Certification: CHP
Certification Full Name: Certified HIPAA Professional
Certification Provider: HIPAA
Exam Code: HIO-201
Exam Name: Certified HIPAA Professional (CHP)
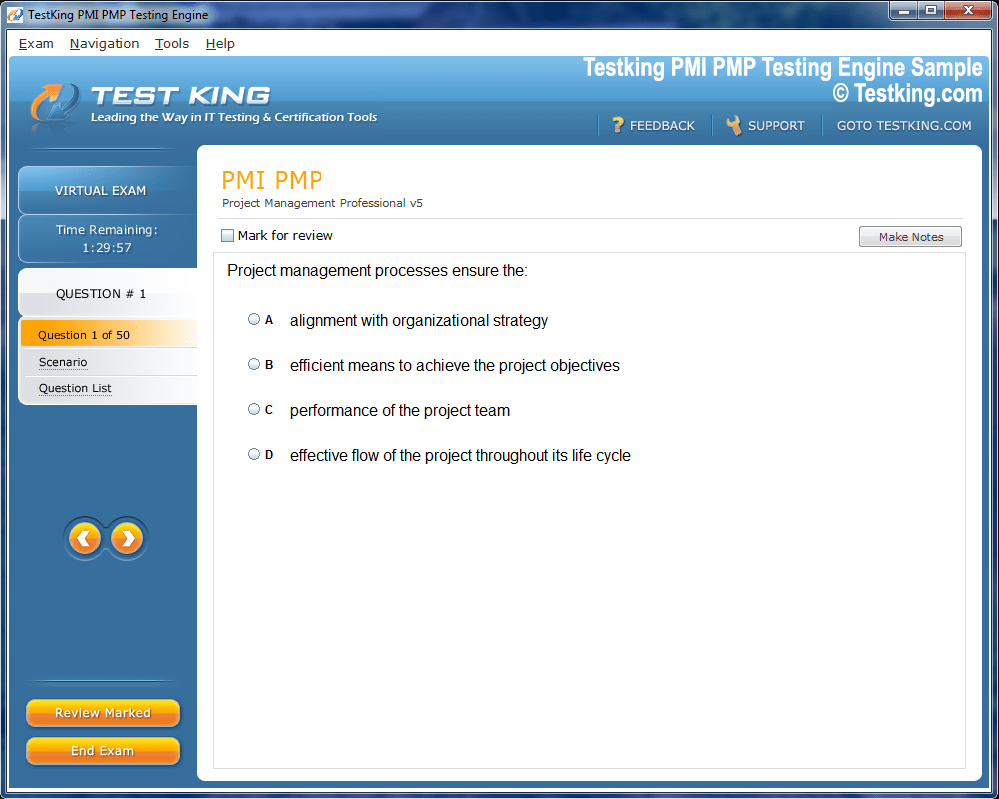
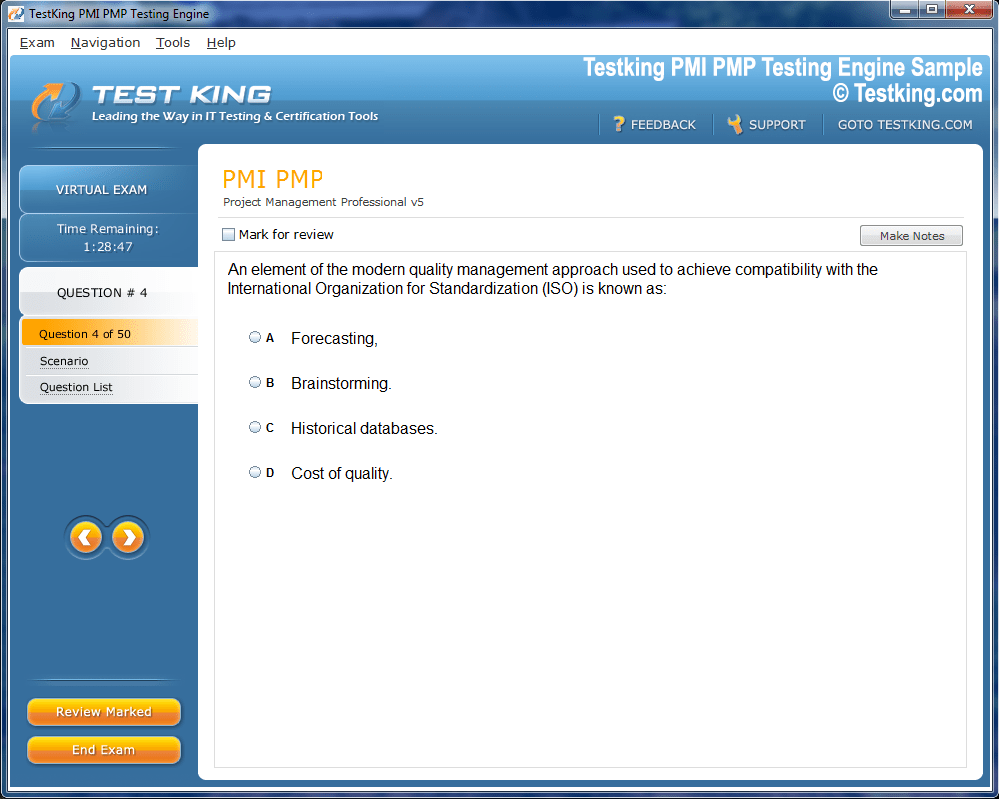
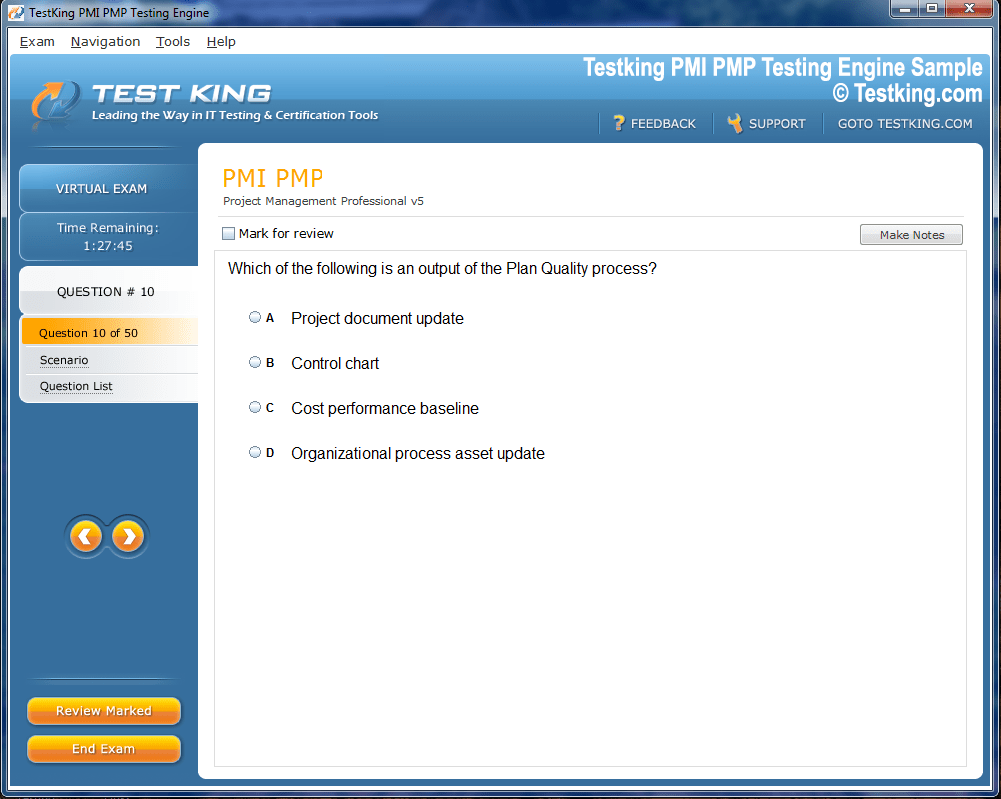
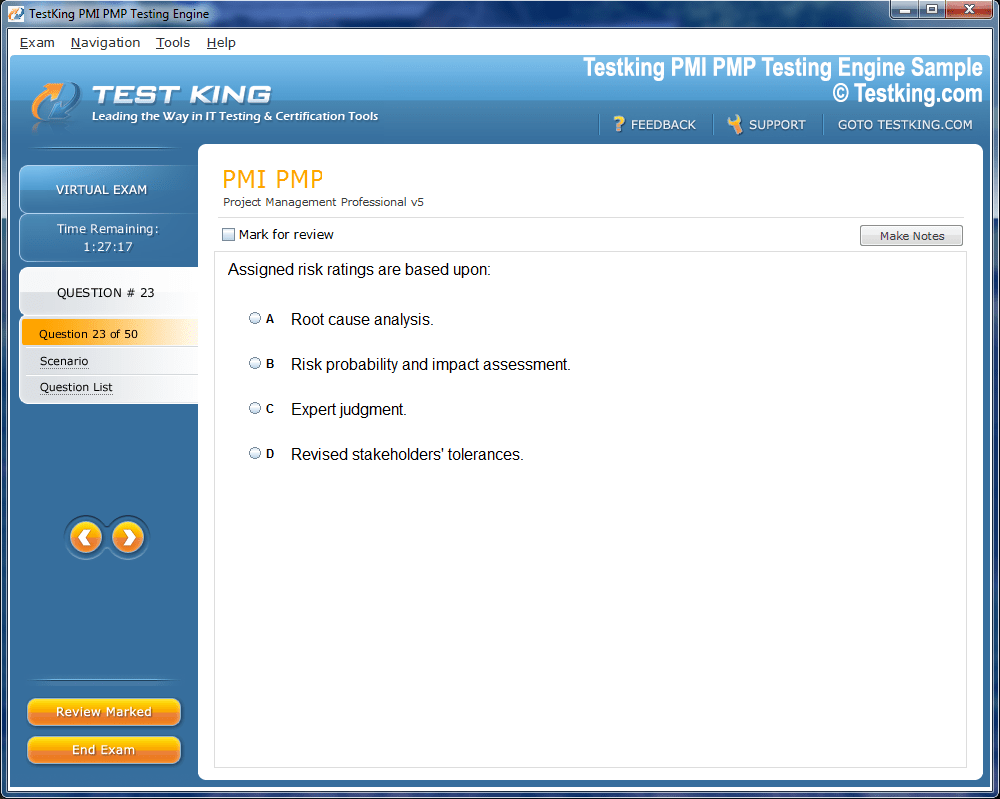
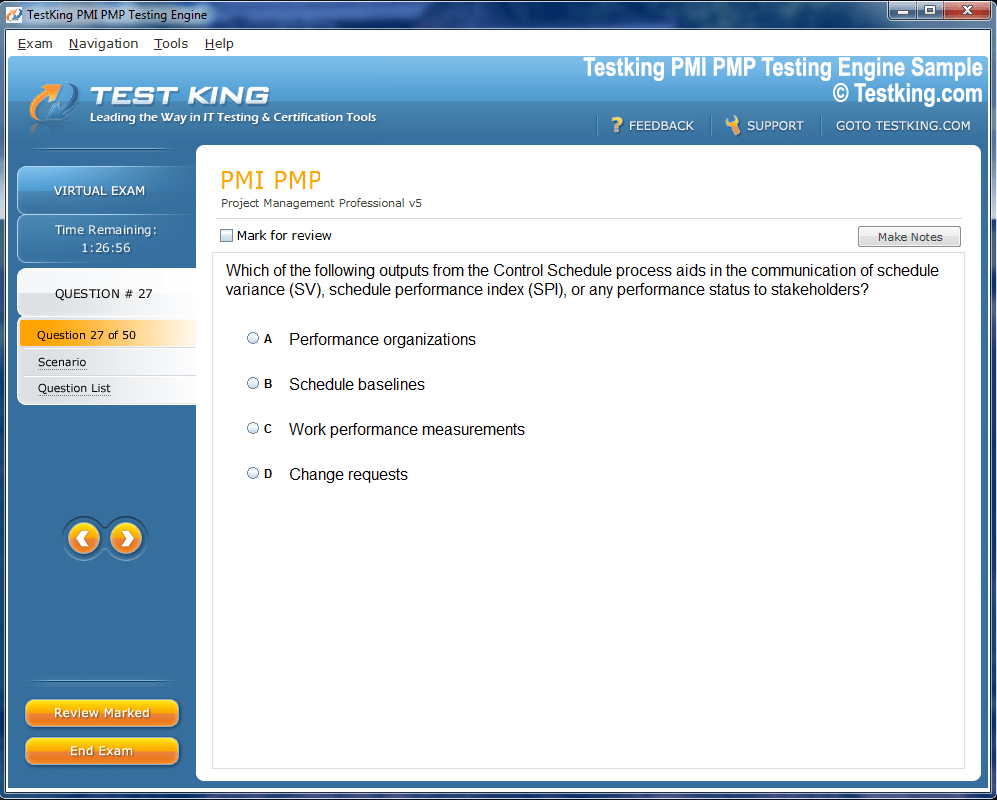
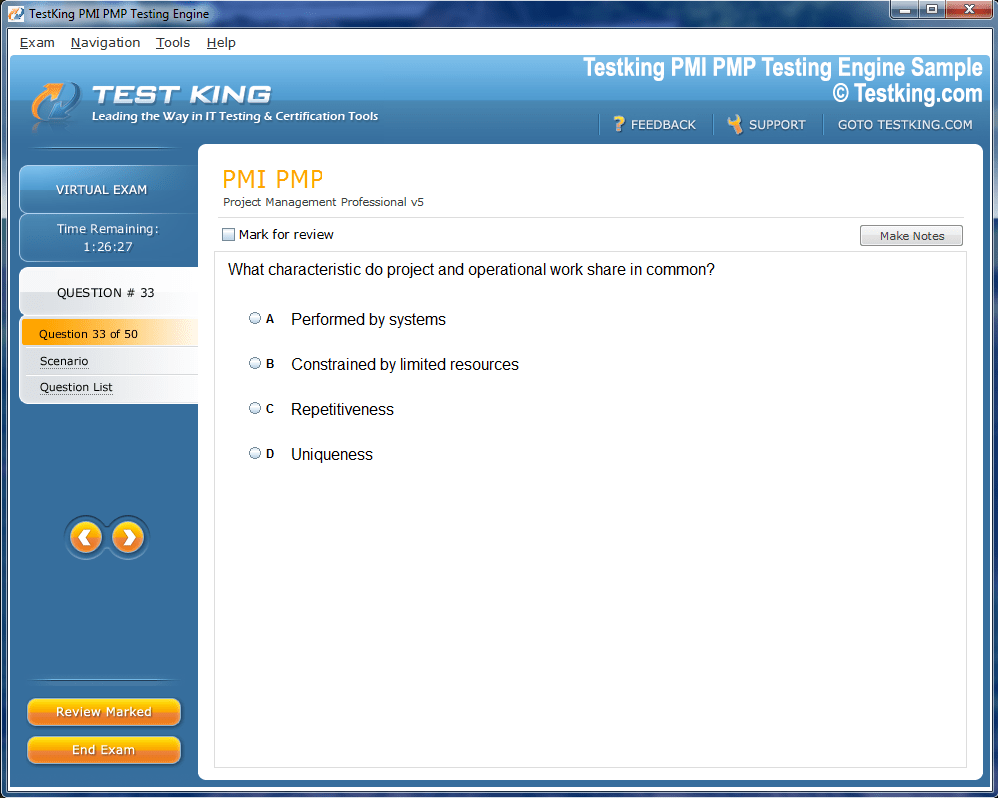
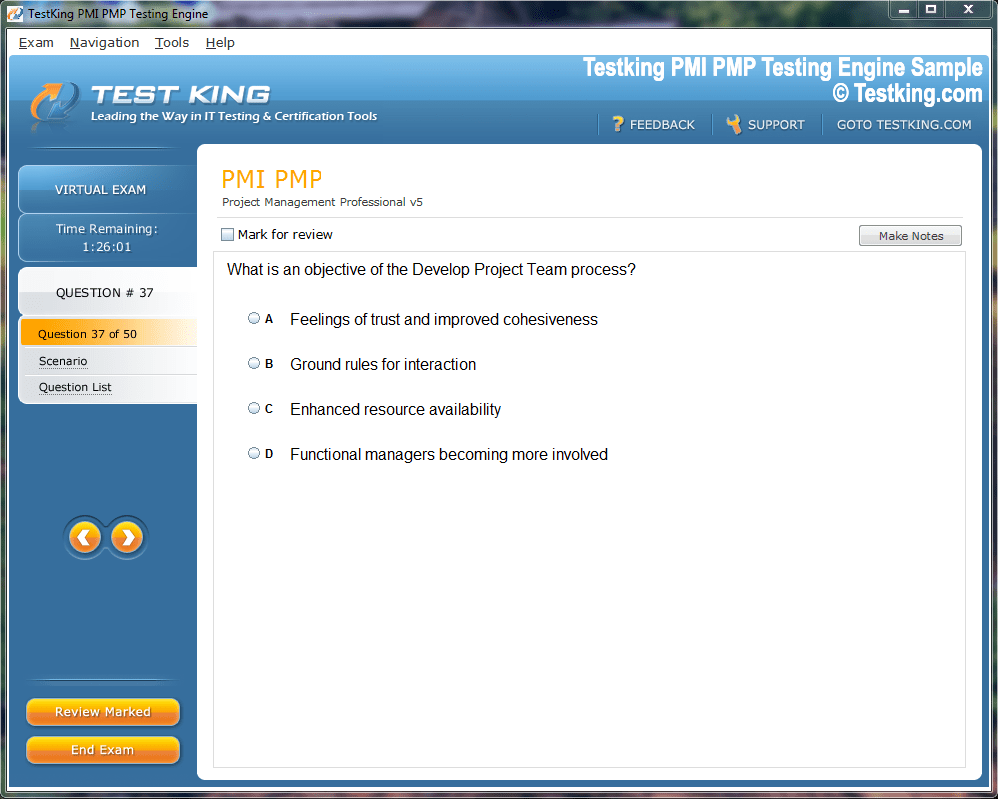
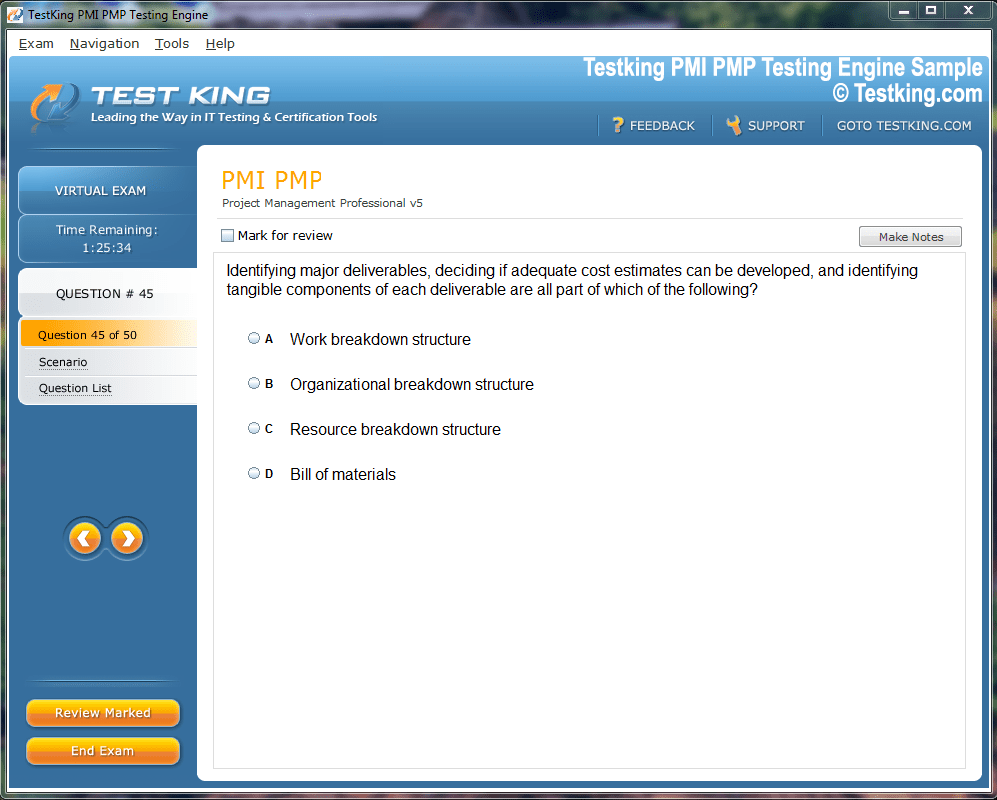
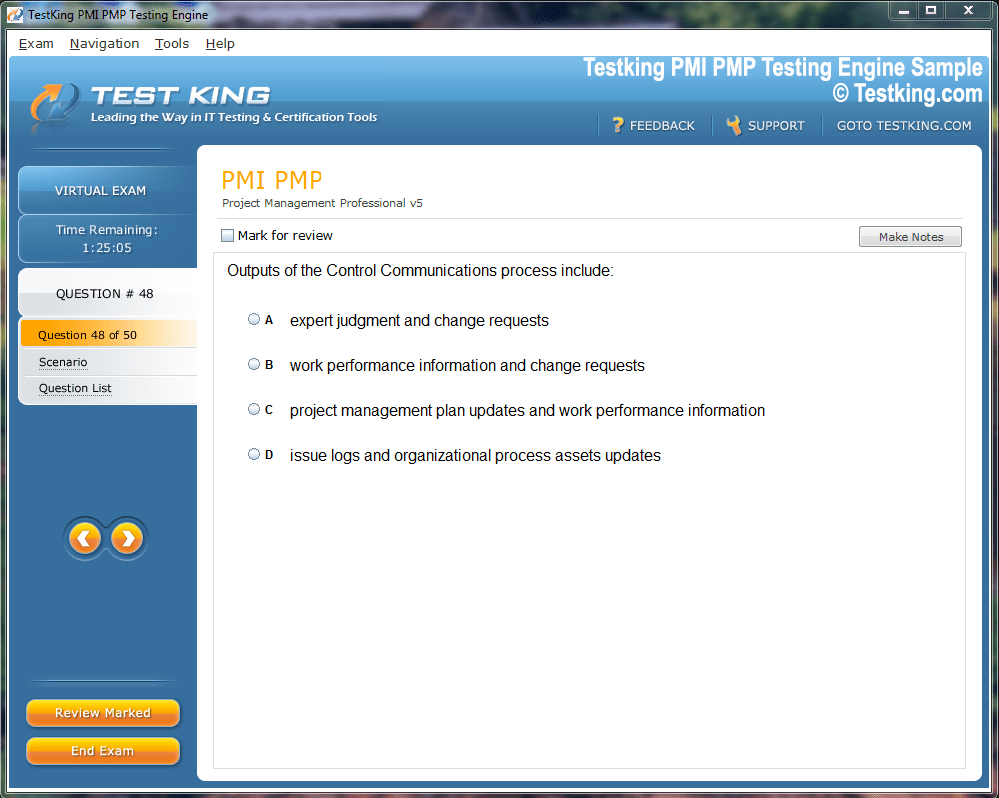
Product Screenshots

nop-1e =1
Mastering HIPAA HIO-201 to Protect Patient Data and Privacy
Healthcare information technology has evolved into a backbone of modern clinical and administrative practice, yet it also presents a formidable landscape of vulnerabilities. Medical facilities store immense volumes of protected health information, often abbreviated as PHI, which carries remarkable financial value in clandestine markets. Unlike many other types of stolen data, patient records contain a holistic view of an individual’s life, including demographic details, insurance credentials, contact numbers, prescription histories, and sometimes even biometric identifiers. This rich mixture of details can be exploited for identity theft, insurance fraud, or the creation of entirely fictitious identities.
The economic incentive for malicious actors to infiltrate hospital systems is therefore extremely high. At the same time, many institutions have not adequately fortified their defenses. Antiquated servers, irregular patching schedules, and unsupported operating systems linger across numerous healthcare networks. In addition, hospital personnel often lack comprehensive training in cybersecurity best practices, leaving them vulnerable to phishing campaigns, social engineering ploys, and careless handling of electronic devices.
Why Healthcare Is a Prime Target
While cyber-criminals seek easy prey across many industries, healthcare presents an alluring target due to its dependence on uninterrupted access to data. If patient records are unavailable, clinical operations grind to a halt, which in extreme cases can endanger lives. Because of this dependency, malicious groups wield ransomware with brutal efficiency in the sector. By encrypting an organization’s databases and demanding payment for decryption keys, criminals exploit the urgency of restoring access to medical files, imaging results, and scheduling platforms. Many institutions, fearing reputational damage and potential loss of life, feel compelled to comply with ransom demands despite the risks of further extortion.
Another factor amplifying healthcare’s vulnerability is the complexity of its information ecosystems. Hospitals and clinics typically rely on interconnected devices such as infusion pumps, diagnostic imaging machines, laboratory analyzers, and electronic health record platforms. Each connection multiplies the surface area available for exploitation. Furthermore, resource-constrained rural providers often lack the capital or skilled staff required to implement advanced security infrastructure. This imbalance between necessity and capability sustains healthcare as a fertile ground for attackers.
Legal Foundations of Patient Data Protection
Recognizing the sensitivity of medical records, the United States government passed the Health Insurance Portability and Accountability Act in 1996. This legislation, widely known as HIPAA, sought to establish privacy and security requirements for healthcare entities and their business associates. HIPAA articulated standards for safeguarding information, ensuring patient consent in data sharing, and defining penalties for breaches of confidentiality.
Although groundbreaking at the time, HIPAA was written during an era when fax machines and early desktop systems dominated healthcare communications. In contrast, today’s reality encompasses cloud computing, machine learning applications, interconnected mobile devices, and expansive telehealth networks. Because of this technological evolution, HIPAA itself cannot serve as a manual for the intricate technical safeguards required in the modern environment. To interpret its principles, professionals often align their practices with frameworks developed by institutions such as the National Institute of Standards and Technology. These frameworks provide prescriptive guidance for encryption, access control, auditing, and incident response, ensuring that organizations translate legislative mandates into practical strategies.
The Place of HIO-201 in Healthcare IT Training
Within this intricate security environment, training and examination play a pivotal role in cultivating skilled professionals. The exam code HIO-201 frequently emerges in discussions of healthcare IT education, representing a structured approach to assessing knowledge of privacy, compliance, and risk management. While HIPAA itself does not certify individuals, the existence of examinations like HIO-201 signals the need for specialized expertise. Through preparation for such assessments, candidates strengthen their grasp of regulatory obligations, technical countermeasures, and organizational processes that collectively sustain security.
The existence of exam-driven frameworks also ensures consistency. Without them, training might vary dramatically across institutions, leaving gaps in understanding. With HIO-201, professionals gain an opportunity to validate their competency, while organizations benefit from evidence that staff members possess a standardized level of proficiency. This dynamic contributes not only to regulatory adherence but also to heightened resilience against cyber threats.
The Role of Third-Party Auditors
Even though a universally recognized certification for HIPAA compliance does not exist, third-party auditing firms often conduct meticulous evaluations of healthcare providers. These evaluations examine whether an organization has established sound privacy practices, implemented adequate security measures, and trained its workforce effectively. Successful audits may result in documentation that affirms compliance efforts, which organizations can use to reassure patients and business partners.
Auditing serves as a preventative mechanism, exposing weaknesses before they escalate into violations. For example, auditors might discover that an organization has not updated its firewall rules in accordance with emerging attack vectors, or that encryption is inconsistently applied across mobile devices. By identifying such discrepancies, audits create opportunities for corrective action. In the broader regulatory landscape, the Health and Human Services Office for Civil Rights conducts its own evaluations, ensuring that organizations do not simply rely on internal declarations of compliance but are held accountable through external oversight.
Preparing for Compliance
Preparation for compliance involves a multifaceted strategy that integrates technological reinforcement with organizational culture. Employee education constitutes the cornerstone of this effort. Without comprehensive training, even the most sophisticated security infrastructure remains vulnerable to human error. Training programs should go beyond superficial awareness campaigns, embedding a culture of vigilance across every department. From nurses handling bedside devices to administrators managing cloud storage contracts, all staff must recognize their responsibilities in maintaining privacy.
Documentation plays a parallel role in compliance. Regulators and auditors require evidence that training occurs regularly and that policies are not simply theoretical. Organizations must therefore maintain detailed records of sessions, attendance, and curriculum content. Additionally, they must craft policies that outline disciplinary measures for noncompliance, demonstrating that privacy expectations are enforceable rather than symbolic.
The Appointment of Security Leadership
HIPAA mandates the appointment of both a security officer and a privacy officer within every covered entity and business associate. These roles may be filled by a single individual in smaller organizations or divided among specialists in larger facilities. Regardless of structure, the officer must possess both technical acumen and administrative insight. Their duties range from monitoring network security alerts to negotiating contracts with vendors that handle PHI.
The designation of such leadership ensures accountability. Without a responsible officer, privacy obligations can dissipate into an ambiguous cloud of shared duties, leaving gaps in enforcement. A named officer embodies organizational commitment, serving as a focal point for compliance initiatives, staff inquiries, and executive decision-making. Furthermore, officers often coordinate with external consultants, regulators, and technology providers, ensuring that the institution remains abreast of evolving threats and standards.
Comprehensive Risk Management
No compliance program can succeed without rigorous risk management. HIPAA requires organizations to conduct risk analyses, which function as thorough appraisals of vulnerabilities across networks, devices, applications, and communication channels. Such analyses are not one-time exercises but must be repeated periodically to account for changes in technology, personnel, and external threats.
The output of risk analysis is a mitigation plan, a document that not only catalogs vulnerabilities but also prescribes remedies. For instance, if a hospital identifies legacy systems running obsolete software, the mitigation plan might recommend phased replacement or isolation from sensitive networks. If an organization lacks multi-factor authentication for remote access, the plan should outline adoption steps, timelines, and accountability measures. Each action must be documented and auditable, ensuring that progress can be demonstrated during official reviews.
Risk management extends beyond the digital domain into physical security. Access controls for server rooms, surveillance systems for data centers, and procedures for handling portable devices all fall within the scope of a comprehensive plan. In addition, administrative safeguards—such as policies governing employee termination or vendor onboarding—also contribute to risk mitigation.
Crafting and Enforcing Policies
Policies function as the lifeblood of compliance. While laws provide broad mandates, organizational policies articulate the specific methods by which those mandates are achieved. For example, a policy might require that all emails containing PHI be automatically scanned by data loss prevention tools, or that portable drives used by staff be encrypted. Policies also define consequences for violations, thereby reinforcing seriousness.
The creation of policies is not a static endeavor. Because cyber threats evolve constantly, policies must undergo regular review. Emerging attack vectors, such as advanced ransomware strains or vulnerabilities in Internet of Things devices, necessitate policy adaptation. Enforcement mechanisms ensure that policies do not remain theoretical. Automated systems can detect anomalous behaviors, quarantine suspicious files, and alert administrators. Such mechanisms reduce reliance on individual vigilance and provide consistent protection across the organization.
The Importance of Internal Auditing
Internal audits represent another indispensable element of compliance. By conducting periodic evaluations, organizations gain visibility into the true state of their infrastructure. These audits should scrutinize both technical systems and procedural adherence. Technical assessments might reveal unpatched software, insecure wireless networks, or outdated encryption algorithms. Procedural reviews could uncover incomplete documentation of training or inconsistent enforcement of policies.
Importantly, internal audits should extend to third-party resources. Many healthcare institutions rely on cloud storage, external billing providers, or specialized telemedicine platforms. Each of these vendors interacts with PHI and, therefore, introduces potential vulnerabilities. An effective audit encompasses the entire ecosystem rather than confining attention to on-premise assets.
Engaging external auditors for certain reviews can also prove invaluable. Outsiders bring fresh perspectives, unclouded by organizational bias, and may identify weaknesses that internal staff overlook. Their findings enrich the organization’s understanding of its exposure and broaden the basis for corrective measures.
The Indispensable Role of Training in Safeguarding PHI
Among all defensive mechanisms available to healthcare institutions, training remains one of the most decisive. Technology alone cannot withstand the relentless ingenuity of cyber adversaries; it requires human vigilance to recognize threats before they metastasize. Healthcare professionals, from surgeons and pharmacists to administrative clerks, routinely interact with protected health information. If they lack the necessary awareness, even a sophisticated firewall or intrusion detection system can be circumvented by a single click on a fraudulent email.
Training programs must therefore be designed with precision and repetition. It is insufficient to host a single orientation session when employees are first hired. Threat landscapes evolve at a relentless pace, with new ransomware strains, phishing techniques, and malware variants appearing each month. To remain effective, training requires ongoing reinforcement, scenario-based exercises, and clear communication of policies.
When organizations align their training modules with frameworks like HIO-201, they gain a structured template for imparting knowledge. This ensures that all participants develop a consistent understanding of compliance expectations, security fundamentals, and the ethical responsibilities of handling PHI. Moreover, HIO-201-guided training emphasizes not only technical skills but also the organizational mindset necessary for sustainable compliance.
Crafting a Documented Training Framework
Documentation constitutes an integral part of the training process. Without verifiable records, organizations cannot demonstrate compliance during audits. Training logs must indicate who attended, when sessions were held, what curriculum was covered, and which instructors facilitated the instruction. Furthermore, policies should stipulate the frequency of refresher courses, with clear escalation procedures for employees who fail to complete their requirements.
Healthcare organizations also benefit from tailoring training to specific roles. A radiologist handling complex imaging equipment may require distinct instruction compared to a receptionist inputting demographic data into scheduling software. By customizing content, organizations avoid redundancy while ensuring that each employee understands the risks pertinent to their responsibilities.
Additionally, organizations should integrate rare but high-risk scenarios into their training. For example, staff members should know how to respond if they suspect a ransomware infection, if a laptop containing PHI is stolen, or if an unauthorized vendor attempts to solicit information. Such preparedness strengthens resilience and reduces panic when genuine incidents arise.
Appointing Security and Privacy Leadership
HIPAA requires the appointment of both a security officer and a privacy officer, roles that extend far beyond symbolic titles. These officers serve as custodians of compliance, orchestrating the intricate interplay of technology, people, and policies. Their presence provides accountability, ensuring that someone bears direct responsibility for safeguarding PHI.
In practice, these officers often face complex decisions. For instance, when a new vendor offers a cutting-edge telemedicine platform, the officers must evaluate not only its clinical benefits but also its security posture. They must review business associate agreements, determine whether the vendor encrypts data in transit and at rest, and ensure that contractual obligations align with regulatory requirements. Without this scrutiny, organizations risk entrusting sensitive data to insufficiently secured systems.
Leadership roles also extend into the cultural sphere. By embodying a visible commitment to compliance, security, and privacy, officers reinforce the importance of vigilance among staff. They deliver updates during staff meetings, distribute bulletins on emerging threats, and ensure that policies are not treated as bureaucratic formalities but as living instruments of protection.
The Symbiosis of Leadership and HIO-201
The exam code HIO-201 exemplifies the structured knowledge base required by security and privacy officers. Preparing for such an examination equips leaders with insights into both technical safeguards and administrative obligations. Through study and evaluation, officers reinforce their ability to interpret regulations, conduct risk analyses, and devise incident response strategies.
By anchoring leadership training in HIO-201 standards, organizations avoid the risk of inconsistency. Without such alignment, leaders might rely on fragmented understandings of compliance, shaped more by anecdotal experience than systematic knowledge. HIO-201 ensures that officers operate from a coherent framework, enhancing both confidence and competence in their roles.
Conducting Thorough Risk Analyses
Risk analysis serves as the cornerstone of HIPAA compliance. It compels organizations to evaluate the threats that loom over their networks, devices, and communications. Unlike superficial assessments, a comprehensive risk analysis scrutinizes every dimension of the healthcare environment, from clinical equipment to administrative databases.
An effective analysis begins with an inventory. Organizations must catalog every device, system, and application that interacts with PHI. This includes desktop computers, laptops, tablets, smartphones, servers, and cloud-based services. Each item represents a potential point of vulnerability, and without a full inventory, blind spots inevitably remain.
Once the inventory is complete, organizations must assess threats. These threats encompass both external attackers and internal risks, such as careless employees or malicious insiders. For each asset, organizations must evaluate the likelihood of exploitation and the potential impact on patient safety, financial stability, and regulatory compliance.
The final stage involves developing a mitigation plan. This plan must assign responsibilities, set timelines, and establish measurable goals. For example, if outdated medical devices lack encryption capabilities, the mitigation plan might recommend network segmentation, disabling of unnecessary services, or procurement of more secure replacements. Documentation ensures that the plan is actionable and auditable.
Extending Risk Management to Physical and Administrative Safeguards
Risk management is not confined to the digital realm. Physical safeguards are equally vital. Server rooms must be locked and monitored by surveillance cameras. Workstations must time out after periods of inactivity to prevent unauthorized access. Portable devices containing PHI must be encrypted and secured with strong authentication mechanisms.
Administrative safeguards also warrant attention. Policies must dictate how employees are granted and revoked access to systems. Vendor contracts must include stipulations for PHI protection. Procedures must guide the secure disposal of outdated equipment, ensuring that no residual data can be recovered by unauthorized individuals.
Through the lens of HIO-201, these safeguards are not ancillary but integral. The exam underscores the necessity of viewing compliance as an ecosystem in which technical, physical, and administrative measures converge to protect patient information.
Policy Development and Continuous Refinement
Policies represent the codification of organizational intent. They translate the abstract principles of HIPAA into tangible directives for daily practice. Yet policies must not remain stagnant. They must evolve in response to emerging threats, technological advancements, and organizational changes.
For instance, as healthcare institutions adopt telehealth platforms, policies must address secure video conferencing, data storage, and patient consent. As artificial intelligence tools analyze diagnostic images, policies must govern algorithmic transparency and safeguard the data sets used for training. Each innovation introduces new risks, and policies must adapt accordingly.
Enforcement is another critical dimension. Automated systems such as data loss prevention tools, intrusion detection systems, and anomaly detection algorithms provide a technological backbone for enforcement. However, disciplinary measures must also exist for human noncompliance. Without accountability, policies risk becoming symbolic gestures rather than effective safeguards.
Internal Auditing as a Compass of Compliance
Internal audits illuminate the truth of an organization’s security posture. Unlike external audits, which often occur sporadically, internal audits can be scheduled regularly to monitor progress. They reveal whether policies are followed, whether training is effective, and whether technical safeguards function as intended.
Audits should examine both obvious vulnerabilities and subtle oversights. Outdated antivirus software may represent an obvious risk, but subtler problems—such as inconsistent application of access controls or incomplete encryption of backup tapes—can prove equally devastating.
Healthcare organizations should also audit their relationships with external vendors. Business associates that handle PHI must be scrutinized with the same rigor as internal systems. Contracts should stipulate audit rights, enabling organizations to verify that vendors comply with agreed-upon standards.
An effective internal audit concludes with recommendations, action plans, and follow-up evaluations. This iterative process ensures continuous improvement rather than complacency.
The Human Factor in Sustaining Security
At the heart of compliance lies the human factor. Technology can be upgraded, policies can be rewritten, and audits can be conducted, but without the commitment of people, all these measures falter. Employees must internalize the principle that protecting PHI is synonymous with protecting patients.
Organizations should therefore cultivate a culture of accountability. Leadership must communicate that security is not optional but essential. Celebrating compliance successes, sharing stories of thwarted attacks, and recognizing staff who demonstrate vigilance reinforce positive behavior.
The cultural transformation does not occur overnight. It requires persistence, clear leadership, and continual reinforcement. Yet once embedded, it provides a formidable defense that technology alone cannot replicate.
The Centrality of Security Policies in Healthcare
Security policies in healthcare are not superficial documents to be archived in filing cabinets. They are dynamic blueprints guiding every interaction with protected health information. In the absence of clearly articulated policies, healthcare professionals may rely on inconsistent habits or personal judgment, creating fertile ground for errors and breaches. Policies must therefore provide explicit instructions, leaving little room for ambiguity.
At their best, policies establish an organizational ethos of responsibility. They remind staff that confidentiality is not optional but fundamental to the trust patients place in medical institutions. Patients expect that their most intimate medical details—diagnoses, treatment regimens, financial identifiers—will remain shielded from unauthorized eyes. A single lapse can erode that trust irreparably. Thus, robust policies are as vital to patient care as diagnostic expertise or surgical precision.
Aligning Policies with Contemporary Threats
Healthcare policies must be adaptive, reflecting the relentless transformation of digital landscapes. Twenty years ago, few institutions could have anticipated the proliferation of cloud-based medical applications, wearable health monitors, or virtual consultations. Today, these technologies define modern healthcare delivery. Without corresponding policies, institutions risk navigating uncharted waters without a compass.
For example, telemedicine requires explicit policies addressing secure video transmission, patient consent for digital communications, and the proper storage of virtual session records. Similarly, the rise of wearable devices necessitates guidelines for integrating third-party data into electronic health records while safeguarding patient privacy. Artificial intelligence introduces further complexities, demanding policies on transparency, data provenance, and algorithmic accountability.
When constructed with foresight, policies serve as adaptable frameworks rather than brittle mandates. They guide organizations through new challenges without requiring complete reinvention each time an innovation arises.
Enforcement Through Technical Mechanisms
While written policies establish expectations, enforcement mechanisms transform those expectations into reality. Automated systems play an essential role in this process. Data loss prevention tools can scan outgoing communications for sensitive information, quarantining suspicious messages before they leave the network. Intrusion detection systems can flag unusual patterns of activity, such as a user downloading vast amounts of data outside of normal working hours.
In addition, access control systems enforce the principle of least privilege. Employees should access only the data necessary for their roles. A billing clerk, for example, requires access to insurance identifiers but not detailed clinical notes. Technical enforcement prevents inadvertent or malicious overreach by limiting exposure to information.
Encryption further strengthens enforcement. By encrypting PHI both in transit and at rest, organizations render stolen data unreadable to unauthorized actors. Even if adversaries penetrate firewalls or intercept transmissions, encryption ensures that the data remains unintelligible without the correct decryption keys.
Administrative Enforcement and Accountability
Technical mechanisms must be accompanied by administrative enforcement. Policies should specify disciplinary measures for noncompliance, ranging from retraining to suspension or termination. Without such accountability, employees may dismiss policies as mere formality. When disciplinary consequences are consistently applied, staff recognize that compliance is non-negotiable.
Administrative enforcement also requires transparency. Employees must understand what is expected of them, what constitutes a violation, and how violations will be addressed. Clear communication fosters fairness and discourages the perception of arbitrary punishment. In addition, organizations should establish anonymous reporting mechanisms, allowing employees to disclose potential violations without fear of reprisal.
Continuous Review and Evolution of Policies
Static policies quickly become obsolete in an environment characterized by ceaseless innovation and emerging threats. Continuous review is therefore essential. Organizations should establish a regular schedule for policy evaluation, such as quarterly or biannual reviews. These evaluations must incorporate insights from internal audits, regulatory updates, and evolving industry standards.
During reviews, organizations should solicit input from diverse stakeholders. Clinicians, administrators, IT specialists, and compliance officers each interact with PHI differently. By incorporating their perspectives, organizations craft policies that are both practical and comprehensive. For instance, a nurse may highlight workflow inefficiencies caused by overly restrictive access controls, while an IT specialist may emphasize the need for stronger encryption protocols.
Through iterative refinement, policies evolve into living documents that balance security, usability, and compliance.
The Role of HIO-201 in Policy Frameworks
The exam code HIO-201 underscores the importance of structured policy frameworks within healthcare organizations. Preparation for this examination immerses professionals in the intricacies of regulatory requirements, technical safeguards, and administrative procedures. As a result, individuals trained under HIO-201 standards are well-positioned to craft, enforce, and evaluate policies that withstand scrutiny.
Furthermore, HIO-201 highlights the interconnectedness of technical, administrative, and physical safeguards. Policies are not siloed but integrated, ensuring that every domain of security aligns with overarching compliance objectives. By embedding HIO-201 principles into policy development, organizations foster coherence and resilience across their security infrastructure.
Internal Audits as Catalysts for Policy Effectiveness
Policies gain credibility only when validated through internal audits. Without verification, organizations cannot determine whether policies are genuinely implemented or merely aspirational. Internal audits function as diagnostic instruments, probing for weaknesses in both policy design and execution.
For example, an audit might reveal that while a policy mandates encryption of portable devices, several laptops in circulation remain unencrypted. Alternatively, an audit may uncover inconsistent training records, suggesting that not all employees have received the mandated instruction. These discoveries enable organizations to recalibrate their policies and address deficiencies before they escalate into breaches.
Internal audits also foster accountability. When employees know that compliance will be regularly assessed, they are more likely to adhere to established procedures. In this way, audits reinforce the seriousness of organizational commitments.
Auditing the Extended Ecosystem
Healthcare organizations seldom operate in isolation. They collaborate with insurers, laboratories, telehealth vendors, cloud providers, and billing companies. Each partnership introduces new avenues of vulnerability. Internal audits must therefore extend beyond the boundaries of the organization to encompass this extended ecosystem.
Business associate agreements establish the foundation for such oversight, obligating partners to comply with HIPAA requirements. Yet agreements alone are insufficient. Organizations must exercise audit rights to verify compliance. This may involve reviewing vendor security certifications, requesting documentation of training programs, or even conducting on-site inspections.
By auditing their partners, organizations ensure that security is not compromised by weak links in the chain of data stewardship. The exam code HIO-201 emphasizes this principle, reminding professionals that compliance is a collective responsibility extending across the healthcare continuum.
The Interplay of Technology and Human Factors
Even the most sophisticated technologies cannot substitute for human discernment. Employees remain the first line of defense against many forms of cyberattack. A vigilant nurse who questions an unusual request for patient information may thwart an attempted breach. Conversely, a distracted administrator who clicks on a malicious attachment may inadvertently unleash a ransomware infection.
Recognizing this interplay, organizations must design policies and training programs that complement technological safeguards. For example, while spam filters reduce the volume of phishing emails reaching employees, training ensures that staff can recognize and report the few that slip through. Similarly, while encryption protects data in transit, staff awareness prevents sensitive information from being transmitted through insecure channels in the first place.
By harmonizing human vigilance with technological safeguards, organizations achieve a layered defense that is more robust than either element alone.
Embedding Compliance in Organizational Culture
For compliance to endure, it must be woven into the fabric of organizational culture. Employees should perceive security not as an external imposition but as a natural extension of their professional responsibilities. This cultural embedding requires persistent leadership, visible commitment, and reinforcement at every level.
Leaders can cultivate this culture by consistently articulating the importance of privacy in patient care. They should highlight not only the regulatory consequences of breaches but also the ethical imperative to protect patient dignity. By framing compliance as an act of respect rather than a bureaucratic obligation, leaders inspire genuine commitment.
Cultural reinforcement also requires recognition. When employees demonstrate vigilance—such as reporting a suspicious email or identifying a policy gap—they should be acknowledged and commended. Such recognition signals that compliance is valued, fostering a positive feedback loop that encourages further engagement.
Preparing for the Unexpected
Even with robust policies, audits, and cultural commitment, breaches remain possible. No system is impervious to every conceivable threat. Organizations must therefore prepare for the unexpected through incident response planning.
An effective incident response plan outlines the steps to be taken when a breach occurs. It assigns responsibilities, establishes communication protocols, and defines escalation procedures. For example, if ransomware is detected, the plan should specify who will isolate infected systems, who will notify regulators, and how patient care will be maintained during the disruption.
Incident response planning transforms chaos into coordination. It ensures that organizations can act swiftly, limiting damage and restoring operations. Regular drills, much like fire drills, reinforce preparedness and instill confidence among staff.
The Ethical Imperative of Policy Implementation
While much discussion of compliance revolves around regulatory mandates and technical safeguards, it is important to remember the ethical dimension. Patients entrust healthcare providers with their most sensitive information, often at moments of vulnerability. To betray that trust is not merely a legal violation but a moral failing.
Security policies, therefore, serve as instruments of ethical stewardship. They codify the organization’s commitment to respecting patient dignity. By implementing, enforcing, and refining these policies, healthcare institutions honor the trust that patients extend to them.
The exam code HIO-201 reinforces this ethical dimension by embedding privacy and security within the professional identity of healthcare IT specialists. It reminds practitioners that compliance is not only about avoiding penalties but about safeguarding humanity’s most intimate data.
The Necessity of Continuous Auditing in Healthcare IT
Auditing within healthcare organizations cannot be reduced to a sporadic formality. It is a rigorous and recurring process that anchors compliance in reality. Without systematic auditing, policies may exist in theory while failing in practice. The dynamic nature of cyber threats ensures that yesterday’s solutions may be inadequate tomorrow. Only through continuous auditing can institutions ensure that protective measures remain effective in a world where adversaries adapt quickly.
Healthcare facilities must treat audits as an ongoing cycle rather than isolated events. Each round of evaluation generates findings, which should lead to corrective actions, followed by reassessment. This iterative model mirrors clinical practice, where diagnosis, treatment, and monitoring form an unbroken chain. By embedding audits into routine operations, organizations foster resilience that evolves with emerging risks.
Dimensions of Internal Audits
An internal audit extends beyond a checklist of security settings. It encompasses a holistic examination of technical, administrative, and physical safeguards. On the technical side, auditors may verify the integrity of firewalls, encryption systems, and intrusion detection tools. They may test whether employees’ access privileges align with their job roles, or whether outdated devices expose vulnerabilities.
Administrative audits scrutinize processes. Are training programs documented with sufficient detail? Do business associate agreements meet regulatory standards? Are policies enforced consistently across departments?
Physical audits ensure that tangible spaces remain secure. Server rooms must be restricted, portable devices must be locked when not in use, and paper records must be stored or destroyed according to established procedures. Each domain interlocks with the others, forming a comprehensive security posture.
The Ripple Effect of Vendor Auditing
Healthcare organizations rely heavily on external partners, from billing processors to telehealth platforms. Each of these business associates represents a potential vector for compromise. A single weak link can undermine even the most sophisticated internal defenses.
Vendor auditing must therefore be integral to compliance. Organizations should demand transparency from their partners, requesting documentation of training programs, encryption practices, and incident response strategies. In some cases, organizations may exercise contractual rights to perform on-site inspections or third-party evaluations.
The exam code HIO-201 emphasizes this ecosystemic perspective, reminding professionals that compliance does not stop at the walls of the hospital. It extends outward into a constellation of collaborators, all of whom must uphold the same standards of privacy and security.
Learning From Audit Findings
Audit findings are not simply lists of deficiencies; they are catalysts for transformation. When auditors identify vulnerabilities, organizations must respond with deliberate action. This may involve revising policies, retraining employees, or investing in new technologies. Importantly, responses must be documented, demonstrating not only that weaknesses were discovered but that they were addressed.
Findings also provide insight into systemic issues. If multiple audits reveal recurring lapses in encryption practices, the problem may not lie with individual employees but with the adequacy of training programs or the usability of encryption tools. By interpreting findings with nuance, organizations can address root causes rather than superficial symptoms.
The Role of External Auditors
While internal audits cultivate self-awareness, external audits introduce objectivity. Outsiders approach systems without preconceived assumptions, allowing them to notice vulnerabilities that internal staff may overlook. External auditors often possess specialized expertise, bringing knowledge of industry best practices and emerging attack vectors.
Collaboration between internal and external auditors strengthens compliance. Internal teams ensure continuity and familiarity with the organization’s systems, while external experts provide fresh perspectives and technical depth. Together, they construct a fuller picture of security posture.
Embedding Auditing Into Culture
Auditing should not be perceived as an intrusion or punishment. Instead, it must be embedded into the organizational culture as a mechanism of continuous improvement. When employees view audits as opportunities for learning, they are more likely to engage constructively. Leaders play a crucial role in shaping this perception by framing audits as pathways to excellence rather than as disciplinary tools.
Celebrating improvements identified through audits reinforces positivity. For example, when a department demonstrates significant progress in encryption compliance, leadership should acknowledge and commend the effort. Such recognition transforms auditing into a source of pride rather than apprehension.
Continuous Improvement as a Compliance Imperative
Compliance is not a static achievement but a dynamic pursuit. Continuous improvement ensures that organizations adapt to shifting regulations, technologies, and threats. This process involves revisiting every facet of compliance—training, policies, risk management, and technical safeguards—with an eye toward refinement.
Continuous improvement also requires humility. Organizations must accept that perfection is unattainable and that vulnerabilities will always exist. Rather than seeking finality, they must cultivate agility, ready to respond to new challenges with speed and precision.
Through continuous improvement, healthcare institutions evolve in tandem with the environment they inhabit, ensuring that their defenses remain relevant and robust.
Integrating HIO-201 Into Continuous Improvement
The exam code HIO-201 provides a structured framework for continuous improvement. It outlines the knowledge areas and competencies necessary for effective compliance, guiding professionals as they refine their practices. Preparation for the examination encourages regular review of policies, reinforcement of training, and evaluation of safeguards.
By aligning continuous improvement efforts with HIO-201, organizations ensure consistency and comprehensiveness. Rather than addressing issues in a fragmented manner, they pursue a unified strategy that encompasses all dimensions of compliance. This alignment also supports professional development, equipping staff with recognized expertise that strengthens organizational credibility.
Incident Response as a Measure of Preparedness
Continuous improvement must include incident response planning. Even with vigilant auditing and robust safeguards, breaches remain a possibility. An organization’s true resilience emerges not in the absence of incidents but in the effectiveness of its response.
An incident response plan should define roles, responsibilities, and escalation pathways. It should establish protocols for communication with regulators, patients, and the public. It should also include mechanisms for preserving evidence, enabling forensic analysis that informs future defenses.
Regular drills are essential to ensuring preparedness. Just as fire drills train occupants to respond calmly to emergencies, incident response drills prepare staff to act decisively during cyber crises. These exercises transform theoretical plans into practiced routines, minimizing hesitation when time is of the essence.
Documentation as the Backbone of Compliance
Documentation sustains every dimension of compliance. It provides tangible proof that training occurred, that policies exist, that audits were conducted, and that incidents were addressed. Without documentation, organizations cannot demonstrate their efforts to regulators or auditors, leaving them vulnerable to penalties even if substantive measures are in place.
Effective documentation must be comprehensive yet accessible. Overly complex records may obscure important details, while oversimplified documentation may omit crucial evidence. Organizations should strive for balance, ensuring that records are detailed enough to withstand scrutiny while remaining clear enough to guide practice.
The discipline of HIO-201 underscores this necessity. Professionals trained in its framework recognize that documentation is not administrative trivia but a critical defense mechanism.
Bridging the Gap Between Technology and Practice
Audits and continuous improvement highlight a recurring challenge: the gap between technology and practice. An organization may invest in advanced encryption software, but if employees find it cumbersome, they may seek workarounds that undermine its effectiveness. Similarly, policies may mandate complex passwords, but if systems lack user-friendly password management tools, compliance may falter.
Bridging this gap requires empathy and collaboration. IT specialists must listen to the concerns of clinicians, whose primary focus is patient care. Policies and technologies must be designed with usability in mind, ensuring that compliance enhances rather than obstructs workflow.
When organizations succeed in harmonizing technology with practice, they achieve sustainable compliance that endures under real-world pressures.
Cultivating Organizational Resilience
Resilience transcends compliance. It represents an organization’s ability to withstand disruptions, adapt to change, and emerge stronger. Auditing and continuous improvement serve as cornerstones of resilience, enabling institutions to anticipate threats, mitigate risks, and recover swiftly from setbacks.
Resilience also depends on culture. Employees who internalize the importance of security contribute actively to defense, reporting anomalies, and adhering to protocols even under stress. Leaders who champion compliance foster an environment where vigilance becomes second nature.
Ultimately, resilience ensures that healthcare organizations can fulfill their mission of patient care without interruption, even in the face of cyber adversity.
The Evolution of Healthcare Cybersecurity
Healthcare has always balanced two imperatives: providing compassionate care and managing vast stores of sensitive information. In the past, paper records were locked in filing cabinets, guarded by physical barriers. Today, digital networks form the nervous system of modern medicine, allowing physicians to share diagnostic images instantly, insurers to verify coverage electronically, and patients to access their records from mobile devices. Yet with this convenience comes exposure.
Cyber threats against healthcare grow more sophisticated every year. Attackers exploit zero-day vulnerabilities, leverage artificial intelligence to craft convincing phishing campaigns, and deploy ransomware capable of paralyzing entire hospital systems. While other industries face similar dangers, the stakes in healthcare are uniquely high. A delayed diagnosis or interrupted surgery caused by inaccessible records can mean the difference between life and death. This gravity underscores why continuous vigilance and structured frameworks like HIO-201 are indispensable.
Why Long-Term Strategy Matters
Short-term compliance is insufficient. An organization may pass an audit today but remain vulnerable tomorrow if it treats compliance as a box-checking exercise. Long-term strategy transforms compliance from a periodic obligation into an enduring commitment. It anticipates future threats, invests in sustainable solutions, and embeds security within the very identity of the organization.
A long-term strategy recognizes that cybercriminals evolve continuously. Yesterday’s firewall may be bypassed by tomorrow’s exploit. Therefore, healthcare organizations must adopt a mindset of perpetual adaptation. They must budget for ongoing upgrades, commit to recurring training, and remain attentive to regulatory developments. Long-term strategy also acknowledges that patient trust is cumulative; it must be earned repeatedly through consistent protection of data over time.
Institutionalizing Training as a Permanent Fixture
Training must be more than an occasional seminar. To achieve resilience, training should become a permanent fixture of organizational life. This involves scheduling recurring sessions, incorporating security awareness into onboarding, and embedding privacy considerations into professional development.
Organizations should design training programs that evolve alongside technology. For example, when mobile applications become central to patient engagement, training should address mobile security risks. When artificial intelligence systems analyze patient data, training should discuss algorithmic bias, transparency, and security of training datasets. By updating training curricula continuously, organizations ensure relevance.
The exam code HIO-201 reinforces this approach by highlighting the ongoing nature of compliance knowledge. Preparing for the examination requires engagement with current standards, but sustaining that knowledge demands continuous learning. In this sense, HIO-201 is not a destination but a compass guiding lifelong professional growth.
Leadership as the Pillar of Ethical Stewardship
Appointing security and privacy officers is only the beginning. For long-term resilience, leadership must embody ethical stewardship. Officers must be more than enforcers of rules; they must be advocates for patient dignity and guardians of trust. Their role includes influencing executive decisions, guiding technology investments, and ensuring that compliance considerations permeate organizational strategy.
Leaders also serve as role models. When staff observe leaders taking compliance seriously—adhering to access protocols, participating in training, and responding swiftly to incidents—they are more likely to emulate those behaviors. Conversely, if leaders treat compliance dismissively, the culture erodes.
Effective leaders also bridge communication gaps. Clinicians, administrators, and IT professionals often speak different professional languages. Leaders translate between these groups, ensuring that compliance measures are understood, accepted, and implemented across all departments.
The Architecture of a Living Risk Management Framework
A risk management framework must be conceived as a living architecture, not a static structure. Threats mutate, technologies advance, and organizational workflows shift. For risk management to remain relevant, it must be revisited frequently.
A living framework begins with a continuous asset inventory. Healthcare institutions must always know which devices, applications, and systems interact with protected health information. As new technologies are deployed, they must be immediately integrated into the inventory.
Next, the framework requires dynamic threat assessment. Emerging attack methods—whether ransomware variants, supply-chain compromises, or insider manipulations—must be evaluated in relation to the institution’s environment. Mitigation plans must then be updated accordingly, with responsibilities and timelines clearly defined.
Finally, the framework must integrate feedback loops from audits, incident reports, and employee observations. This feedback ensures that the framework adapts not only to external threats but also to internal realities. HIO-201 underscores this principle by framing risk management as a cyclical, continuous process rather than a single undertaking.
Policy as an Ethical Contract
Policies represent more than procedural instructions; they are ethical contracts between healthcare providers and patients. When organizations craft policies requiring encryption, access controls, or incident reporting, they are affirming their duty to safeguard patient dignity. These policies codify values into practice.
To fulfill their role as ethical contracts, policies must be accessible and comprehensible. Overly technical language may alienate non-technical staff, while vague instructions may leave room for dangerous improvisation. Clarity ensures that every employee understands their obligations.
Regular updates transform policies from brittle documents into flexible instruments. As telehealth expands, as wearable technologies proliferate, and as genomic data becomes increasingly integrated into care, policies must evolve. In doing so, they sustain their ethical promise to patients.
The Unending Relevance of Internal and External Audits
Auditing remains indispensable for ensuring that policies, training, and risk management strategies function as intended. Internal audits create a culture of accountability, ensuring that employees know their actions may be reviewed. External audits bring objectivity, introducing insights that internal teams might overlook.
Auditing also provides evidence of diligence. When regulators investigate breaches, organizations with detailed audit records can demonstrate that they acted responsibly. This evidence may mitigate penalties and protect reputations. More importantly, it reassures patients that the breach was not the result of negligence.
HIO-201 emphasizes auditing as an ongoing necessity, reminding professionals that resilience requires vigilance rather than complacency.
Incident Response as a Measure of Organizational Maturity
No matter how robust the defenses, incidents will occur. The true measure of organizational maturity is not the absence of breaches but the effectiveness of the response. Mature organizations maintain incident response plans that are practiced, documented, and continually refined.
An effective response minimizes harm, preserves patient safety, and restores operations swiftly. It also demonstrates transparency, informing patients and regulators promptly. After the crisis, a mature organization conducts post-incident reviews, identifying lessons learned and integrating them into future defenses.
In this sense, every incident becomes both a challenge and an opportunity. By responding ethically and adaptively, organizations transform adversity into progress.
Cultivating a Culture of Security-Conscious Care
Ultimately, long-term resilience depends on culture. Compliance cannot survive as a series of isolated directives. It must become woven into the daily fabric of healthcare delivery. When nurses double-check their devices for security updates, when administrators encrypt their communications instinctively, and when physicians treat privacy as inseparable from patient care, compliance becomes culture.
This cultural transformation requires relentless reinforcement. Leaders must communicate its importance repeatedly, employees must be recognized for vigilance, and training must emphasize the ethical dimensions of compliance. Culture ensures that security persists even when technologies change, regulations evolve, and new threats emerge.
The Ethical Imperative of Trust
At the core of compliance lies trust. Patients disclose their most sensitive information under the assumption that it will remain confidential. They share details of illnesses, histories, and vulnerabilities, believing that their dignity will be respected. Breaches violate this trust, causing harm that transcends financial consequences.
By embedding HIO-201 principles into long-term strategies, healthcare organizations reaffirm their ethical commitment. They signal to patients that privacy is not a negotiable commodity but a fundamental right. Trust becomes the foundation of every interaction, strengthening the bond between provider and patient.
The Future Trajectory of Healthcare Security
Looking forward, healthcare security will only grow more complex. Artificial intelligence will analyze genomic data to personalize treatments, yet it will also create new attack surfaces. Quantum computing may revolutionize encryption while simultaneously rendering current algorithms obsolete. Global networks will facilitate cross-border sharing of medical information, raising new questions about jurisdiction and privacy.
Healthcare organizations that succeed will be those that embrace adaptability. They will integrate continuous learning, agile policies, resilient risk management, and ethical leadership into their DNA. They will treat compliance not as a regulatory burden but as a moral compass guiding them through uncertainty.
The Enduring Value of HIO-201
The exam code HIO-201 stands as a symbol of structured knowledge, continuous vigilance, and professional accountability. While no single examination can solve the challenges of healthcare security, HIO-201 provides a unifying framework. It ensures that professionals across the sector share a common language, a shared understanding of principles, and a collective commitment to safeguarding PHI.
Through the discipline fostered by HIO-201, healthcare organizations build a foundation of resilience. They create a culture where compliance is not merely about avoiding penalties but about honoring patients’ trust. They prepare for the unknown, respond to the unexpected, and evolve with the times.
Conclusion
The landscape of healthcare cybersecurity is both complex and critical, demanding vigilance across technology, policies, and human behavior. Protecting patient information requires more than compliance with regulations; it calls for a holistic strategy that integrates continuous training, robust risk management, and ethical leadership. The principles embodied in HIO-201 provide a structured framework to guide professionals in safeguarding PHI, fostering consistency, and ensuring preparedness against evolving threats. Internal and external audits, combined with adaptive policies and incident response planning, reinforce organizational resilience, while embedding a culture of security-conscious care ensures that compliance is lived, not merely documented. Ultimately, healthcare organizations that embrace this multifaceted approach not only meet regulatory obligations but also uphold patient trust, honor ethical responsibilities, and cultivate long-term resilience. By aligning technology, human awareness, and governance, they create a sustainable framework capable of protecting sensitive information in a rapidly changing digital environment.
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How often do you update the questions?
Testking strives to provide you with the latest questions in every exam pool. Therefore, updates in our exams/questions will depend on the changes provided by original vendors. We update our products as soon as we know of the change introduced, and have it confirmed by our team of experts.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.


