Certification: ACSM Registered Clinical Exercise Physiologist
Certification Full Name: ACSM Registered Clinical Exercise Physiologist
Certification Provider: ACSM
Exam Code: 040-444
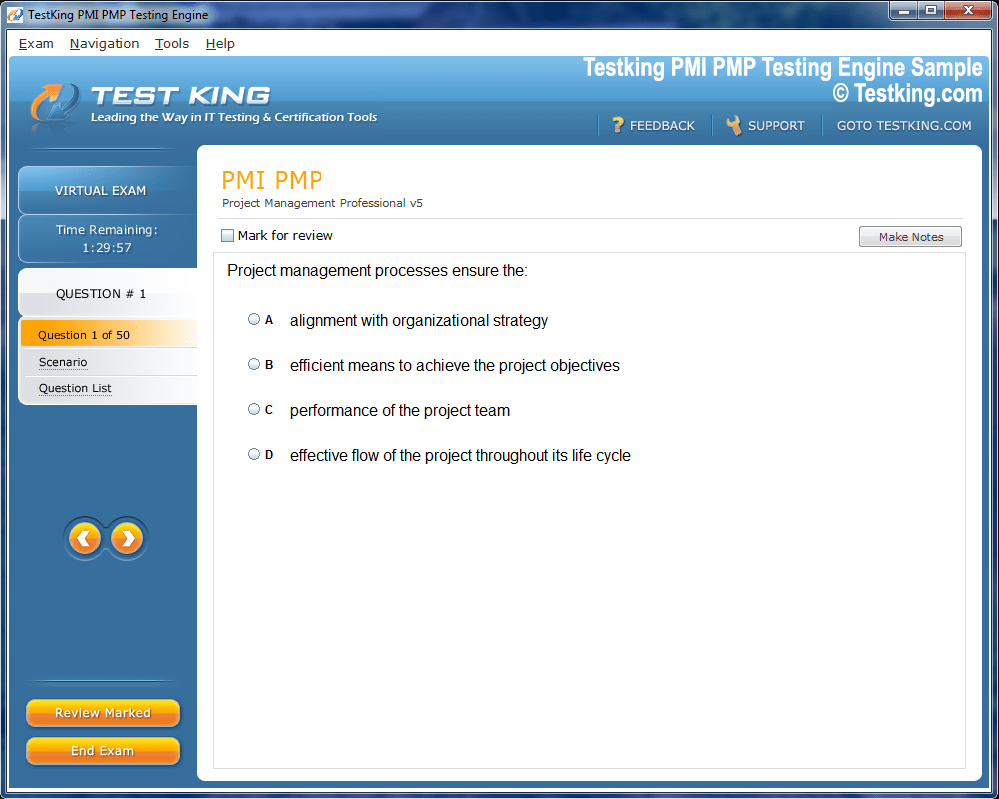
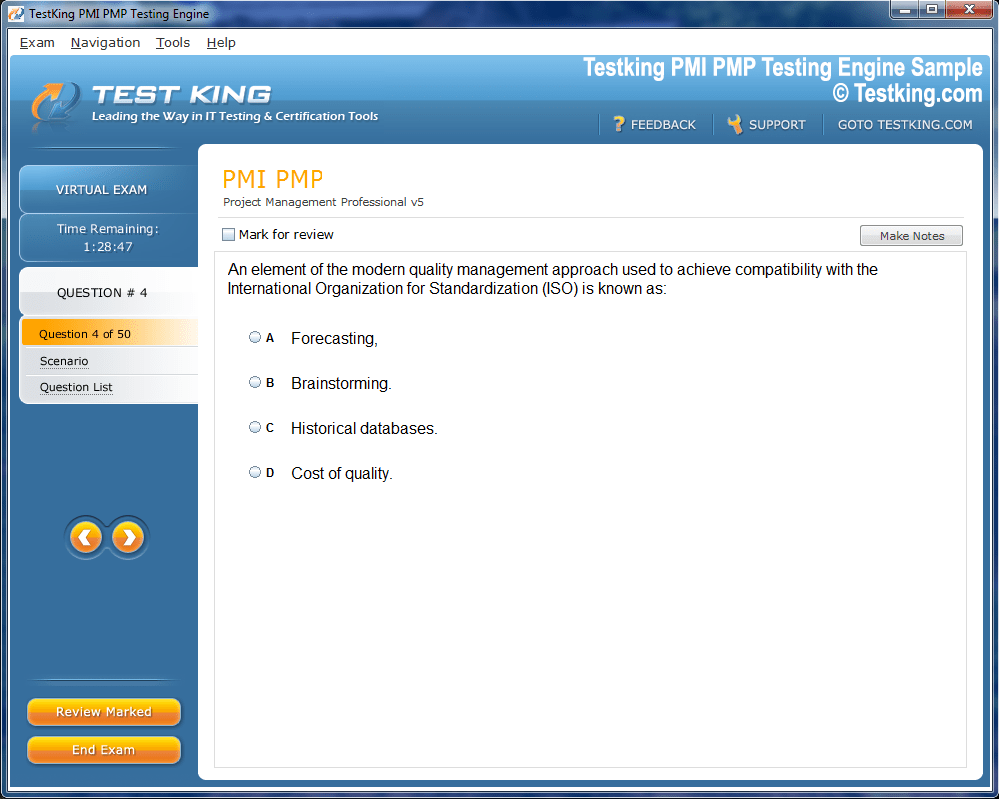
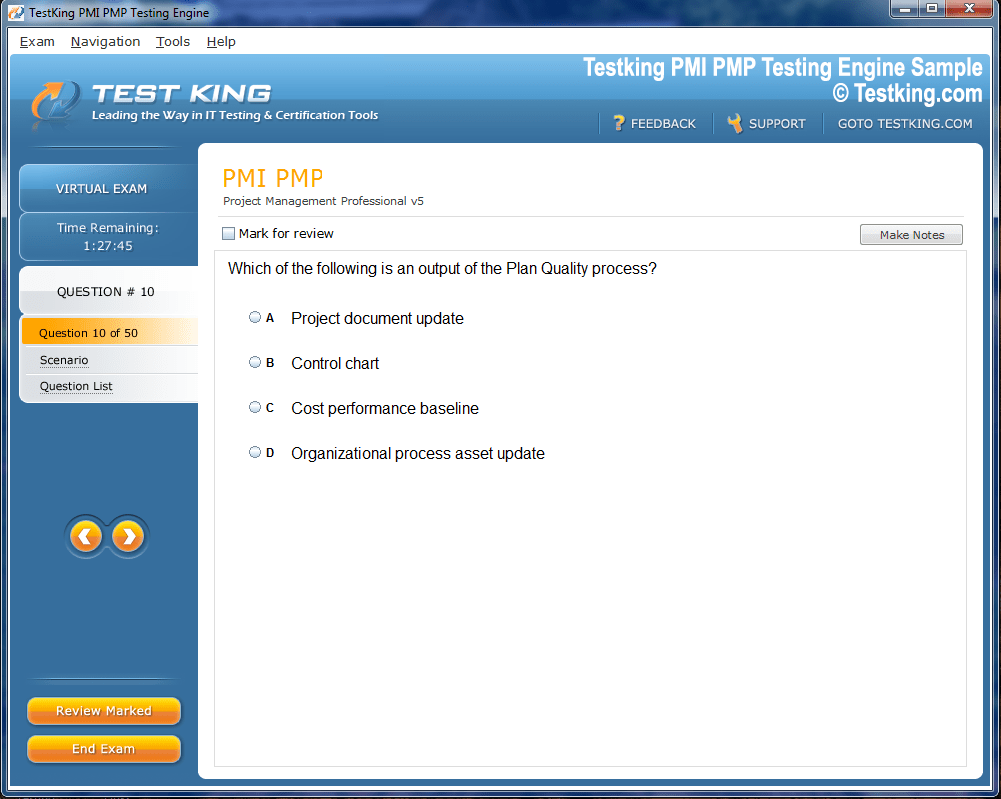
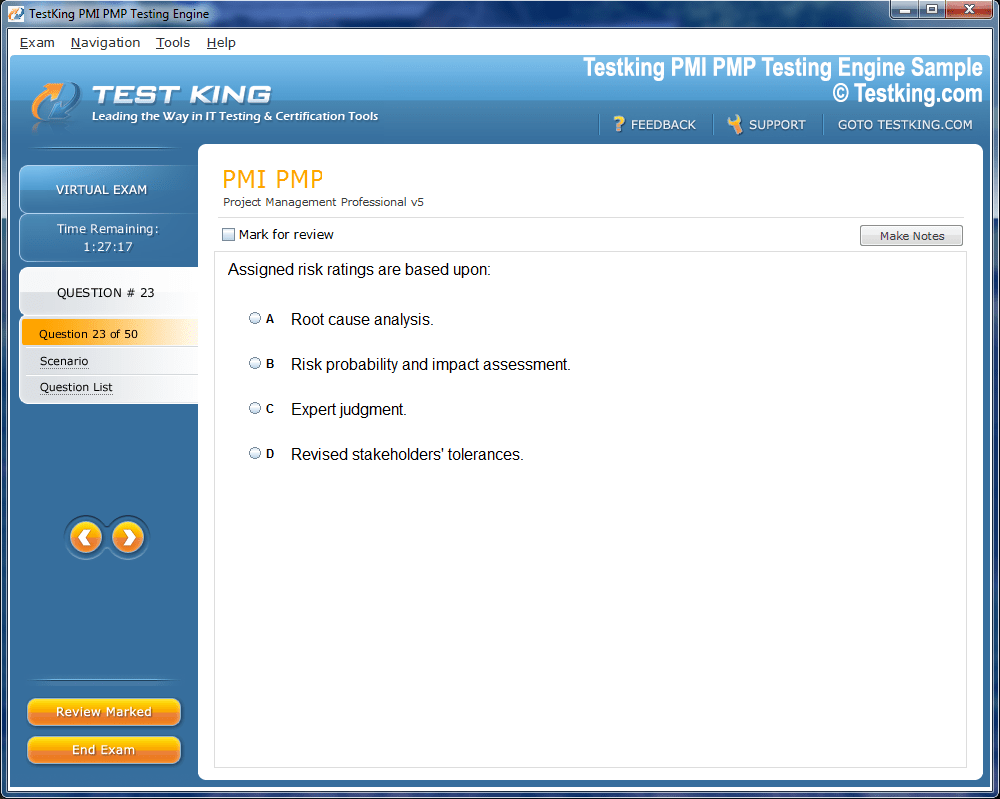
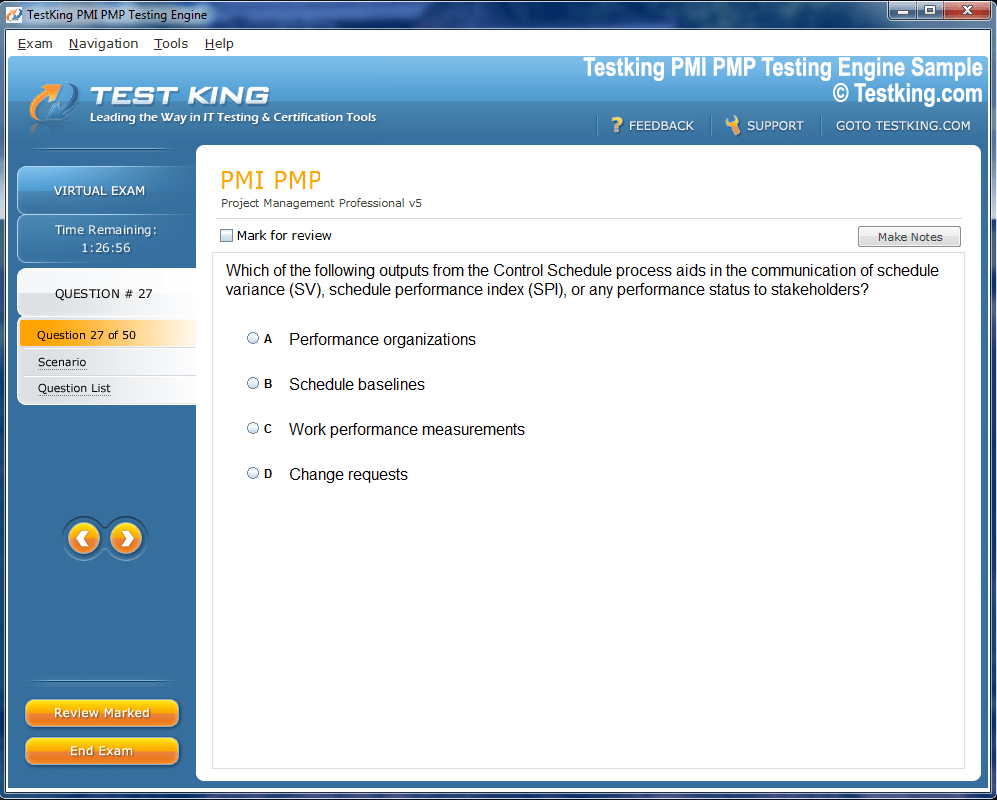
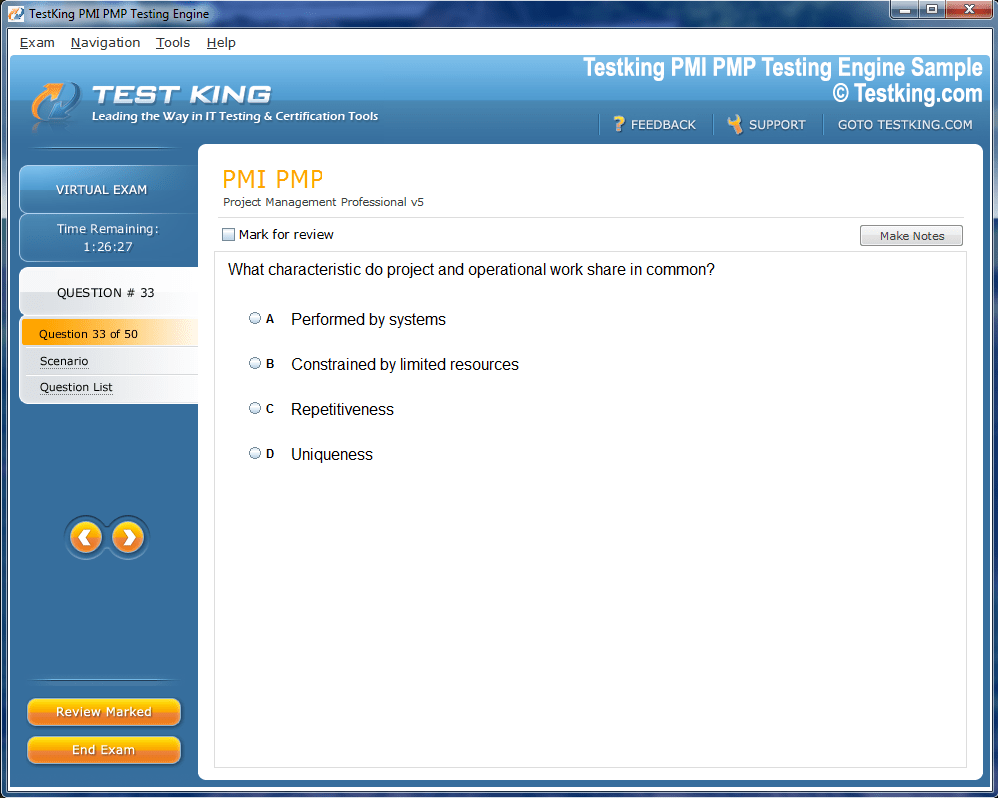
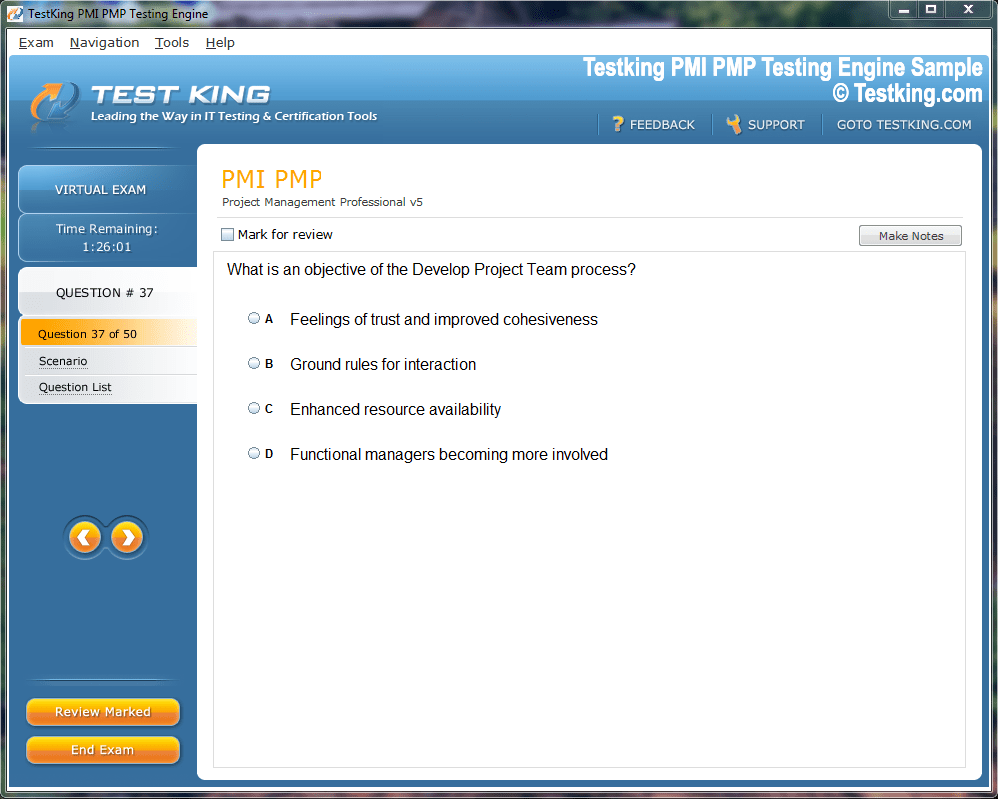
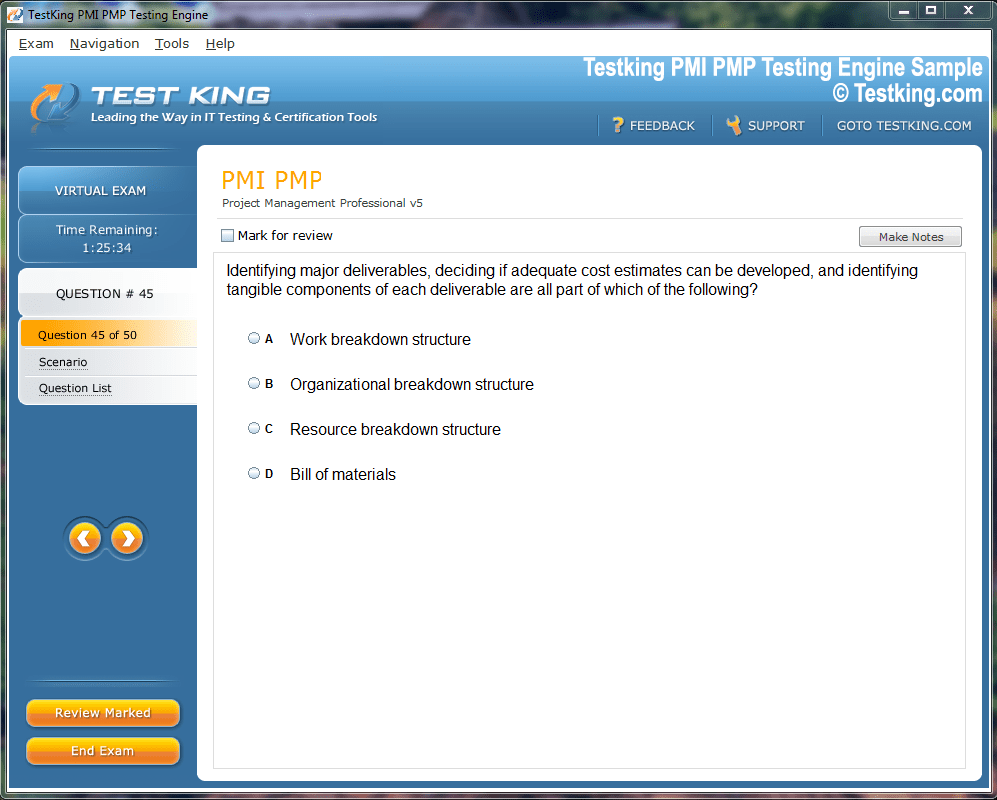
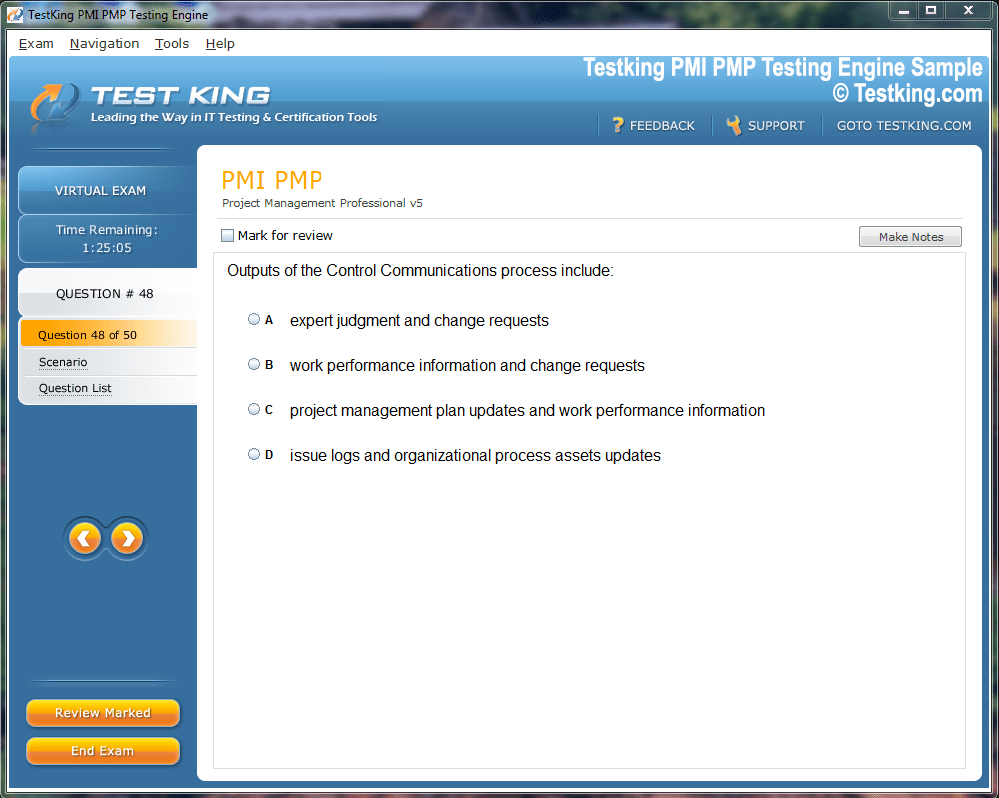
Product Screenshots

nop-1e =1
Foundations of the ACSM Registered Clinical Exercise Physiologist Certification Exam
The American College of Sports Medicine, or ACSM, stands as a premier organization in the fields of sports medicine and exercise science. It provides certifications that are widely recognized as the gold standard for health and fitness professionals. Among its most advanced credentials is the Registered Clinical Exercise Physiologist, or RCEP. This certification is specifically designed for allied health professionals who work with patients facing chronic diseases and conditions. Earning this credential signifies a high level of expertise in clinical exercise physiology, setting a professional apart in a competitive healthcare landscape. The RCEP certification exam is the gateway to this esteemed status.
The journey to becoming an ACSM RCEP involves a rigorous preparation process culminating in a comprehensive exam. This test is meticulously designed to evaluate a candidate's ability to apply scientific principles to practical, clinical scenarios. It assesses not just theoretical knowledge but also the critical thinking skills required to safely and effectively manage patients with complex health issues. Passing the RCEP exam demonstrates mastery over a specialized body of knowledge, proving that an individual is capable of providing top-tier exercise-related services within a medical setting, often as part of an interdisciplinary healthcare team.
The Role and Significance of the RCEP
A Registered Clinical Exercise Physiologist is a crucial member of the modern healthcare team. These specialists utilize exercise as a therapeutic modality to treat and manage a wide range of chronic conditions. They work with diverse patient populations, including those with cardiovascular disease, pulmonary conditions like COPD, metabolic disorders such as diabetes, and various other comorbidities. The RCEP's primary role is to develop, implement, and supervise exercise programs that are tailored to the unique physiological and psychological needs of each patient, ensuring both safety and efficacy in their treatment plans.
The significance of the RCEP lies in their ability to bridge the gap between clinical medicine and practical exercise application. While a physician may diagnose a condition and recommend physical activity, the RCEP provides the detailed, evidence-based prescription and guidance necessary for the patient to succeed. This specialized skill set helps improve patient outcomes, enhance quality of life, reduce the risk of secondary health events, and lower overall healthcare costs. The RCEP exam is designed to ensure that certified professionals possess the advanced competency required to fulfill this vital and increasingly recognized role in preventive and rehabilitative care.
Eligibility and Prerequisites for the Exam
Aspiring candidates must meet stringent eligibility requirements before they can sit for the ACSM RCEP certification exam. There are two primary pathways to qualify. The first pathway requires a master's degree in exercise science, exercise physiology, or a directly related field. In addition to the advanced degree, candidates following this route must also have accumulated at least 600 hours of hands-on clinical experience. This experience is critical, as it provides the practical context for the theoretical knowledge gained during their graduate studies, preparing them for real-world patient care scenarios they will face professionally.
The second pathway is for individuals who hold a bachelor's degree in exercise science, exercise physiology, or an equivalent field. While a master's degree is not required for this route, the clinical experience requirement is substantially higher. Candidates with a bachelor's degree must complete a minimum of 1,200 hours of practical clinical work. This extensive experience requirement ensures that these professionals have developed a deep, hands-on understanding of patient assessment, exercise testing, and prescription. Regardless of the pathway, all candidates must also hold a current Basic Life Support or CPR for the Professional Rescuer certification.
Structure and Format of the RCEP Exam
The ACSM RCEP exam is a computer-based assessment that challenges candidates with a wide array of questions. The exam is composed of approximately 125 to 150 multiple-choice questions. It is important to note that a portion of these questions are "pilot" or unscored items, which the ACSM uses to evaluate question quality for future versions of the exam. Candidates are not informed which questions are scored and which are unscored, so it is essential to answer every question to the best of one's ability. Test-takers are typically given a total of 3.5 hours to complete the entire exam.
This time allotment requires effective time management to ensure that every question can be carefully considered. The questions are not just simple recall of facts; many are scenario-based, requiring the candidate to analyze a patient case and select the most appropriate course of action. This format is intended to simulate the decision-making process that an RCEP uses in their daily practice. The exam is administered at designated testing centers, providing a standardized and secure environment for all candidates. Familiarity with this structure is a key component of a successful exam preparation strategy.
Exam Domains: An Overview
The content of the RCEP exam is organized into four distinct but interconnected domains of practice. Each domain represents a core area of competency for a clinical exercise physiologist. The first domain is Patient Assessment and Risk Stratification. This section focuses on the initial evaluation of a patient, including reviewing medical history, conducting physical exams, and interpreting clinical data to determine the individual's health status and risk level. A thorough understanding of this domain is fundamental, as all subsequent decisions about testing and exercise prescription are based on this initial assessment.
The second domain is Exercise Testing. This covers the knowledge and skills needed to select, administer, and interpret various forms of clinical exercise tests. The third domain, Exercise Prescription, deals with the development of safe, effective, and individualized exercise programs based on the findings from the assessment and testing phases. The final domain is Education and Behavior Change. This area emphasizes the RCEP's role as an educator and motivator, covering topics like patient counseling, goal setting, and strategies to promote long-term adherence to a healthy lifestyle. Each domain is weighted differently on the exam, reflecting its importance in practice.
Knowledge, Skills, and Abilities (KSAs)
The foundation of the RCEP exam is a detailed list of Knowledge, Skills, and Abilities, often referred to as KSAs. These are specific competencies that an entry-level RCEP is expected to possess. The KSAs provide a comprehensive blueprint for the exam's content. The "Knowledge" component refers to the theoretical understanding required, such as the pathophysiology of chronic diseases or the physiological responses to exercise. "Skills" refer to the practical proficiencies, like measuring blood pressure correctly or administering a graded exercise test. "Abilities" relate to the capacity to synthesize knowledge and skills to make sound clinical judgments.
Prospective candidates should use the official ACSM list of KSAs as a primary study guide. By systematically reviewing each KSA, a candidate can identify their personal areas of strength and weakness. This allows for a more targeted and efficient study plan. The KSAs cover everything from understanding electrocardiography and pharmacology to applying behavioral theories and managing emergencies. A deep familiarity with these competencies is not just crucial for passing the exam but is also essential for providing safe and competent care as a practicing Registered Clinical Exercise Physiologist.
Initial Study Strategies and Resources
Beginning the preparation for the ACSM RCEP exam requires a structured and strategic approach. The first step should be to download the official exam content outline and the detailed KSAs from the ACSM. This document is the roadmap for your studies. After a thorough review, create a realistic study schedule that allocates sufficient time to each domain based on its weight on the exam and your personal confidence level with the material. It is often beneficial to start studying several months in advance to avoid cramming and to allow for deeper comprehension of complex topics.
A variety of resources can be utilized to prepare for the exam. The primary texts recommended by ACSM, such as "ACSM's Guidelines for Exercise Testing and Prescription," are indispensable. These books provide the foundational knowledge for the majority of the exam questions. Additionally, consider enrolling in an RCEP exam preparation workshop or online course. These programs often provide structured reviews, practice questions, and insights from experienced instructors. Forming a study group with peers can also be highly beneficial, allowing for collaborative learning and discussion of challenging concepts.
Interpreting Laboratory and Diagnostic Test Results
The RCEP exam heavily emphasizes the ability to interpret data from common laboratory and diagnostic tests. Clinical Exercise Physiologists are not expected to diagnose conditions from these results, but they must be able to recognize normal versus abnormal values and understand their implications for exercise. This includes analyzing results from a complete blood count, a basic metabolic panel, and a lipid panel. For example, recognizing an abnormally low hemoglobin level might indicate anemia, which would significantly impact a patient's exercise tolerance and necessitate modifications to their exercise test protocol.
Furthermore, candidates must be familiar with the results of key cardiometabolic and pulmonary diagnostic procedures. This involves interpreting findings from an electrocardiogram (ECG) at rest, understanding the basics of echocardiogram reports, analyzing results from pulmonary function tests like spirometry, and recognizing the significance of vascular imaging studies. Questions on the exam will likely present a patient case with a set of lab values or test results and ask the candidate to determine the appropriate next step regarding exercise testing or prescription based on that data.
The Clinical Physical Examination
While the RCEP does not perform a full diagnostic physical exam like a physician, they are responsible for conducting a focused, pre-participation physical examination. This assessment is crucial for ensuring the patient is stable and safe to begin an exercise test or program. The exam will test your knowledge of the key components of this evaluation. This includes accurately measuring vital signs such as resting heart rate and blood pressure, following proper protocols and using correct cuff sizes. It also involves assessing the pulmonary system by observing breathing patterns and auscultating for abnormal breath sounds.
The cardiovascular assessment includes palpating peripheral pulses for rate, rhythm, and quality, and checking for peripheral edema. A basic musculoskeletal evaluation is also necessary to identify any orthopedic limitations or abnormalities that might affect the patient's ability to exercise safely or require modifications to the chosen modality. The RCEP must be able to recognize "red flag" findings during this examination, such as a resting systolic blood pressure over 200 mmHg or signs of respiratory distress, which would be absolute contraindications to proceeding with exercise testing.
ACSM Preparticipation Screening and Risk Stratification
A cornerstone of the first domain on the RCEP exam is the ACSM's preparticipation health screening algorithm. Candidates must have this process memorized and be able to apply it flawlessly to various patient scenarios. The algorithm is designed to identify individuals who may be at a higher risk for adverse cardiovascular events during exercise. It guides the decision-making process regarding the need for medical clearance from a physician before the individual begins an exercise program or undergoes an exercise test. This systematic approach is critical for ensuring patient safety.
The algorithm uses a logical sequence of questions based on the individual's current level of physical activity, the presence of known cardiovascular, metabolic, or renal disease, and the presence of major signs or symptoms suggestive of these diseases. Based on the answers, the individual is categorized, and a recommendation is made. Risk stratification goes beyond this initial screening, involving a deeper analysis of all collected data—history, exam findings, and lab results—to classify a patient as low, moderate, or high risk, which in turn influences the level of supervision required during exercise.
Indications and Contraindications for Exercise Testing
Before any exercise test is performed, the RCEP must determine if it is appropriate and safe for the patient. The RCEP exam will test your knowledge of the specific indications and contraindications for exercise testing. Indications are the reasons for performing the test. For a clinical population, the primary indications often include diagnostic purposes (to identify the presence of coronary artery disease), prognostic purposes (to assess the severity of a known disease and predict future events), and therapeutic purposes (to evaluate the effectiveness of an intervention or to develop an exercise prescription).
Equally important is the knowledge of contraindications, which are conditions or factors that make the test unsafe to perform. These are categorized as either absolute or relative. Absolute contraindications are situations where the risk of performing the test outweighs any potential benefit, and the test should not be conducted under any circumstances. Examples include an acute myocardial infarction within two days or unstable angina. Relative contraindications are conditions where the test may be performed if the potential benefit outweighs the risk, but it should be done with caution, often with a physician present.
Principles of Exercise Test Selection
Selecting the appropriate exercise test is a critical decision that depends entirely on the information gathered during the initial patient assessment. The RCEP exam will challenge your ability to choose the most suitable test based on a patient's clinical status, their goals for testing, and their physical limitations. There is no one-size-fits-all protocol. The selection process involves considering the primary question the test is meant to answer. Is it for diagnostic purposes in a patient with suspected coronary artery disease, or is it for functional capacity assessment in a patient entering cardiac rehabilitation?
Furthermore, the choice of modality—such as a treadmill, cycle ergometer, or arm ergometer—is a key consideration. A treadmill test, which involves walking, is often preferred as it is a familiar, weight-bearing activity for most people. However, for a patient with severe osteoarthritis of the knees or balance issues, a cycle ergometer would be a safer and more appropriate choice. The exam will present case scenarios requiring you to justify your selection of a specific test protocol and modality based on the patient's unique clinical profile.
Common Exercise Testing Protocols
A thorough knowledge of various graded exercise test (GXT) protocols is fundamental for the RCEP exam. You must be familiar with the specifics of the most commonly used protocols, including the Bruce, modified Bruce, Naughton, and Balke-Ware treadmill protocols, as well as the Astrand and YMCA cycle ergometer protocols. This familiarity needs to go beyond just knowing the names. You must understand the workload progressions for each stage, including the speed, grade, or resistance changes, and the duration of each stage.
The key is to understand which protocol is best for which population. The standard Bruce protocol, with its large and rapid increases in workload, is suitable for physically active, younger individuals but is often too aggressive for deconditioned patients or older adults. In those cases, a modified Bruce or a Naughton protocol, which starts at a lower intensity and has smaller increments, would be more appropriate. The ability to match the protocol to the patient's estimated functional capacity is a skill that demonstrates clinical competence and is frequently evaluated on the exam.
Monitoring During Exercise Testing
Continuous and careful monitoring of the patient throughout the exercise test is paramount for safety and for gathering accurate data. The RCEP exam requires a comprehensive understanding of what to monitor, when to monitor it, and how to interpret the findings in real-time. Key physiological variables that must be tracked include heart rate, blood pressure, the 12-lead ECG, and the patient's subjective ratings of perceived exertion (RPE) and clinical symptoms, such as chest pain (angina) or shortness of breath (dyspnea).
Measurements should be taken at rest, during the last minute of each stage of the GXT, at peak exercise, and for several minutes into recovery. You must be proficient in recognizing normal and abnormal responses to exercise. A normal response includes a linear increase in heart rate and systolic blood pressure with increasing workload, while diastolic blood pressure should remain relatively stable. The exam will test your ability to identify abnormal responses, such as a drop in systolic blood pressure with increasing workload, which could signify a serious underlying issue.
ECG Interpretation During Exercise
For the RCEP, interpreting the electrocardiogram (ECG) before, during, and after exercise is one of the most critical skills. While the formal diagnosis is made by a physician, the RCEP must be able to identify significant ECG changes that may indicate myocardial ischemia or an arrhythmia, as these findings are often key indicators for stopping a test. The exam will expect you to have a strong foundation in basic ECG interpretation, including identifying different waves and intervals, calculating heart rate, and determining the cardiac axis.
The primary focus during exercise testing is on monitoring for ST-segment depression or elevation, which can be indicative of ischemia. You must know the criteria for a "positive" or abnormal test, such as ≥1.0 mm of horizontal or downsloping ST-segment depression. Additionally, you must be able to recognize common exercise-induced arrhythmias, both benign (like isolated PVCs) and potentially life-threatening (like ventricular tachycardia), and know the appropriate course of action for each. ECG interpretation is a high-level skill that distinguishes the clinical professional.
Gas Exchange and Ventilatory Responses
While not performed in all clinical settings, the direct measurement of gas exchange during a cardiopulmonary exercise test (CPX or CPET) provides the most accurate assessment of cardiorespiratory fitness (CRF). The RCEP exam requires knowledge of the key variables obtained from a CPX, including oxygen uptake (VO2), carbon dioxide production (VCO2), respiratory exchange ratio (RER), and the ventilatory or anaerobic threshold. VO2max, or peak VO2, is considered the gold standard measure of CRF and is a powerful prognostic indicator in many clinical populations.
You must understand the normal physiological responses of these variables to progressive exercise. For instance, VO2 increases linearly with workload until its maximum is reached. The RER, which is the ratio of VCO2 to VO2, typically starts around 0.8 at rest and increases to 1.0 and beyond at peak exercise. A particularly important concept is the ventilatory threshold, the point at which ventilation begins to increase disproportionately to the increase in oxygen uptake. This marker is often used to prescribe exercise intensity and is a key data point to identify from CPX results on the exam.
Test Termination Criteria
Knowing when to stop an exercise test is arguably the most important safety consideration. The ACSM provides clear guidelines on absolute and relative indications for terminating a GXT, and mastery of these criteria is non-negotiable for the RCEP exam. Absolute indications are signs and symptoms that mandate the immediate cessation of the test. These include a drop in systolic blood pressure of >10 mmHg from baseline despite an increase in workload, moderate to severe angina, signs of poor perfusion like dizziness or pallor, and sustained ventricular tachycardia.
Relative indications are less critical but should be used to weigh the risks and benefits of continuing the test. These might include marked ST displacement or increasing chest pain. In addition to these clinical signs, the test is also terminated when the patient reaches their volitional fatigue and requests to stop, or when they achieve a predetermined endpoint. The exam will present scenarios where you must analyze a set of changing clinical variables and decide if the test should be stopped, applying these established criteria correctly.
The FITT-VP Principle of Exercise Prescription
The foundation of any sound exercise prescription is the FITT-VP principle, a framework that is central to the RCEP exam. This acronym stands for Frequency, Intensity, Time, Type, Volume, and Progression. Each component must be carefully considered to create a plan that is safe, effective, and tailored to the individual patient. Frequency refers to how often the exercise is performed, typically expressed in days per week. Intensity describes how hard the patient should be working, which can be prescribed using various methods like heart rate reserve, VO2 reserve, or the rating of perceived exertion (RPE) scale.
Time refers to the duration of each exercise session. Type specifies the mode of exercise, such as walking, cycling, or swimming. Volume is the total amount of exercise performed, often calculated as the product of frequency, intensity, and time, and expressed in MET-minutes or kilocalories per week. Finally, Progression outlines how the exercise program should be advanced over time as the patient's fitness level improves. The exam will require you to apply this principle to design comprehensive exercise prescriptions for various clinical scenarios.
Prescribing Exercise Intensity
Determining the appropriate exercise intensity is one of the most critical aspects of the prescription, and the RCEP exam places significant emphasis on this topic. There are several methods for prescribing intensity, and the RCEP must be proficient in all of them. The heart rate reserve (HRR) method, also known as the Karvonen method, is a very common approach. It uses a percentage of the difference between maximal heart rate and resting heart rate to establish a target heart rate range. The peak oxygen uptake (VO2) reserve method is conceptually similar and is considered a gold standard when data from a gas exchange test is available.
Other methods include using a direct percentage of the patient's measured maximal heart rate or peak VO2. For patients on certain medications like beta-blockers that blunt the heart rate response, or for those who have difficulty monitoring their pulse, the Rating of Perceived Exertion (RPE) scale is an invaluable tool. The RCEP must be able to select the most appropriate method based on the patient's condition, medications, and available data, and be able to perform the necessary calculations accurately for the exam.
Exercise Prescription for Cardiac Patients
Developing exercise prescriptions for patients with cardiovascular disease, such as those in a cardiac rehabilitation program, is a core competency for an RCEP. The exam will test your knowledge of specific guidelines for this population. For patients post-myocardial infarction or coronary artery bypass surgery, the initial exercise prescription is typically conservative, focusing on low-intensity aerobic activity like walking. The intensity is often guided by the results of a recent exercise test, with a heart rate target set safely below the ischemic or arrhythmic threshold.
The prescription must also consider the patient's medications. For example, beta-blockers lower the heart rate at rest and during exercise, so target heart rates must be adjusted accordingly or an RPE scale used instead. Resistance training is also a crucial component for cardiac patients but should generally be initiated after a period of consistent aerobic training. The RCEP must know the proper protocols, including starting with light weights and emphasizing proper breathing techniques to avoid an excessive blood pressure response.
Exercise Prescription for Pulmonary Patients
Patients with chronic pulmonary diseases, such as Chronic Obstructive Pulmonary Disease (COPD), present unique challenges that will be addressed on the RCEP exam. The primary limiting symptom for these patients is often dyspnea, or shortness of breath, rather than cardiovascular limitations. Therefore, exercise intensity is most effectively prescribed and monitored using the Borg CR10 dyspnea scale rather than heart rate. Patients are typically instructed to exercise at a dyspnea level of 3 to 5 on a 0-10 scale.
The exercise prescription for pulmonary patients often includes a combination of aerobic exercise, resistance training, and flexibility. Aerobic exercise, such as walking or stationary cycling, helps improve cardiovascular endurance and reduce ventilatory demand at submaximal workloads. Resistance training is particularly important for addressing the peripheral muscle weakness and atrophy that is common in this population. Additionally, training of the inspiratory muscles may be included to improve breathing efficiency and reduce dyspnea, a specialized intervention the RCEP should be familiar with.
Exercise Prescription for Metabolic Disease
The RCEP exam will require a detailed understanding of exercise prescription for individuals with metabolic diseases, most notably type 1 and type 2 diabetes. For these patients, exercise is a critical tool for improving glycemic control, enhancing insulin sensitivity, and reducing cardiovascular risk factors. A key consideration is the timing of exercise in relation to meals and medication, particularly insulin, to avoid hypoglycemia (low blood sugar). Blood glucose levels should be monitored before, during, and after exercise, especially when beginning a new program.
The general prescription for patients with diabetes includes at least 150 minutes per week of moderate-intensity aerobic exercise, spread over at least three days with no more than two consecutive days without activity. Resistance training is also highly recommended at least twice a week, as it has been shown to significantly improve glycemic control. The RCEP must be aware of the potential complications of diabetes, such as peripheral neuropathy and retinopathy, and know how to modify the exercise prescription to accommodate these conditions safely.
Theories of Health Behavior Change
Moving into the fourth domain, the RCEP exam assesses your knowledge of foundational theories that explain how people change health-related behaviors. It is not enough to simply provide a patient with an exercise prescription; the RCEP must also be an effective coach who can facilitate long-term adherence. Understanding theories like the Transtheoretical Model (TTM) is crucial. The TTM posits that individuals move through five stages of change: precontemplation, contemplation, preparation, action, and maintenance. The strategies used to help a patient will differ depending on their current stage.
Another key theory is Social Cognitive Theory, which emphasizes the concept of self-efficacy—an individual's belief in their own ability to succeed. RCEPs can help build a patient's self-efficacy through strategies like setting small, achievable goals (mastery experiences) and providing encouragement (verbal persuasion). The exam will expect you to be able to identify a patient's stage of change or level of self-efficacy from a case description and select the most appropriate theoretical strategy to apply.
Motivational Interviewing and Goal Setting
Motivational Interviewing (MI) is a specific counseling technique that is highly relevant to the RCEP's role and is a likely topic on the exam. It is a collaborative, patient-centered communication style designed to strengthen a person's own motivation for and commitment to change. Instead of telling the patient what to do, the RCEP uses MI to explore and resolve the patient's ambivalence about changing their behavior. Key techniques include asking open-ended questions, practicing reflective listening, affirming the patient's strengths, and summarizing their thoughts.
Closely linked to MI is the process of collaborative goal setting. Goals are most effective when they are developed in partnership with the patient, not prescribed to them. The exam will test your knowledge of the SMART goal framework. Goals should be Specific, Measurable, Achievable, Relevant, and Time-bound. For example, instead of a vague goal like "exercise more," a SMART goal would be "I will walk on the treadmill at a moderate pace for 30 minutes, three days per week, for the next two weeks."
Strategies to Promote Program Adherence
Even with the best prescription and initial motivation, many patients struggle with long-term adherence to their exercise programs. The RCEP exam will assess your understanding of practical strategies to help patients overcome common barriers and stick with their plans. One of the most effective approaches is to help the patient identify and solve their personal barriers to exercise, which could include lack of time, lack of social support, or fear of injury. Brainstorming solutions with the patient empowers them and increases their sense of control.
Other important strategies include encouraging patients to use self-monitoring tools like an activity log or a wearable fitness tracker, which can increase awareness and provide a sense of accomplishment. Helping the patient build a strong social support network, either with family and friends or through group-based exercise programs, is also a powerful tool. Variety in the exercise program can help prevent boredom. The ability to apply these behavioral strategies is a key part of the RCEP's multifaceted skill set.
Utilizing Practice Exams Effectively
Taking practice exams is one of the most valuable activities in your final preparation phase. The goal of using practice tests is twofold. First, they help you to assess your knowledge and identify any remaining gaps that need to be filled. When you get a question wrong, do not just look at the right answer. Take the time to understand why your choice was incorrect and why the correct answer is the best option. This deepens your comprehension and helps prevent you from making the same mistake on the actual exam.
Second, practice exams help you to hone your test-taking skills. Time yourself under realistic conditions to get a feel for the pacing required to complete the 125-150 questions in the allotted 3.5 hours. This will help you develop a time management strategy, such as deciding how long to spend on each question before moving on. It also helps you become familiar with the format and style of multiple-choice questions, reducing anxiety and building confidence for the real exam day.
Advanced Study and Memorization Techniques
To master the vast amount of information required for the RCEP exam, you may need to employ some advanced study techniques. For memorizing specific facts, such as the criteria for cardiovascular risk factors or the absolute contraindications for exercise testing, flashcards can be very effective. You can create physical cards or use a digital flashcard application. The act of creating the cards itself is a powerful learning tool, and the process of active recall when reviewing them strengthens memory retention far more than passive reading.
For more complex topics, like the pathophysiology of different diseases or the mechanisms of action for various medications, try the "teach-back" method. Explain the concept out loud to a study partner, a family member, or even just to yourself. If you can explain it clearly and accurately to someone else, it is a strong indicator that you have a solid grasp of the material. This method forces you to organize your thoughts and identify areas where your understanding is still fuzzy, making it an excellent tool for exam preparation.
Managing Test Day Anxiety and Logistics
Your performance on the RCEP exam can be influenced by your mental and physical state on the day of the test. It is crucial to manage test-day anxiety and take care of the logistics in advance. The week before the exam, focus on getting adequate sleep, eating nutritious meals, and engaging in light physical activity or relaxation techniques like deep breathing or meditation. Avoid intense, last-minute cramming, as this often increases anxiety and is less effective than consistent review. Trust in the preparation you have done over the preceding months.
On the day before the exam, confirm the location of the testing center and plan your transportation. Pack everything you need, such as your identification and any other permitted items. Aim to arrive at the testing center early to avoid any stress related to being late. During the exam, if you start to feel anxious, take a few moments to close your eyes and take some slow, deep breaths to reset your focus. A calm and clear mind is your best asset during a challenging exam.
Strategies for Answering Exam Questions
When you begin the exam, it is important to have a clear strategy for tackling the questions. First, read each question and all of the possible answers carefully before making a selection. Pay close attention to keywords like "most," "best," "except," or "not," as these can completely change the meaning of the question. For scenario-based questions, read the patient case details thoroughly and try to form a clinical picture in your mind before looking at the options.
If you encounter a difficult question, do not spend too much time on it. Use the process of elimination to narrow down the choices. If you are still unsure, make your best educated guess, flag the question for review, and move on. You can return to flagged questions at the end if you have time remaining. It is better to answer all the questions, even with some uncertainty, than to run out of time and leave questions blank. Pacing yourself and maintaining your focus are key to navigating the exam successfully.
After the Exam: Certification and Renewal
After you have completed the exam, you will typically receive your results at the testing center. Upon passing, you officially earn the prestigious title of ACSM Registered Clinical Exercise Physiologist. However, the journey of professional development does not end there. To maintain your RCEP certification, you are required to participate in continuing education. This involves accumulating a specific number of Continuing Education Credits, or CECs, over a set period.
The continuing education requirement ensures that RCEPs stay current with the latest research, guidelines, and best practices in the rapidly evolving field of clinical exercise physiology. CECs can be earned through a variety of activities, such as attending professional conferences, completing online courses, publishing research, or obtaining other related certifications. This commitment to lifelong learning is a hallmark of a true healthcare professional and is essential for providing the highest quality of care to patients throughout your career.
Career Pathways for the RCEP
Earning the RCEP certification opens the door to a wide range of rewarding career opportunities within the healthcare sector. The most common setting for RCEPs is in hospital-based cardiac and pulmonary rehabilitation programs. In this role, they work directly with patients who are recovering from heart attacks, heart surgery, or who are managing chronic lung disease. They are responsible for all aspects of the patient's exercise therapy, from initial assessment to ongoing program management and education.
Beyond traditional rehabilitation, RCEPs are increasingly finding roles in other clinical settings. This includes medically supervised weight management programs, diabetes and endocrinology clinics, cancer rehabilitation centers, and peripheral artery disease programs. Some RCEPs work in clinical research, helping to conduct studies that advance our understanding of the role of exercise in health and disease. Others may pursue opportunities in private practice, corporate wellness, or academia, teaching the next generation of exercise science professionals. The RCEP certification provides a strong foundation for a diverse and impactful career.
Scope of Practice and Professional Responsibilities
As an advanced allied health professional, the RCEP has a clearly defined scope of practice. They are experts in using exercise to manage chronic disease but must always work within the boundaries of their professional competence and in collaboration with physicians and other healthcare providers. The RCEP is qualified to receive referrals from physicians, conduct comprehensive patient assessments, supervise clinical exercise tests, and independently prescribe and lead exercise programs for patients with complex health conditions.
This advanced role comes with significant professional responsibilities. The RCEP is ethically bound to prioritize patient safety and well-being above all else. This includes maintaining patient confidentiality, adhering to evidence-based practice guidelines, and recognizing situations that are beyond their scope of practice and require referral to another healthcare professional. Upholding these high standards of conduct is essential for maintaining the integrity of the profession and the trust of patients and medical colleagues. Passing the exam is the first step in a career dedicated to these principles.
Conclusion
The journey to becoming an ACSM Registered Clinical Exercise Physiologist is a demanding yet profoundly rewarding endeavor, culminating in a rigorous certification exam that validates an exceptional level of expertise. This five-part series has navigated the intricate landscape of the RCEP credential, from the foundational knowledge required for the exam to the practical application of skills in a clinical setting. We began by establishing the significance of the RCEP as a specialized allied health professional who expertly wields exercise as a therapeutic tool for individuals with chronic diseases. This role is not merely about fitness; it is about integrating the science of exercise physiology into the art of patient care, bridging a critical gap within the healthcare continuum.
The stringent eligibility requirements, demanding both advanced academic preparation and extensive hands-on clinical experience, underscore the high standards to which this profession is held.
Our exploration delved deep into the core domains of the RCEP exam, starting with the bedrock of all clinical practice: Patient Assessment and Risk Stratification. We emphasized that before any exercise is prescribed, a meticulous process of gathering history, performing a physical evaluation, and interpreting complex clinical data must occur. The mastery of the ACSM preparticipation screening algorithm and the ability to stratify patients based on their risk profile are non-negotiable skills that ensure patient safety, the foremost responsibility of every RCEP. This initial domain sets the stage for every subsequent clinical decision, making it a critical area of focus for any exam candidate. It is the analytical starting point from which all effective and safe exercise interventions originate.
Next, we navigated the technical and interpretive challenges of the second domain, Exercise Testing. This section highlighted the RCEP’s proficiency in selecting, administering, and interpreting a variety of graded exercise tests. From calibrating equipment to monitoring a patient's hemodynamic and electrocardiographic responses, the RCEP must be a vigilant and knowledgeable practitioner. The ability to recognize subtle, abnormal responses to exercise, particularly on an ECG, and to apply established test termination criteria decisively, is a skill that can be life-saving. This domain tests not just procedural knowledge but also the capacity for real-time clinical judgment under pressure, a true test of a competent clinical exercise physiologist.
The heart of the RCEP's therapeutic role was covered in our discussion of the third and fourth domains: Exercise Prescription and Education and Behavior Change. Here, scientific knowledge is translated into a tangible, individualized plan of action for the patient. A deep understanding of the FITT-VP principle, tailored specifically to the unique pathophysiology of cardiac, pulmonary, and metabolic diseases, is paramount. However, the most scientifically perfect exercise prescription is useless if the patient does not adhere to it. Therefore, the RCEP must also be a masterful coach, skilled in behavioral change theories, motivational interviewing, and collaborative goal setting.
This dual focus on both the "what" and the "how" of exercise intervention is what makes the RCEP so effective in fostering lasting, positive health outcomes. Finally, we addressed the crucial endgame: final exam preparation and the career that follows. Success on the RCEP exam is not a matter of chance but the result of a structured, strategic, and disciplined approach to studying. Utilizing practice exams, managing test-day anxiety, and understanding the nuances of the exam questions are all part of a comprehensive strategy. Passing this challenging exam is a significant milestone that unlocks a diverse array of career paths within clinical and rehabilitative medicine. It signifies entry into a respected profession, one that carries the immense responsibility of upholding a defined scope of practice and a commitment to lifelong learning. The RCEP is more than a certification; it is a promise of excellence, a dedication to evidence-based practice, and a commitment to improving the lives of patients facing the challenges of chronic disease.
Frequently Asked Questions
Where can I download my products after I have completed the purchase?
Your products are available immediately after you have made the payment. You can download them from your Member's Area. Right after your purchase has been confirmed, the website will transfer you to Member's Area. All you will have to do is login and download the products you have purchased to your computer.
How long will my product be valid?
All Testking products are valid for 90 days from the date of purchase. These 90 days also cover updates that may come in during this time. This includes new questions, updates and changes by our editing team and more. These updates will be automatically downloaded to computer to make sure that you get the most updated version of your exam preparation materials.
How can I renew my products after the expiry date? Or do I need to purchase it again?
When your product expires after the 90 days, you don't need to purchase it again. Instead, you should head to your Member's Area, where there is an option of renewing your products with a 30% discount.
Please keep in mind that you need to renew your product to continue using it after the expiry date.
How often do you update the questions?
Testking strives to provide you with the latest questions in every exam pool. Therefore, updates in our exams/questions will depend on the changes provided by original vendors. We update our products as soon as we know of the change introduced, and have it confirmed by our team of experts.
How many computers I can download Testking software on?
You can download your Testking products on the maximum number of 2 (two) computers/devices. To use the software on more than 2 machines, you need to purchase an additional subscription which can be easily done on the website. Please email support@testking.com if you need to use more than 5 (five) computers.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by all modern Windows editions, Android and iPhone/iPad versions. Mac and IOS versions of the software are now being developed. Please stay tuned for updates if you're interested in Mac and IOS versions of Testking software.


