Test Name: NAPLEX - North American Pharmacist Licensure Examination
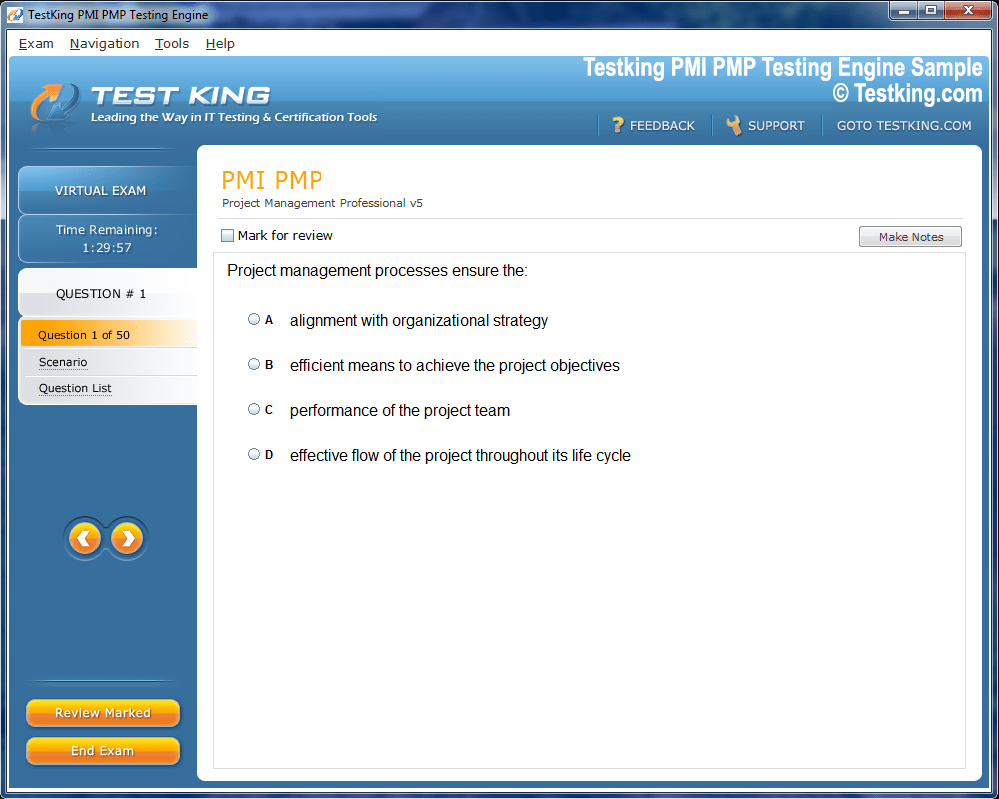
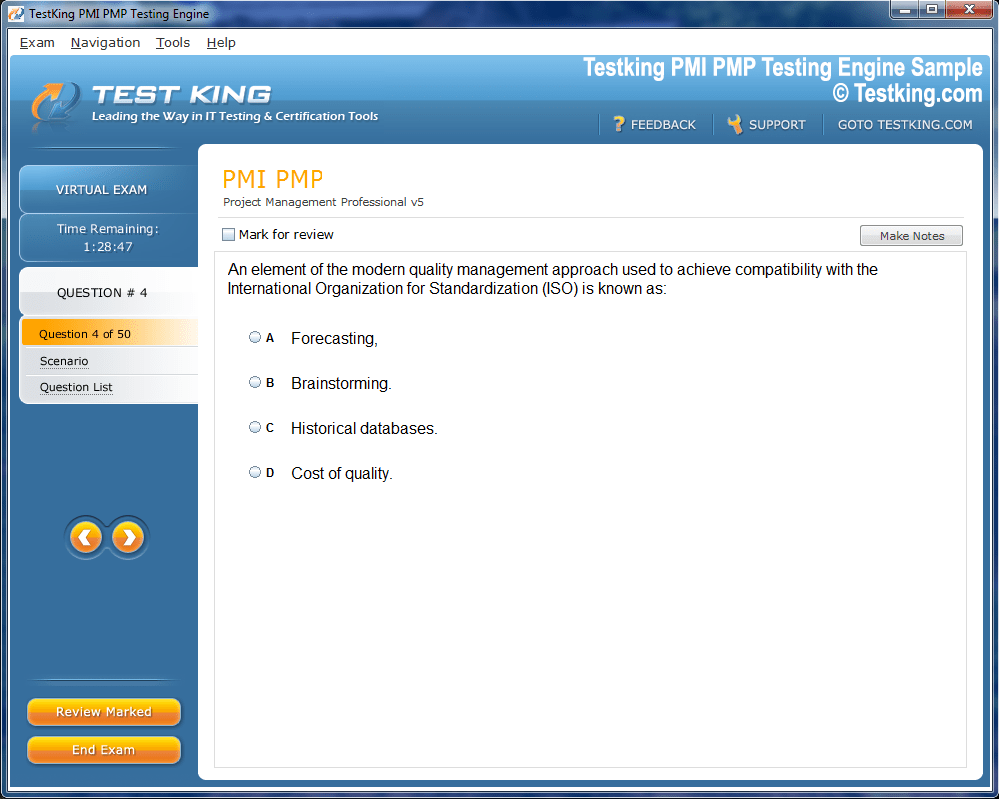
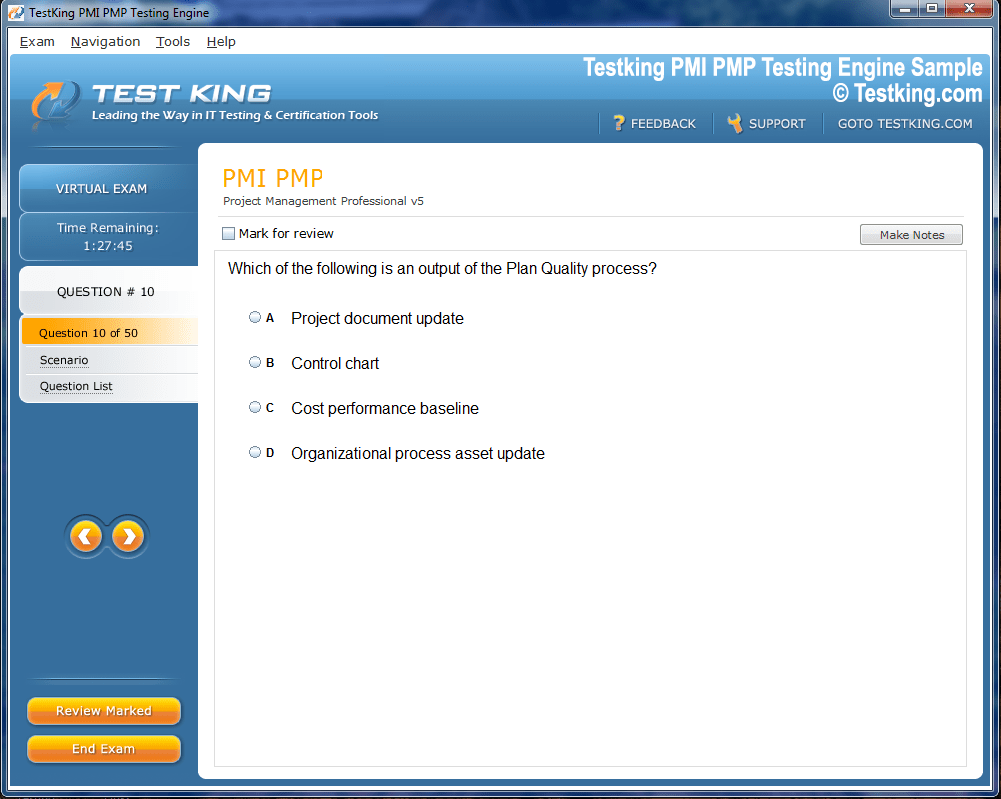
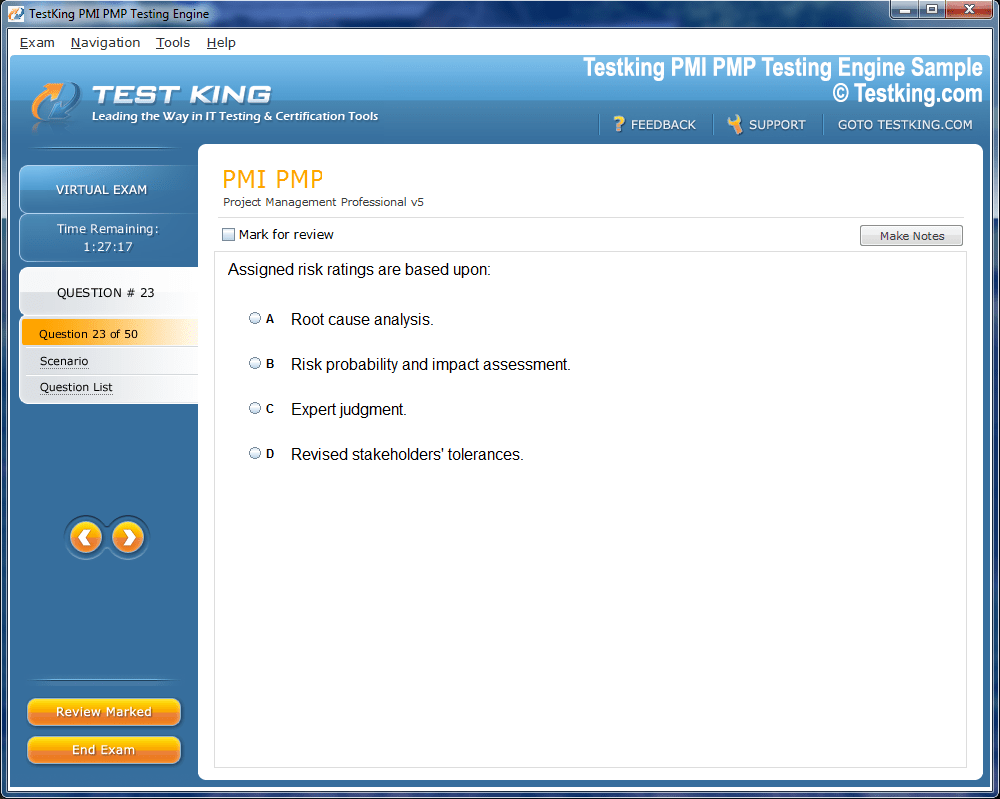
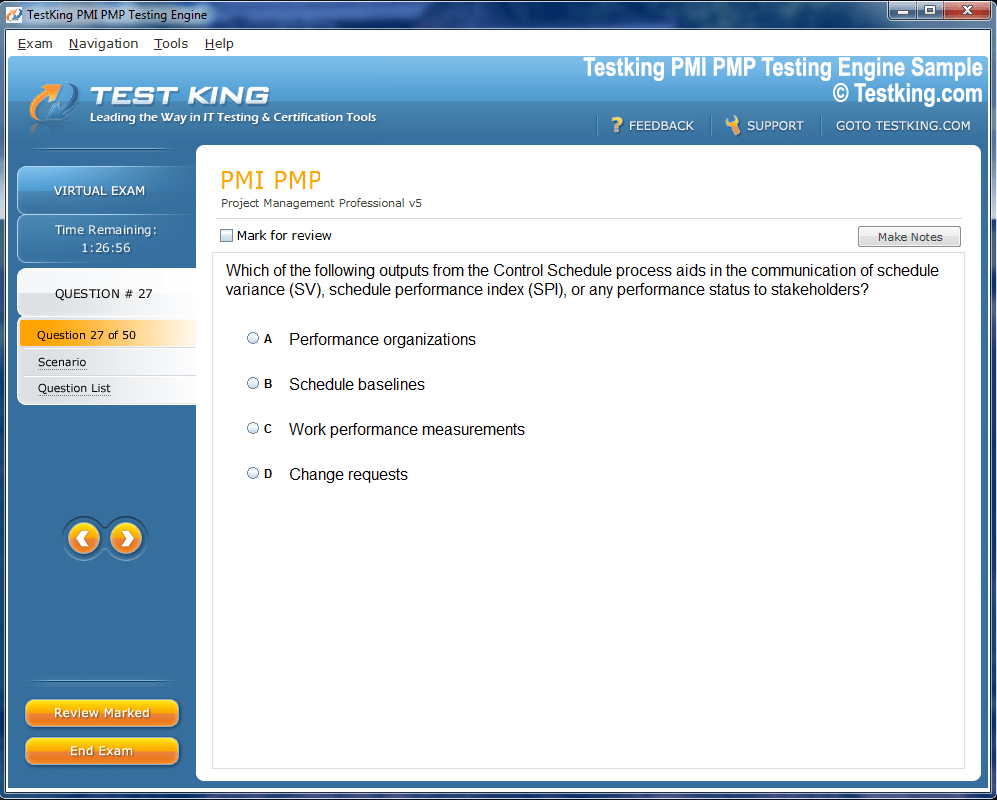
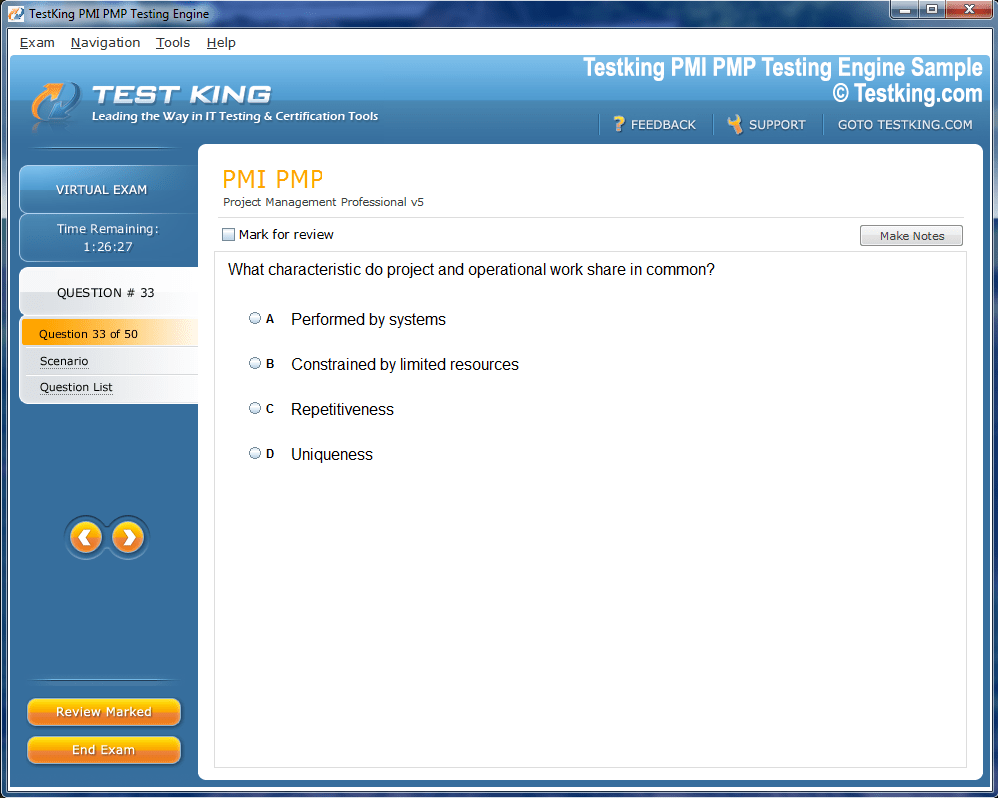
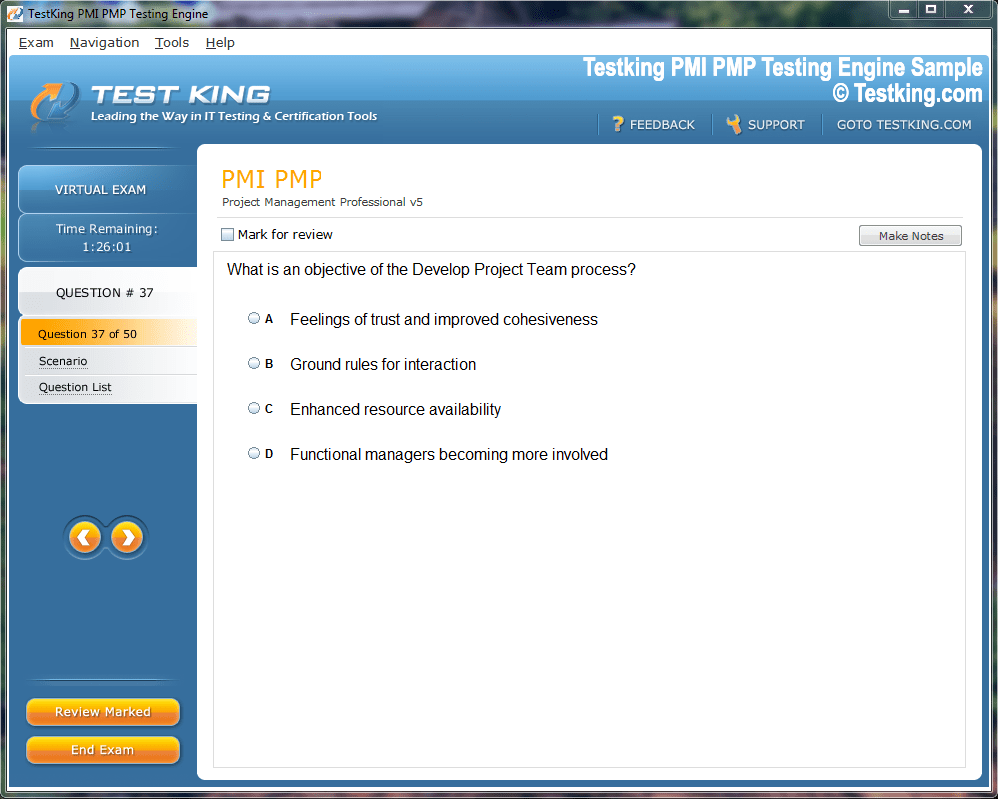
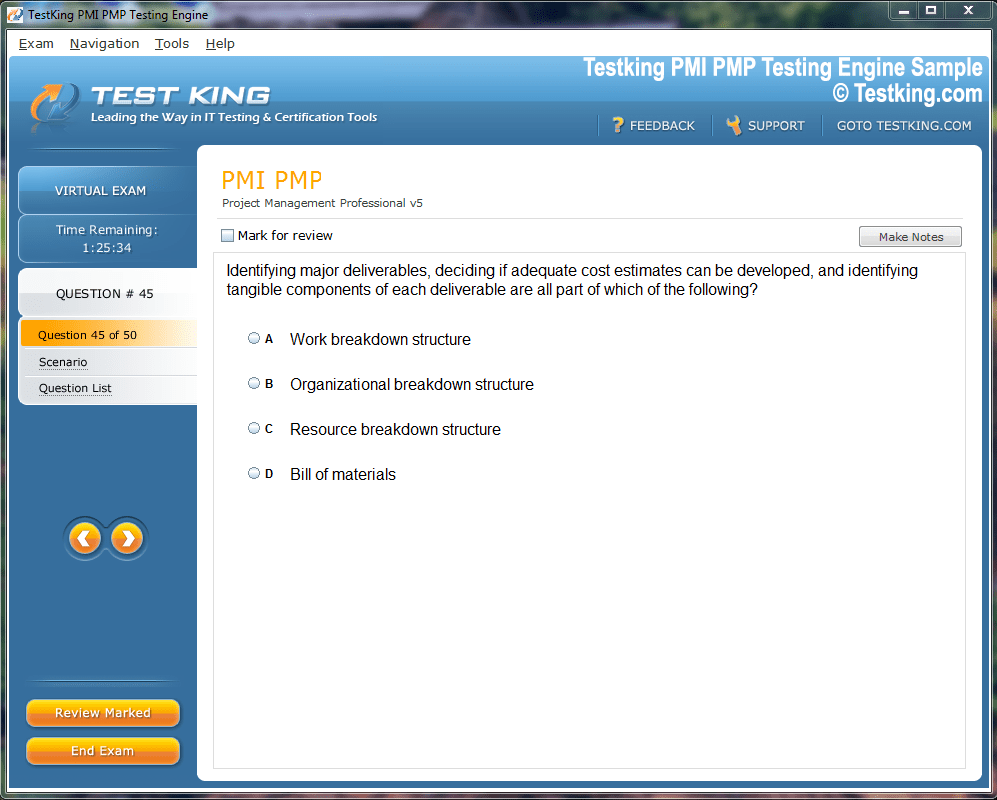
Product Screenshots

nop-1e =1
Strategies and Insights for NAPLEX Certification Preparation
For many fourth-year pharmacy students, the final months of their academic journey evoke a complex amalgamation of exhilaration, trepidation, and meticulous anticipation. After years of rigorous study, clinical rotations, and laboratory immersion, the prospect of entering the professional realm approaches with a palpable intensity. Yet, before one can fully embrace the responsibilities of a licensed pharmacist, a critical examination remains: the North American Pharmacist Licensure Examination (NAPLEX). This examination serves not merely as a procedural formality but as a definitive benchmark of knowledge, analytical acumen, and professional competence within the domain of pharmacy.
The preparation for the NAPLEX is an intricate odyssey, demanding both intellectual diligence and strategic foresight. Beyond rote memorization, candidates must cultivate an aptitude for clinical reasoning, pharmaceutical calculations, and patient-centered decision-making. The process can be stratified into three principal segments: initiating the application process, rigorous preparation for the examination, and navigating the logistics of test day. Mastery of these segments ensures that aspirants can traverse the labyrinthine structure of licensure requirements with efficacy and poise.
Initiating the Application Process
Timeliness in application submission is an often underappreciated determinant of success. Candidates who undertake the NAPLEX shortly after graduation generally exhibit higher rates of passage, attributable to the retention of freshly acquired knowledge. The initial phase entails a thorough engagement with the NAPLEX/MPJE Candidate Application Bulletin. This compendium is not merely a procedural checklist but a repository of essential instructions delineating eligibility criteria, registration mandates, and preparatory requisites. Its accessibility on multiple platforms facilitates comprehensive perusal and meticulous planning.
After familiarization with the bulletin, candidates must establish an NABP e-Profile. This digital interface functions as the centralized hub for examination-related activities, including requests for eligibility verification, acquisition of authorization to test (ATT), and submission of requests for ADA accommodations. It is imperative that the identification credentials within the e-Profile precisely mirror those on government-issued documentation, as discrepancies may precipitate administrative impediments on the day of testing.
The e-Profile also serves as a conduit for communication with the examining authority, allowing candidates to receive notifications, updates, and clarifications pertinent to the licensure process. Engaging with this platform diligently mitigates potential procedural pitfalls and instills a structured approach to the forthcoming examination journey.
Understanding Eligibility and Requirements
Eligibility criteria for the NAPLEX are multifaceted, encompassing academic completion, verification of experiential components, and adherence to professional standards. The Candidate Application Bulletin elucidates these criteria with precision, detailing the requisite documentation, timelines, and procedural nuances. For instance, verification of didactic coursework and experiential rotations must be submitted by the respective institutions to the NABP, ensuring an authoritative confirmation of the candidate's preparedness for professional practice.
Additionally, candidates must be cognizant of jurisdiction-specific regulations, as individual state boards may impose supplementary prerequisites or procedural variations. These can include fees, documentation of clinical experience, or supplemental assessments. The interplay of national and state-level requirements necessitates vigilant attention to detail and proactive engagement with regulatory entities.
Strategic Planning for Submission
Developing a strategic timeline for application submission is indispensable. Early submission not only aligns with the optimal window for examination scheduling but also allows for contingencies in case of administrative delays or additional documentation requests. Candidates are encouraged to maintain meticulous records of all correspondence, receipts, and confirmations, thereby constructing an archival reference that can be utilized in resolving potential discrepancies.
Proactive engagement with mentors, faculty advisors, or institutional coordinators can further streamline the application process. Such guidance provides insights into procedural nuances, expedites verification processes, and imparts pragmatic strategies for navigating bureaucratic intricacies. The amalgamation of structured planning, precise documentation, and informed mentorship constitutes a foundational pillar in the pursuit of NAPLEX readiness.
The Role of Psychological Preparedness
While procedural mastery is critical, psychological readiness constitutes an equally salient component of examination success. The anticipation of high-stakes assessment engenders cognitive and emotional pressures that can impede performance if left unaddressed. Cultivating resilience, focus, and adaptive coping mechanisms enhances the candidate's capacity to assimilate and apply knowledge under examination conditions. Techniques such as mindfulness, mental rehearsal, and structured reflection can fortify cognitive endurance and mitigate stress-induced cognitive interference.
Moreover, adopting a growth-oriented mindset fosters sustained engagement with the study material and encourages iterative self-assessment. By perceiving challenges as opportunities for refinement rather than insurmountable obstacles, candidates can maintain motivation and optimize learning efficacy throughout the preparatory period.
Integrating Practical Considerations
The application phase also encompasses practical considerations that extend beyond documentation. Financial planning is imperative, as examination fees, potential retakes, and ancillary costs necessitate prudent budgetary management. Additionally, candidates must anticipate logistical elements such as transportation to the testing center, accommodation arrangements if necessary, and contingency plans for unforeseen disruptions. Addressing these pragmatic dimensions ensures that extraneous factors do not encumber the examination experience.
Furthermore, candidates should acquaint themselves with institutional resources, such as practice tools, preparatory workshops, and advisory sessions, which can augment their readiness. Engaging with these resources strategically enhances familiarity with the examination format, promotes efficient time management, and bolsters confidence before the formal assessment.
Consolidating the Application Phase
In summation, the initial phase of NAPLEX preparation demands a harmonious integration of procedural diligence, strategic foresight, and psychological fortitude. Establishing an NABP e-Profile, submitting requisite documentation, and adhering to eligibility criteria constitute the structural framework within which candidates navigate their preparatory journey. Complementing these actions with proactive planning, mentorship engagement, and attention to practical logistics fosters a comprehensive approach to examination readiness.
The orchestration of these elements ensures that candidates enter the subsequent phases—study and test-day execution—with clarity, confidence, and a foundation of systematic preparedness. By meticulously attending to the intricacies of application and eligibility, aspirants not only fulfill regulatory mandates but also cultivate the disciplined mindset requisite for professional excellence in pharmacy practice.
Bridging to Preparation
Having secured eligibility and navigated the administrative complexities of the application, candidates are primed to transition into the study phase. This next stage emphasizes mastery of pharmacotherapeutics, clinical reasoning, and problem-solving skills. The rigor of this preparation mirrors the multifaceted demands of contemporary pharmacy practice, reinforcing both conceptual understanding and practical application.
Strategic study, informed by comprehensive outlines of examination content, ensures that candidates allocate effort efficiently across diverse topic areas. Structured schedules, iterative assessment, and targeted remediation underpin effective preparation. In tandem, cultivation of psychological resilience and adherence to pragmatic considerations equip candidates to confront the examination environment with composure and precision.
Strategizing Study for the NAPLEX
After securing eligibility and ensuring all application procedures are complete, the paramount task becomes systematic study. Preparation for the North American Pharmacist Licensure Examination (NAPLEX) is a complex endeavor requiring not only mastery of pharmacological principles but also the capacity for critical thinking, analytical reasoning, and practical application. Achieving competence necessitates a structured approach, blending comprehensive review, practice exercises, and assessment of conceptual retention.
A foundational step involves thorough engagement with the NAPLEX Content Outline. This document delineates the domains assessed on the examination, encompassing topics such as pharmacokinetics, therapeutics, patient care processes, and regulatory considerations. Utilizing the outline as a blueprint allows candidates to prioritize areas of relative weakness while ensuring comprehensive coverage. Conceptual interconnections between topics, such as drug interactions and patient counseling, must be emphasized to cultivate a holistic understanding rather than isolated memorization.
Establishing a Study Framework
Effective study strategies integrate time management, cognitive reinforcement, and iterative evaluation. Candidates are encouraged to develop a schedule that balances intensive review with periods of consolidation and reflection. This temporal structuring prevents cognitive fatigue and fosters durable retention. Allocating study blocks according to topic complexity and personal proficiency allows for targeted reinforcement while maintaining overall progress across the breadth of content.
Incorporating active learning techniques is particularly advantageous. Techniques such as self-explanation, concept mapping, and scenario-based problem solving facilitate deeper understanding. Engaging with clinical vignettes or simulated patient interactions not only reinforces pharmacological knowledge but also enhances decision-making acuity—a critical skill in the NAPLEX context.
Practice Examinations as Diagnostic Tools
The employment of practice examinations is integral to assessing preparedness and guiding further study. The Pre-NAPLEX, a simulation encompassing 100 previously utilized questions, offers candidates a realistic appraisal of proficiency. Administered in a home environment, this tool provides immediate feedback, enabling identification of persistent gaps and refinement of study strategies.
For students within academic institutions, the NAPLEX Advantage serves as an additional instrument. Proctored by schools and unavailable for individual purchase, this practice examination has demonstrated moderate predictive correlation with subsequent NAPLEX outcomes. Utilizing these diagnostic tools iteratively allows candidates to calibrate their study approach, ensuring alignment with the examination's scope and cognitive demands.
Mastery of Calculations and Clinical Reasoning
Pharmaceutical calculations and clinical reasoning represent areas of particular importance within NAPLEX preparation. Candidates must develop precision in dosage computations, compounding measurements, and pharmacokinetic assessments. Mastery in these domains requires repetitive practice and careful attention to units, conversions, and methodological steps, mitigating the risk of calculation errors under examination conditions.
Clinical reasoning encompasses evaluation of therapeutic appropriateness, monitoring parameters, and patient-specific factors. Engaging in scenario-based exercises, case discussions, and problem-solving tasks enhances the capacity to synthesize data, identify interventions, and anticipate outcomes. This integration of knowledge and reasoning mirrors the decision-making processes inherent in professional pharmacy practice.
Psychological and Cognitive Optimization
Effective preparation extends beyond content mastery to encompass cognitive and emotional optimization. The rigors of intensive study can induce mental fatigue, stress, and anxiety. Implementing strategies for psychological resilience—such as mindfulness, meditation, and structured breaks—ameliorates cognitive strain and enhances retention. Periodic self-assessment and reflective practice facilitate metacognitive awareness, enabling candidates to identify inefficient strategies and adjust study behaviors accordingly.
Sleep hygiene, nutrition, and physical activity further contribute to optimal cognitive function. Research underscores the interplay between physiological well-being and learning efficacy, highlighting the necessity of holistic preparation that integrates mental, emotional, and physical dimensions.
Resource Utilization and Study Materials
Candidates have access to a plethora of resources to support their NAPLEX preparation. These include textbooks, review guides, question banks, and institutional workshops. Strategic utilization of these materials is crucial. Over-reliance on singular sources may produce knowledge gaps, whereas integrative engagement across diverse resources fosters comprehensive mastery.
Collaborative study groups, mentorship, and peer discussion can augment individual preparation. These interactions enable the exchange of perspectives, clarification of ambiguities, and reinforcement of key concepts. Additionally, articulating knowledge in group settings enhances memory consolidation and facilitates the identification of nuanced clinical considerations.
Test Day Logistics and Familiarity
While content mastery is pivotal, familiarity with test-day procedures is equally consequential. The Candidate Bulletin provides exhaustive guidance regarding permissible items, identification requirements, scheduling, and break structures. Acquaintance with these logistics reduces anxiety, prevents procedural errors, and fosters confidence.
Candidates should also familiarize themselves with the testing environment, including seating arrangements, time allocation, and computer-based navigation. Simulating test conditions during practice sessions can acclimate candidates to the temporal pressures and interface, mitigating potential distractions and enhancing performance consistency.
Integrating Review and Retention Strategies
Consolidation of knowledge requires repeated review, spaced repetition, and active retrieval. Candidates are encouraged to revisit complex topics systematically, reinforcing retention and strengthening neural pathways associated with long-term memory. Utilizing techniques such as summarization, self-quizzing, and scenario application ensures that learned material is accessible during high-stakes examination conditions.
Integrating reflection periods into the study schedule allows candidates to assess mastery, recognize progress, and recalibrate focus areas. This iterative process of assessment, reflection, and targeted review embodies the principles of deliberate practice, which have been empirically demonstrated to enhance expertise acquisition and examination performance.
Practical Preparations Beyond Study
Preparation for the NAPLEX encompasses practical considerations beyond intellectual readiness. Ensuring logistical arrangements for transportation, identification, and contingency planning reduces extraneous stressors. Candidates should also verify examination appointments, review test-center protocols, and establish plans for unforeseen circumstances, such as illness or travel disruptions.
Financial preparation, including budgeting for examination fees, supplementary materials, and potential retakes, is a pragmatic aspect of readiness. Attending to these administrative elements ensures that cognitive resources remain dedicated to study and skill consolidation rather than unanticipated logistical challenges.
Cultivating Confidence and Composure
Confidence is a cumulative product of preparation, mastery, and experience. Regular practice, iterative assessment, and engagement with comprehensive study materials foster a sense of competence. Concurrently, cultivating composure through mindfulness, rehearsal of test-day routines, and adaptive coping strategies enables candidates to navigate the examination with equilibrium.
The psychological dimension of preparedness is particularly salient during high-stakes assessments. Candidates who maintain emotional regulation, focus, and resilience are better equipped to synthesize knowledge and execute decisions accurately under temporal and cognitive pressures.
Transitioning to Examination Execution
Upon completion of structured study and practice, candidates approach the NAPLEX with a foundation of knowledge, procedural familiarity, and psychological readiness. The study phase, characterized by iterative engagement with content, application of diagnostic tools, and cultivation of cognitive resilience, primes candidates for successful examination execution.
In tandem with conceptual mastery, attentiveness to procedural, logistical, and emotional dimensions ensures a holistic approach. By integrating these elements, candidates are not merely prepared to answer questions correctly but are equipped to navigate the examination environment with strategic insight, composure, and precision.
The culmination of deliberate study, practice examination engagement, and cognitive optimization constitutes the penultimate stage of NAPLEX readiness. Candidates emerge from this phase with reinforced knowledge, honed skills, and adaptive strategies for test-day performance. This integrated preparation cultivates the professional competence, analytical acumen, and procedural familiarity requisite for success. Having established both mastery and readiness, candidates are positioned to advance confidently to the subsequent phase: navigating the logistics of test day, ensuring compliance with procedural mandates, and executing their knowledge under authentic examination conditions.
Navigating the Examination Environment
As candidates approach the North American Pharmacist Licensure Examination (NAPLEX), familiarity with the examination environment becomes paramount. Beyond intellectual mastery, the ability to adapt to the procedural and environmental contingencies of test day influences performance. The examination setting requires attentiveness, composure, and strategic foresight. Acquaintance with logistics, timing, and permissible conduct mitigates extraneous stressors and allows cognitive resources to remain focused on question analysis and problem-solving.
The Candidate Bulletin provides exhaustive guidance on these dimensions, including identification requirements, prohibited items, and testing protocols. Candidates are advised to review these guidelines meticulously, internalizing procedural nuances and anticipating potential challenges. Simulated practice of test-day routines fosters habituation, ensuring that procedural elements do not disrupt performance.
Test-Day Logistics
Understanding the flow of the testing day is critical to minimizing cognitive distraction and enhancing efficiency. Candidates must verify arrival times, identify appropriate transportation routes, and ensure that all identification documentation aligns with the NABP e-Profile. Even minor discrepancies or delays can induce anxiety, undermining concentration and recall.
The testing environment also involves structured break periods. Candidates should plan hydration, nutrition, and restroom activities strategically, aligning these with cognitive pacing. Break periods are finite, and efficient utilization ensures that mental acuity remains optimized throughout the examination.
Cognitive Readiness and Mental Priming
Equally crucial is the cognitive and emotional priming undertaken immediately before the examination. Mental rehearsal, visualization, and mindfulness techniques enable candidates to transition into a state of heightened focus. By envisioning the procedural flow and anticipating challenging questions, candidates reinforce cognitive pathways and enhance decision-making fluidity.
Stress management strategies, such as controlled breathing, brief meditation, or progressive relaxation, mitigate the physiological manifestations of anxiety. These practices facilitate optimal neural functioning, supporting memory retrieval, analytical processing, and problem-solving under temporal constraints.
Strategic Question Analysis
The NAPLEX is designed to assess both knowledge and clinical reasoning. Question structures may involve patient scenarios, calculation-based queries, or conceptual problem-solving. Candidates are advised to approach each question methodically, parsing the stem for pertinent information and identifying key variables influencing the appropriate response.
Elimination techniques are particularly valuable in narrowing options for multiple-choice items. By systematically discarding implausible responses, candidates increase the probability of selecting correct answers and conserve cognitive resources. Attention to linguistic nuances, qualifiers, and context-specific cues enhances analytical accuracy and mitigates misinterpretation.
Time Management During the Examination
Effective time management is a critical determinant of examination success. The NAPLEX encompasses a finite number of questions within a specified temporal framework, necessitating a balance between speed and accuracy. Candidates should allocate time proportionally to question complexity, ensuring that challenging items do not disproportionately consume temporal resources.
Periodic monitoring of progress relative to elapsed time is recommended, facilitating adaptive pacing. Candidates may designate a final review window for uncertain questions, leveraging residual temporal capacity to maximize answer accuracy. Mastery of time allocation enhances confidence, reduces rushed decision-making, and mitigates cognitive fatigue.
Managing Cognitive Fatigue
Cognitive endurance is tested not only by content complexity but also by the duration of the examination. Candidates may experience mental fatigue, attentional drift, or diminished processing speed as the examination progresses. Strategies to counteract these effects include brief micro-pauses for controlled breathing, incremental hydration, and conscious mental refocusing.
Engaging metacognitive monitoring—assessing comprehension, attention, and response certainty—enables candidates to identify moments of cognitive decline and implement corrective strategies. By maintaining awareness of mental state and deploying adaptive interventions, candidates sustain performance consistency across the entire examination duration.
Navigating Calculation-Based Questions
Pharmaceutical calculations constitute a substantial component of the NAPLEX. Candidates must apply precise mathematical operations to compute dosages, concentrations, infusion rates, and pharmacokinetic parameters. Accuracy in these calculations is paramount, as errors may compromise clinical reasoning and patient safety interpretations within the examination context.
Structured approaches to calculation questions, including stepwise methodology, unit verification, and double-checking of results, enhance precision. Familiarity with common conversions, formulas, and approximations reduces cognitive load and permits efficient problem-solving under temporal pressure.
Integrating Clinical Decision-Making
Clinical decision-making questions assess the capacity to synthesize patient-specific data, therapeutic guidelines, and pharmacological principles. Candidates must consider factors such as comorbidities, drug interactions, monitoring parameters, and patient preferences. Scenario-based reasoning is central to this domain, requiring integration of theoretical knowledge with practical application.
Candidates are encouraged to adopt a systematic approach: identify the patient problem, enumerate potential interventions, evaluate risks and benefits, and select the most appropriate course of action. This structured reasoning ensures alignment with professional standards and promotes clarity in response selection.
Handling Uncertainty and Ambiguity
Certain NAPLEX items present ambiguity or require judgment in the context of incomplete information. Candidates must maintain composure, employ analytical reasoning, and avoid precipitous conclusions. Engaging with the question stem critically, referencing relevant principles, and considering clinical plausibility enhances decision-making accuracy.
Acceptance of uncertainty, coupled with methodical problem-solving, fosters resilience and adaptability. Candidates who navigate ambiguous items with measured reasoning are better equipped to optimize overall examination performance.
Post-Question Reflection and Adaptation
During the examination, brief reflective pauses following challenging questions can recalibrate cognitive focus. Candidates may internally review reasoning processes, verify computational steps, and ensure alignment with clinical rationale. This micro-reflection supports accuracy and reinforces confidence for subsequent items.
Adaptive strategies may include revisiting flagged questions if time permits, redistributing attention to high-yield content areas, and modulating cognitive effort based on perceived difficulty. Flexibility in approach allows candidates to optimize performance dynamically throughout the examination.
Environmental Acclimatization
Acclimatization to the physical and sensory environment of the testing center mitigates potential distractions. Candidates should arrive early, locate facilities, and orient themselves to seating, lighting, and auditory conditions. Familiarity with the interface of the computer-based testing system enhances comfort and reduces procedural errors.
Environmental awareness extends to personal ergonomics, including posture, seating position, and access to necessary materials. Optimizing these factors supports sustained concentration and minimizes physical discomfort that could detract from cognitive performance.
Integrating Exam-Day Nutrition and Hydration
Physiological optimization contributes to cognitive endurance. Candidates should consume balanced nutrition before testing, emphasizing complex carbohydrates, protein, and hydration to maintain stable energy levels. Avoidance of excessive caffeine or high-sugar foods mitigates potential fluctuations in alertness.
During scheduled breaks, strategic hydration and light, non-disruptive snacks can sustain mental acuity. Coordinating intake with testing intervals ensures minimal interference with examination tasks while maintaining physiological equilibrium.
Psychological Resilience Under Pressure
The psychological dimension of test-taking is profound. High-stakes assessment can evoke anxiety, self-doubt, or over-arousal, which may impair judgment and recall. Candidates who cultivate resilience through preparation, mental rehearsal, and adaptive coping are better positioned to sustain focus.
Positive self-talk, visualization of successful execution, and controlled breathing techniques mitigate stress responses. Candidates who maintain equanimity under pressure optimize the translation of preparation into accurate, confident responses.
Strategies for Test-Day Success
Success on the NAPLEX is the product of integrated preparation encompassing content mastery, procedural familiarity, and psychological readiness. Candidates who approach the examination with structured strategies for question analysis, time management, cognitive endurance, and emotional regulation optimize their performance potential.
By harmonizing intellectual, logistical, and physiological considerations, candidates navigate the examination environment with poise, precision, and strategic insight. This holistic approach ensures that high-stakes assessment reflects not only knowledge acquisition but also professional reasoning, adaptability, and resilience.
Transitioning to Post-Examination Phase
Having completed the examination with strategic execution, candidates transition to the final stage: awaiting and interpreting results. This phase, while less active, remains integral to the overall licensure process. Understanding result dissemination, implications for professional trajectory, and potential next steps fosters clarity and reduces anticipatory anxiety.
Post-examination reflection also allows candidates to consolidate lessons learned, reinforcing strengths and identifying areas for potential future development. The culmination of preparation, execution, and reflection embodies the comprehensive journey toward licensure and professional practice.
Understanding Examination Results
Upon completion of the North American Pharmacist Licensure Examination (NAPLEX), candidates enter the evaluative phase, which involves the processing and dissemination of results. This stage, while devoid of active study, is pivotal in determining the subsequent trajectory of licensure and professional development. Examination results reflect both cognitive mastery and applied clinical reasoning, providing an objective assessment of readiness for professional practice.
Results are typically communicated through the NABP e-Profile, where candidates can access performance indicators and overall pass status. The communication is structured to provide clarity and minimize ambiguity, yet it necessitates careful interpretation. Candidates should approach results analytically, understanding the implications for licensure eligibility and, if necessary, remedial planning.
Analyzing Performance Metrics
Beyond a binary pass or fail outcome, the NAPLEX report includes performance metrics across various content domains. This granularity allows candidates to identify strengths, weaknesses, and patterns of knowledge retention. By evaluating domain-specific performance, candidates can discern areas requiring reinforcement, whether for retake preparation or continued professional competency development.
Performance analysis also illuminates the efficacy of study strategies employed during preparation. Identifying areas of consistent difficulty may indicate the need for alternative learning methodologies or a more focused review of clinical scenarios, calculations, or regulatory concepts. This reflective approach supports continuous professional growth.
Addressing Unsuccessful Outcomes
In the event of an unsuccessful attempt, candidates must navigate the process of retake eligibility. NABP and state boards establish specific protocols governing retake applications, waiting periods, and documentation requirements. Awareness of these regulations is essential to avoid procedural delays and to plan a strategic approach for subsequent attempts.
Retake preparation emphasizes not only content review but also critical analysis of prior performance. Candidates are encouraged to revisit previously challenging areas, integrate new study strategies, and employ diagnostic practice examinations to assess improvement. Iterative cycles of practice, reflection, and targeted study enhance the likelihood of successful future outcomes.
Strategic Retake Planning
Effective retake planning begins with a detailed review of previous performance metrics. Candidates should identify content domains with lower proficiency, prioritize study resources, and allocate sufficient time for comprehensive review. Structured timelines and measurable milestones facilitate disciplined preparation and mitigate the risk of superficial or fragmented study.
Supplementary resources, such as question banks, scenario-based exercises, and institutional workshops, can augment retake readiness. Leveraging multiple modalities of learning—visual, auditory, and kinesthetic—enhances cognitive assimilation and retention, fostering a more robust understanding of complex pharmacological principles.
Psychological Adaptation to Retake Preparation
Retake preparation is as much a psychological endeavor as an intellectual one. Candidates must cultivate resilience, patience, and motivation to re-engage with rigorous study demands. Adaptive strategies, including goal setting, mindfulness, and structured reflection, support sustained engagement and mitigate potential demoralization.
Positive reframing—perceiving previous unsuccessful attempts as opportunities for refinement rather than failure—facilitates constructive engagement. Candidates who adopt growth-oriented perspectives maintain focus, leverage prior experience, and approach retake preparation with renewed strategic insight.
Maintaining Professional Competence During the Waiting Period
While awaiting examination results or preparing for a retake, candidates benefit from ongoing engagement with professional knowledge and practice. Continuous study, clinical observation, and review of contemporary pharmaceutical literature reinforce understanding and maintain proficiency.
Participation in experiential rotations, shadowing opportunities, or volunteer clinical activities supports the practical application of pharmacological principles. These activities enhance retention, bridge gaps between theoretical knowledge and clinical implementation, and sustain professional identity during transitional periods.
Continuing Education and Knowledge Reinforcement
Structured continuing education offers candidates a mechanism to reinforce knowledge and remain abreast of evolving pharmaceutical practices. Engaging with case studies, guidelines, and evidence-based literature cultivates analytical skills and contextual understanding. Candidates who integrate these practices maintain cognitive readiness and enhance clinical judgment, both for retake scenarios and future professional practice.
Furthermore, documenting learning experiences contributes to a portfolio of professional development, facilitating reflection and strategic identification of ongoing competency needs. This approach aligns with lifelong learning principles, ensuring sustained growth beyond the immediate examination context.
Preparing for Licensure Upon Passing
For candidates who achieve successful outcomes, attention transitions to procedural steps for formal licensure. These steps encompass verification of results with state boards, completion of ancillary documentation, and compliance with jurisdiction-specific requirements. Candidates should meticulously adhere to instructions, ensuring that licensure processes are executed without administrative impediments.
Successful navigation of this stage formalizes professional status, authorizing candidates to engage fully in the practice of pharmacy. Awareness of timelines, submission protocols, and required materials is critical to seamless licensure completion.
Integration of Clinical Competence
Licensure is not merely a formal credential but a confirmation of the ability to integrate knowledge into clinical practice. Candidates must synthesize pharmacotherapeutics, patient care principles, and regulatory guidelines to deliver evidence-based interventions. The NAPLEX serves as a benchmark of this integration, yet ongoing competence requires continuous engagement with clinical practice, reflection, and knowledge refinement.
Practical application encompasses patient counseling, medication therapy management, and interprofessional collaboration. Candidates transitioning from examination preparation to professional practice should cultivate adaptive reasoning, ethical judgment, and effective communication to navigate diverse clinical scenarios.
Reflective Practice and Continuous Improvement
Reflection is central to professional maturation. Candidates should evaluate the preparation process, identify strategies that yielded effective retention, and recognize areas where alternative approaches may enhance future learning. This metacognitive perspective supports both licensure success and long-term professional development.
Engagement with reflective practice also fosters ethical and patient-centered decision-making. By analyzing past clinical decisions, problem-solving approaches, and outcomes, practitioners refine judgment, reinforce accountability, and cultivate professional wisdom.
Mentorship and Professional Networking
Mentorship serves as a pivotal mechanism for both pre-licensure and post-licensure development. Experienced practitioners provide guidance on clinical reasoning, professional expectations, and career navigation. Candidates benefit from insights into effective study strategies, regulatory intricacies, and practical problem-solving approaches.
Professional networking extends beyond mentorship, encompassing engagement with colleagues, institutional leaders, and professional organizations. Such interactions cultivate knowledge exchange, collaboration, and exposure to evolving practice standards. Networking supports continuous learning and situates candidates within the broader professional community.
Ethical Considerations in Post-Examination Preparation
Ethical considerations remain integral throughout the transition from examination to practice. Candidates must uphold integrity in preparation, clinical reasoning, and documentation. Ethical reflection encourages adherence to professional standards, responsible patient care, and conscientious application of knowledge.
Engaging with ethical scenarios, case studies, and regulatory guidance reinforces the capacity for principled decision-making. This orientation ensures that technical competence is complemented by moral and professional responsibility, a hallmark of effective pharmacy practice.
Preparing for Future Professional Challenges
The post-examination period, whether awaiting results or transitioning to practice, offers opportunities to anticipate professional challenges. Candidates may explore emerging pharmaceutical technologies, regulatory developments, and shifts in healthcare delivery. Awareness of these dynamics enables adaptive competence, preparing practitioners to respond effectively to evolving professional demands.
Integrating knowledge of healthcare systems, interprofessional collaboration, and patient-centered approaches ensures readiness for multifaceted clinical responsibilities. Candidates who approach this period proactively cultivate resilience, versatility, and strategic insight.
Consolidating Knowledge Through Active Engagement
Maintaining proficiency requires active engagement with knowledge and practice. Candidates may undertake case analyses, engage in simulations, or participate in continuing education modules. This dynamic approach reinforces prior learning, enhances clinical judgment, and bridges the gap between theoretical understanding and applied practice.
Active engagement also nurtures cognitive flexibility, enabling candidates to adapt established principles to novel scenarios. This capacity is essential for both retake preparation and ongoing professional development, ensuring that competence extends beyond initial licensure achievement.
Holistic Professional Development
The post-examination phase exemplifies the integration of intellectual, practical, and ethical dimensions of pharmacy practice. Candidates cultivate competence not only through content mastery but also through reflection, mentorship, ethical engagement, and ongoing clinical experience. This holistic approach ensures that professional readiness is sustained, comprehensive, and adaptable to the complex realities of healthcare practice.
Transitioning Into Practice
Ultimately, the journey from examination preparation to licensure constitutes a continuum of growth. Candidates who navigate this process systematically, reflectively, and ethically emerge as practitioners equipped with both technical expertise and professional acumen. The transition into practice is facilitated by deliberate engagement with knowledge, attention to procedural requirements, and cultivation of adaptive skills.
By integrating the lessons of preparation, assessment, and reflection, candidates solidify a foundation for enduring professional competence. Licensure is a milestone, yet continuous learning, reflective practice, and active engagement with clinical challenges define the ongoing evolution of a capable and conscientious pharmacist.
Advancing Clinical Reasoning Post-NAPLEX
With the North American Pharmacist Licensure Examination behind them, new pharmacists enter a phase that demands the refinement of clinical reasoning and the practical application of knowledge acquired during training. The transition from examination preparation to real-world practice entails the integration of complex pharmacological concepts, patient-centered care, and interprofessional collaboration. Developing advanced clinical reasoning ensures that practitioners are capable of navigating multifaceted healthcare scenarios with discernment and precision.
Advanced reasoning begins with synthesizing pharmacotherapeutic principles within the context of individual patient variables. Considerations such as comorbidities, polypharmacy, pharmacogenomic implications, and patient preferences must be analyzed in tandem. This multidimensional evaluation cultivates nuanced decision-making and fosters patient outcomes that are both safe and effective.
Interpreting Complex Clinical Scenarios
Pharmacy practice increasingly involves intricate clinical scenarios where straightforward solutions are insufficient. Candidates must engage in meticulous assessment of laboratory data, medication histories, and therapeutic guidelines to formulate appropriate interventions. The ability to discern subtle indicators, anticipate potential complications, and adapt recommendations accordingly is crucial for competent practice.
Scenario-based exercises, simulations, and case studies reinforce this skill set. Engaging in reflective practice, where practitioners analyze previous interventions and outcomes, further consolidates reasoning abilities. Such reflective cycles enhance cognitive flexibility and prepare pharmacists to respond adeptly to unforeseen clinical challenges.
Interprofessional Collaboration
Effective patient care requires collaboration across healthcare disciplines. Pharmacists must communicate recommendations clearly with physicians, nurses, and other allied health professionals, advocating for evidence-based interventions while respecting diverse clinical perspectives. Interprofessional collaboration enhances patient safety, optimizes therapeutic outcomes, and fosters a culture of collective problem-solving.
Developing proficiency in this domain involves active listening, clarity of expression, and the ability to present a rationale for interventions grounded in pharmacological evidence. Engaging in collaborative practice models during training or post-licensure enriches competence and reinforces professional confidence.
Navigating Specialized Populations
Advanced practice often entails serving specialized patient populations, including pediatrics, geriatrics, and individuals with complex chronic conditions. Pharmacists must consider age-specific pharmacokinetics, comorbidity interactions, and adherence challenges when designing therapeutic regimens.
Attention to social determinants of health, cultural sensitivity, and patient education is critical. Tailoring communication strategies, counseling approaches, and monitoring plans to diverse populations ensures equity and effectiveness in pharmaceutical care. Candidates who cultivate these competencies elevate the standard of practice and reinforce the pharmacist's role as an integral healthcare provider.
Medication Therapy Management and Optimization
Post-NAPLEX practice emphasizes the strategic optimization of medication therapy. Pharmacists assess therapeutic efficacy, monitor adverse effects, and adjust regimens to maximize patient outcomes. This dynamic process requires continuous evaluation of pharmacokinetic parameters, drug interactions, and patient adherence factors.
Incorporating evidence-based guidelines, clinical trial data, and patient-specific considerations strengthens decision-making. Pharmacists are tasked with balancing therapeutic goals, minimizing risks, and anticipating potential complications, which collectively enhance the quality and safety of care delivered.
Maintaining Competence Through Continuing Education
The rapidly evolving landscape of pharmacotherapy necessitates ongoing learning. Continuing education (CE) programs, professional workshops, and peer-reviewed literature provide avenues for skill enhancement and knowledge expansion. Engagement with CE fosters lifelong learning, ensures alignment with contemporary practice standards, and supports maintenance of licensure requirements.
Candidates are encouraged to pursue targeted learning that addresses areas of emerging complexity, such as biologics, pharmacogenomics, and novel therapeutic modalities. This strategic approach ensures that professional competence remains adaptive and responsive to the dynamic healthcare environment.
Ethical and Professional Considerations
Ethical deliberation remains central to advanced practice. Pharmacists navigate decisions involving informed consent, patient autonomy, and allocation of limited resources. Reflective practice, case discussions, and engagement with ethical frameworks strengthen the capacity for principled decision-making.
Professional conduct encompasses accuracy in documentation, accountability in clinical recommendations, and adherence to regulatory standards. By integrating ethical and professional considerations into daily practice, pharmacists reinforce trust, reliability, and integrity within healthcare systems.
Leveraging Technology in Practice
Technological integration increasingly shapes pharmacy practice. Electronic health records, clinical decision support systems, and telepharmacy platforms augment clinical judgment and enhance patient care. Mastery of these tools enables pharmacists to access data efficiently, identify potential therapeutic issues, and communicate recommendations seamlessly with other healthcare providers.
Utilizing technology effectively requires both technical proficiency and analytical discernment. Pharmacists must interpret algorithmic suggestions critically, cross-referencing with clinical knowledge to ensure safe and individualized patient care.
Cultivating Leadership Skills
Beyond clinical competence, pharmacists are often called upon to assume leadership roles. Leadership encompasses guiding interprofessional teams, mentoring junior colleagues, and contributing to institutional policy development. Effective leadership fosters collaboration, promotes adherence to best practices, and enhances the quality of patient care.
Developing leadership skills involves active participation in committees, professional organizations, and quality improvement initiatives. By engaging strategically, pharmacists cultivate influence, communication acumen, and the capacity to drive systemic improvements in healthcare delivery.
Quality Improvement and Risk Management
Pharmacists play a central role in quality improvement initiatives, monitoring therapeutic outcomes, and identifying potential areas of risk. Systematic evaluation of processes, adverse events, and medication errors contributes to the development of safer, more effective healthcare systems.
Incorporating structured methodologies such as root cause analysis, failure mode and effects analysis, and performance metrics enables pharmacists to implement targeted interventions. This proactive approach not only enhances patient safety but also reinforces professional accountability and competence.
Research and Evidence-Based Practice
Engagement with research strengthens clinical reasoning and informs practice decisions. Pharmacists who participate in clinical studies, analyze outcomes data, or contribute to scholarly publications integrate evidence-based principles into routine care.
Critical appraisal skills, including evaluation of methodology, statistical interpretation, and contextual application, enable pharmacists to translate research findings into practical recommendations. This iterative process bridges theoretical knowledge and real-world implementation, ensuring that patient care remains current and scientifically grounded.
Mentorship and Teaching
Experienced pharmacists contribute to the profession through mentorship and teaching. Guiding students, residents, or junior colleagues reinforces knowledge, fosters reflective practice, and cultivates the next generation of competent practitioners.
Teaching also enhances the mentor’s own understanding, as explaining complex concepts necessitates clarity of thought and synthesis of information. Structured mentorship programs, preceptorship, and informal guidance all contribute to professional development and the perpetuation of best practices within pharmacy.
Building Resilience and Professional Identity
Advanced practice entails navigating complex, high-pressure environments. Resilience, adaptability, and reflective self-awareness are essential for sustaining professional performance and preventing burnout.
Developing resilience involves strategic self-care, peer support, and ongoing reflection on successes and challenges. Cultivating a strong professional identity reinforces motivation, ethical decision-making, and engagement with lifelong learning. This foundation supports sustained excellence in both clinical and organizational settings.
Preparing for Specialized Certifications
Many pharmacists pursue additional certifications to expand their expertise and the scope of practice. Specialty credentials, such as those in ambulatory care, oncology, or pharmacotherapy, require advanced knowledge, practical experience, and formal examination.
Strategic planning for these certifications involves targeted study, engagement with specialized clinical scenarios, and consistent practice of advanced decision-making. Pursuit of additional credentials not only enhances professional competence but also contributes to career progression and recognition within the healthcare community.
Integrating Feedback and Reflective Practice
Continuous improvement relies on feedback from colleagues, supervisors, and self-assessment. Reflective practice, incorporating both successes and challenges, enables pharmacists to refine clinical reasoning, enhance communication, and adapt strategies to complex scenarios.
Documenting reflections and interventions promotes metacognition and facilitates longitudinal tracking of growth. This disciplined approach reinforces mastery, accountability, and adaptability in evolving practice environments.
Enhancing Communication and Patient Education
Effective communication remains a cornerstone of pharmacy practice. Pharmacists educate patients about medication use, potential adverse effects, and lifestyle considerations. Tailoring communication to individual literacy levels, cultural context, and health beliefs ensures comprehension and adherence.
In addition to patient interaction, communication with healthcare providers requires clarity, conciseness, and evidence-based justification. Developing these skills supports collaborative care, reduces errors, and enhances therapeutic outcomes.
Post-NAPLEX, pharmacists enter a continuum of professional growth that encompasses advanced clinical reasoning, interprofessional collaboration, ethical decision-making, and lifelong learning. Mastery of these domains requires deliberate practice, reflective engagement, and proactive participation in evolving healthcare systems.
By integrating these elements, practitioners consolidate foundational knowledge acquired during preparation, enhance competence in complex scenarios, and cultivate resilience and adaptability. This stage marks a transition from licensure achievement to sustained professional excellence, reinforcing the pharmacist’s role as a critical contributor to patient care and healthcare innovation.
Sustaining Lifelong Excellence in Pharmacy
Completion of the North American Pharmacist Licensure Examination (NAPLEX) marks the formal beginning of a professional journey that extends far beyond initial licensure. Achieving competency on this high-stakes examination confirms foundational knowledge and clinical reasoning but does not signify the culmination of learning. Pharmacy, as a dynamic and ever-evolving discipline, requires practitioners to maintain curiosity, adaptability, and engagement with emerging trends throughout their careers.
Lifelong excellence in pharmacy involves the integration of continued education, reflective practice, mentorship, and leadership. Practitioners must remain vigilant in updating knowledge, adapting to evolving standards of care, and implementing innovations in therapeutics and patient management. The cultivation of intellectual agility ensures that pharmacists provide care that is both current and evidence-based.
Continuous Professional Development
Ongoing professional development is essential for maintaining licensure and enhancing clinical expertise. Participation in continuing education courses, certification programs, and workshops provides structured avenues for knowledge expansion. Engagement with peer-reviewed literature, clinical guidelines, and emerging research ensures that practice remains aligned with scientific advancements.
Structured professional development also fosters critical thinking, analytical reasoning, and adaptive decision-making. By continuously challenging assumptions, evaluating new evidence, and integrating novel strategies into practice, pharmacists sustain clinical competence and refine problem-solving skills.
Leadership and Advocacy in Pharmacy
Pharmacists are increasingly called upon to assume leadership roles within healthcare systems, policy-making bodies, and professional organizations. Effective leadership involves guiding interdisciplinary teams, implementing quality improvement initiatives, and influencing practice standards. By cultivating leadership competencies, pharmacists shape the delivery of care and contribute to organizational excellence.
Advocacy complements leadership, emphasizing the pharmacist’s role in advancing patient care, public health, and professional recognition. Engagement in policy discussions, professional associations, and community initiatives enables practitioners to influence regulations, expand access to care, and promote evidence-based practice. These activities reinforce the pharmacist’s role as a proactive agent of systemic improvement.
Embracing Emerging Trends and Technologies
The healthcare landscape is increasingly characterized by technological integration, precision medicine, and novel therapeutic modalities. Pharmacists must remain informed of these trends to provide optimal patient care. Telepharmacy, electronic health records, pharmacogenomic applications, and artificial intelligence tools are transforming practice, requiring proficiency in both technology and clinical judgment.
Adaptation to emerging trends demands ongoing learning, critical evaluation of new technologies, and integration into patient-centered care. Pharmacists who proactively engage with innovation enhance efficiency, improve safety, and optimize therapeutic outcomes.
Advanced Specialization and Credentialing
As practice evolves, many pharmacists pursue advanced credentials and specialization to expand scope and expertise. Specialty certifications in areas such as oncology, critical care, pharmacotherapy, and ambulatory care require targeted study, experiential practice, and formal assessment.
Preparation for advanced credentials involves deliberate planning, mastery of complex clinical scenarios, and consistent engagement with specialized knowledge. Achieving these credentials not only validates expertise but also enhances professional visibility, career opportunities, and the capacity to impact patient care meaningfully.
Mentorship and Professional Legacy
Experienced pharmacists serve as mentors, shaping the development of trainees, junior colleagues, and students. Mentorship encompasses guidance in clinical reasoning, professional ethics, and career planning. By fostering the growth of others, mentors reinforce their own knowledge, reflect on their practice, and contribute to the continuity of excellence within the profession.
Building a professional legacy involves imparting knowledge, advocating for high standards, and exemplifying ethical and patient-centered practice. Mentorship creates a cyclical model of professional development, ensuring that expertise, values, and standards are perpetuated across generations of practitioners.
Cultivating Resilience and Well-Being
Sustaining a long and impactful career in pharmacy requires resilience and attention to personal well-being. The demands of clinical practice, administrative responsibilities, and professional development can produce stress and cognitive fatigue. Strategies such as mindfulness, structured reflection, work-life balance, and peer support help maintain psychological resilience.
Resilient practitioners are better equipped to manage high-pressure scenarios, respond adaptively to challenges, and sustain quality of care. Attention to mental, physical, and emotional health reinforces professional longevity and ensures consistent performance in dynamic clinical environments.
Reflective Practice and Self-Assessment
Reflective practice enables pharmacists to evaluate their decisions, identify areas for improvement, and consolidate knowledge. Engaging in structured self-assessment, journaling clinical experiences, and analyzing patient outcomes fosters metacognitive awareness and professional growth.
Self-assessment also promotes adaptive learning, allowing practitioners to identify emerging gaps in knowledge, evaluate the effectiveness of interventions, and refine clinical strategies. This iterative approach enhances competence, confidence, and the ability to navigate complex healthcare scenarios.
Interdisciplinary Collaboration and Systems Thinking
Modern pharmacy practice operates within complex healthcare ecosystems, requiring pharmacists to engage collaboratively across disciplines. Interdisciplinary collaboration enhances patient care by integrating diverse perspectives, optimizing treatment plans, and reducing errors.
Systems thinking enables pharmacists to anticipate interactions within healthcare processes, identify inefficiencies, and implement improvements. By combining collaborative skills with systems-oriented analysis, pharmacists contribute meaningfully to organizational performance, patient safety, and therapeutic efficacy.
Patient-Centered Innovation
Pharmacists are uniquely positioned to innovate patient care practices. This may involve developing educational interventions, optimizing medication therapy management programs, or introducing technology-assisted adherence tools. Creativity and problem-solving within a patient-centered framework drive improvements in safety, efficacy, and accessibility.
Innovation also extends to process optimization, quality improvement, and operational efficiency. By integrating creative solutions with evidence-based practice, pharmacists enhance the value of services provided, reinforce professional credibility, and positively impact patient outcomes.
Navigating Regulatory and Legal Considerations
Advanced practice requires thorough knowledge of regulatory frameworks, licensure requirements, and legal obligations. Pharmacists must remain informed of jurisdictional regulations, evolving standards of practice, and compliance obligations to ensure safe and lawful delivery of care.
Proactive engagement with regulatory developments allows practitioners to anticipate changes, implement necessary adjustments, and advocate for policies that support optimal patient care. Legal and regulatory literacy complements clinical competence, safeguarding professional practice and reinforcing ethical responsibility.
Mentorship in Specialized Practice
Specialized pharmacists, such as those in oncology, critical care, or pharmacotherapy, play a critical role in mentoring peers and trainees within their niche. This mentorship fosters the dissemination of advanced knowledge, cultivates analytical skills, and ensures that specialized practice standards are maintained across institutions.
Structured mentorship programs in specialized practice enhance both the mentor’s and mentee’s capabilities. They create opportunities for reflective learning, collaborative problem-solving, and professional networking, reinforcing expertise and fostering a culture of continuous improvement.
Continuous Learning Through Research
Participation in research enhances clinical acumen and professional growth. Pharmacists engaged in clinical studies, pharmacoeconomic evaluations, or translational research deepen understanding of therapeutic principles and refine decision-making processes.
Research involvement encourages critical appraisal, methodological rigor, and evidence-based reasoning. Integrating research findings into practice ensures that patient care is informed by the latest advancements, supporting innovation, safety, and efficacy in pharmacotherapy.
Fostering Professional Communities
Active engagement in professional organizations cultivates networks for learning, collaboration, and advocacy. Participation in committees, conferences, and collaborative initiatives promotes knowledge exchange and strengthens professional identity.
Communities of practice support mentorship, provide resources for continued development, and facilitate the dissemination of best practices. By contributing to these networks, pharmacists enhance their impact, maintain engagement with the broader profession, and influence the evolution of practice standards.
Ethical Leadership and Advocacy
Ethical leadership involves guiding others in adherence to professional principles, promoting patient safety, and modeling integrity in decision-making. Pharmacists in leadership roles influence policy, mentor colleagues, and ensure that ethical considerations underpin organizational and clinical practices.
Advocacy efforts complement leadership by promoting access to care, public health initiatives, and evidence-based policy. Ethical and proactive engagement ensures that the pharmacist’s influence extends beyond individual patient interactions to systemic improvement and societal benefit.
Adapting to Global and Community Health Needs
Pharmacy practice increasingly encompasses global and community health considerations. Pharmacists must address disparities in access, cultural factors, and social determinants of health when designing interventions.
Understanding epidemiological trends, public health initiatives, and community-specific needs allows practitioners to implement targeted, effective interventions. Adapting practice to local and global health landscapes reinforces relevance, responsiveness, and the broader societal impact of pharmacy.
Lifelong Professional Identity and Growth
Sustaining excellence in pharmacy involves cultivating a professional identity that integrates knowledge, ethics, clinical judgment, and leadership. Lifelong growth is characterized by continuous learning, reflection, adaptation, and engagement with evolving practice landscapes.
By maintaining curiosity, embracing challenges, and committing to ongoing improvement, pharmacists solidify their role as essential healthcare providers. The foundation established during NAPLEX preparation evolves into a career defined by competence, adaptability, and dedication to patient-centered care.
Consolidating Competence Across the Professional Spectrum
The achievement of licensure marks only the beginning of a pharmacist’s professional journey. True competence extends far beyond initial qualification and evolves through a continuous process of learning, reflection, and adaptation. Pharmacists operate in a dynamic healthcare environment where patient needs, therapeutic innovations, and clinical expectations are constantly changing. To remain effective, practitioners must engage in lifelong professional development that integrates clinical expertise, ethical responsibility, and leadership.
Continuous learning ensures that pharmacists remain informed about emerging therapies, evolving disease management strategies, and technological advancements that influence patient care. Reflective practice deepens professional insight, allowing practitioners to evaluate their decisions, learn from experience, and enhance the quality of care delivered. Collaboration with interdisciplinary teams fosters shared expertise, promotes comprehensive patient management, and strengthens the healthcare system as a whole.
Research and innovation further underpin sustained excellence in pharmacy. By contributing to evidence-based practice, pharmacists drive improvements in medication safety, optimize treatment outcomes, and influence healthcare policy. Ethical practice and patient-centered care remain central pillars, ensuring that all professional actions align with compassion, integrity, and societal trust. Leadership—whether through mentorship, advocacy, or system-level engagement—empowers pharmacists to inspire change and elevate standards within the profession.
Ultimately, the path following NAPLEX success represents an ongoing commitment to personal and professional growth. Pharmacists who actively pursue education, mentorship, and collaboration cultivate enduring competence and resilience. Their influence extends beyond dispensing medications—they become innovators, educators, and advocates who shape the future of healthcare. Lifelong excellence in pharmacy, therefore, is not defined by examination results but by a deliberate and reflective pursuit of knowledge, ethics, and service. Through this holistic and evolving engagement, pharmacists continue to advance the quality and impact of healthcare delivery.
Conclusion
The journey toward becoming a licensed pharmacist, culminating in the North American Pharmacist Licensure Examination (NAPLEX), is both rigorous and transformative. From the initial stages of application and eligibility verification to the strategic preparation and execution of the examination, candidates navigate a multidimensional process that tests knowledge, critical reasoning, and practical application. Success in the NAPLEX reflects not only mastery of pharmacotherapeutic principles and calculations but also the capacity to integrate patient-centered care, clinical reasoning, and professional judgment under high-stakes conditions. Post-examination, the focus shifts toward interpreting results, addressing performance gaps, and transitioning into professional practice. Whether navigating retakes or advancing into licensure, candidates engage with continuous learning, reflective practice, and evidence-based application of knowledge. This phase underscores the importance of resilience, structured preparation, and ongoing engagement with emerging trends, guidelines, and best practices in pharmacy.
Long-term professional growth encompasses advanced clinical reasoning, interdisciplinary collaboration, and active participation in patient care innovation. Pharmacists cultivate expertise through mentorship, continuing education, research, and leadership, ensuring that their practice evolves alongside advancements in healthcare. Ethical conduct, systems thinking, and advocacy remain integral throughout, reinforcing the pharmacist’s role as a trusted, adaptable, and proactive healthcare provider. Ultimately, the NAPLEX represents a gateway to a career defined by lifelong learning, professional excellence, and meaningful impact on patient outcomes. By embracing deliberate preparation, reflective practice, and continuous professional development, pharmacists sustain competence, leadership, and innovation, embodying the highest standards of the profession and contributing to the advancement of healthcare systems globally.
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How often do you update the questions?
Testking strives to provide you with the latest questions in every exam pool. Therefore, updates in our exams/questions will depend on the changes provided by original vendors. We update our products as soon as we know of the change introduced, and have it confirmed by our team of experts.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.


