.
Equally critical is mastery of compliance and ethical standards. Understanding the roles of CMS, the Office of Inspector General, and interagency coordination ensures that candidates can identify, prevent, and address potential violations. Skills in auditing, risk assessment, documentation, and ethical decision-making prepare candidates to uphold program integrity and maintain public trust.
Preparation strategies, including structured study plans, scenario-based practice, cognitive techniques, and exam-day readiness, equip candidates to handle the rigorous demands of the AHM-510 Exam. Integrating reflective learning and adaptive approaches enhances retention, analytical reasoning, and professional judgment.
Ultimately, success in the AHIP AHM-510 Exam reflects more than academic achievement; it signifies the ability to operate with competence, integrity, and insight within the Medicare system. Candidates who combine knowledge, preparation, and ethical discernment are well-positioned to contribute meaningfully to healthcare administration and to advance both their careers and the quality of patient care.